
Am Fam Physician. 2009;80(5):470-476
Author disclosure: Nothing to disclose.
Biceps tendinitis is inflammation of the tendon around the long head of the biceps muscle. Biceps tendinosis is caused by degeneration of the tendon from athletics requiring overhead motion or from the normal aging process. Inflam-mation of the biceps tendon in the bicipital groove, which is known as primary biceps tendinitis, occurs in 5 percent of patients with biceps tendinitis. Biceps tendinitis and tendinosis are commonly accompanied by rotator cuff tears or SLAP (superior labrum anterior to posterior) lesions. Patients with biceps tendinitis or tendinosis usually complain of a deep, throbbing ache in the anterior shoulder. Repetitive overhead motion of the arm initiates or exacerbates the symptoms. The most common isolated clinical finding in biceps tendinitis is bicipital groove point tenderness with the arm in 10 degrees of internal rotation. Local anesthetic injections into the biceps tendon sheath may be therapeutic and diagnostic. Ultrasonography is preferred for visualizing the overall tendon, whereas magnetic resonance imaging or computed tomography arthrography is preferred for visualizing the intraarticular tendon and related pathology. Conservative management of biceps tendinitis consists of rest, ice, oral analgesics, physical therapy, or corticosteroid injections into the biceps tendon sheath. Surgery should be considered if conservative measures fail after three months, or if there is severe damage to the biceps tendon.
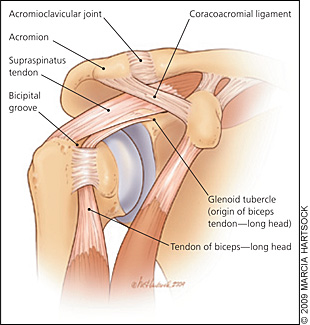
Biceps tendinitis is a disorder of the tendon around the long head of the biceps muscle. Inflammation of the biceps tendon within the intertubercular (bicipital) groove is called primary biceps tendinitis, which occurs in 5 percent of patients with biceps tendinitis.1 The 95 percent of patients without primary biceps tendinitis usually have an accompanying rotator cuff tear or a tear of the superior labrum anterior to posterior, known as a SLAP lesion. Pathology of the biceps tendon is most often found in patients 18 to 35 years of age who are involved in sports, including throwing and contact sports, swimming, gymnastics, and martial arts. These patients often have secondary impingement of the biceps tendon, which may be caused by scapular instability, shoulder ligamentous instability, anterior capsule laxity, or posterior capsule tightness. Secondary impingement may also be caused by soft tissue labral tears or rotator cuff tears that expose the biceps tendon to the coracoacromial arch2,3 (Figure 1).
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Bicipital groove point tenderness is the most common isolated finding during physical examination of patients with biceps tendinitis. | C | 1 |
| Ultrasonography is the best modality for evaluating isolated biceps tendinopathy extra-articularly. If other pathology is suspected, magnetic resonance imaging should be performed. | C | 3, 5, 14, 33–41 |
| Biceps tenodesis may be performed in patients younger than 60 years, athletes, manual laborers, and patients who object to a muscle bulge above the elbow. | C | 14, 42, 43 |
Biceps tendinitis may also refer to tendinosis, which is a syndrome of overuse and degeneration. Older patients (i.e., athletes older than 35 years or nonathletes older than 65 years) may have acute biceps tendinitis caused by sudden overuse, or biceps tendinosis caused by use over time.4 Primary impingement syndrome is considered the most common cause of biceps tendinosis or tenosynovitis (i.e., inflammation of the tendon sheath).4 Primary impingement is a mechanical impingement under the coracoacromial arch caused by bone spur formation of the acromion, an unfused acromial apophyses, or thickening of the coracoacromial ligament. It may also be caused by osteoarthritic spurs impinging on the bicipital groove.3 Primary impingement in athletes older than 35 years leads to a higher incidence of rotator cuff tears than in younger athletes.
Anatomy and Physiology
The long head of the biceps tendon rises from the supraglenoid tubercle and the superior glenoid labrum. The proximal portion of the long head of the biceps tendon is extrasynovial but intra-articular.5 The tendon travels obliquely inside the shoulder joint, across the humeral head anteriorly, and exits the joint within the bicipital groove of the humeral head beneath the transverse humeral ligament. The bicipital groove is defined by the greater tuberosity (lateral) and the lesser tuberosity (medial). The biceps tendon is contained in the rotator interval, a triangular area between the subscapularis and supraspinatus tendons at the shoulder (Figure 1). The rotator interval is responsible for keeping the biceps tendon in its correct location.6–8 Because the rotator interval is usually indistinguishable from the rotator cuff and capsule, lesions of the biceps tendon are usually accompanied by lesions of the rotator cuff.9
SLAP lesions are often present in patients with biceps tendinitis and tendinosis. The anterosuperior labrum and superior labrum are more likely to tear than the inferior portion of the labrum because they are not attached as tightly to the glenoid.9–13 Additionally, certain conditions that affect the glenohumeral joint may also involve the biceps tendon because it is intra-articular. These may include rheumatologic (e.g., rheumatoid arthritis, lupus), infectious, or other types of reactive or inflammatory conditions.
Diagnosis
HISTORY AND PHYSICAL EXAMINATION
Patients with biceps tendinitis often complain of a deep, throbbing ache in the anterior shoulder. The pain is usually localized to the bicipital groove and may radiate toward the insertion of the deltoid muscle, or down to the hand in a radial distribution. This makes it difficult to distinguish from pain that is secondary to impingement or tendinitis of the rotator cuff, or cervical disk disease.14 Pain from biceps tendinitis usually worsens at night, especially if the patient sleeps on the affected shoulder. Repetitive overhead arm motion, pulling, or lifting may also initiate or exacerbate the pain.9 The pain is most noticeable in the follow-through of a throwing motion.3 Instability of the tendon may present as a palpable or audible snap when range of motion of the arm is tested.
Rupture of the biceps tendon is one of the most common musculotendinous tears. If the biceps has ruptured, patients will describe an audible, painful popping, followed by relief of symptoms. The anterior shoulder may be bruised, with a bulge visible above the elbow as the muscle retracts distally from the rupture point. Risk factors of biceps rupture include a history of rotator cuff tear, recurrent tendinitis, contralateral biceps tendon rupture, rheumatoid arthritis, age older than 40 years, and poor conditioning.9 If a patient has a feeling of popping, catching, or locking in the shoulder, a SLAP lesion may be present. This usually occurs after trauma, such as a direct blow to the shoulder, a fall on an outstretched arm, or repetitive overhead motion in athletes.12,14–17
The most common finding of biceps tendon injury is bicipital groove point tenderness.1 During physical examination, the patient stands or sits with the arm at his or her side in 10 degrees of internal rotation. When the arm is in this position, the humeral head with the bicipital groove faces forward. External rotation of the arm and humeral head places the tender bicipital groove in a posterolateral position. This movement is one of the most specific findings of biceps tendon injury.1
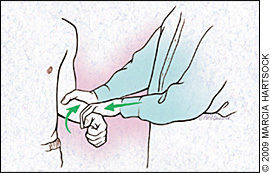
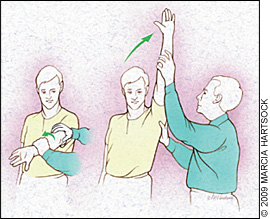
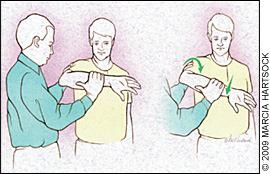
Many provocative tests (i.e., Yergason, Neer, Hawkins, and Speed tests) have been developed to isolate pathology of the biceps tendon12; however, because these tests create impingement underneath the coracoacromial arch, it is difficult to rule out concomitant rotator cuff lesions. The Yergason test requires the patient to place the arm at his or her side with the elbow flexed at 90 degrees, and supinate against resistance18 (Figure 2). The test is considered positive if pain is referred to the bicipital groove. The Neer test involves internal rotation of the arm while in the forward flexed position16 (Figure 3). If the patient experiences pain, it is a positive sign of impingement syndrome. During the Hawkins test, the patient flexes the elbow to 90 degrees while the physician elevates the patient's shoulder to 90 degrees and places the forearm in a neutral position19 (Figure 4). With the arm supported, the humerus is rotated internally. The test is positive if bicipital groove pain is present. For the Speed test, the patient tries to flex the shoulder against resistance with the elbow extended and the forearm supinated9,20 (Figure 5). A positive test is pain radiating to the bicipital groove. If any of these tests is positive, it indicates that impingement is present, which can lead to biceps tendinitis or tendinosis.
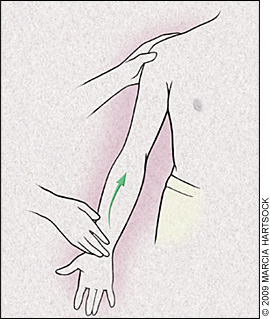
Scapular dysfunction should be suspected if the patient has evidence of medial or inferomedial border prominence of the scapula when viewed posteriorly with the patient at rest.2 Posterior capsule tightness is apparent with decreased internal rotation of the shoulder.3 The anterior slide test can identify SLAP lesions9 (Figure 6). With the patient in a hands-on-hips position, the scapula and clavicle are stabilized by one of the examiner's hands while the other hand is used to apply anterior-superior force at the elbow of the affected side. A positive test is a “click” or “pop” localized to the anterior shoulder and felt underneath the examiner's hand on the acromion, or the reproduction of painful symptoms.21

DIAGNOSTIC AND THERAPEUTIC INJECTIONS
Injections of a local anesthetic may further differentiate the origin of shoulder pain. An injection of 8 to 10 mL of 1% lidocaine (Xylocaine) into the subacromial space under sterile conditions should relieve the pain of rotator cuff tendinitis, but not that of biceps tendinitis.22 A local anesthetic or corticosteroid solution may be injected into the biceps tendon sheath, but the injection must not enter the tendon because of the risk of rupture.5–8,10–12,14,15,23–27 Table 119,26,28 and Figure 7 describe the specifics of the biceps tendon sheath injection, and Table 2 compares various corticosteroid solutions and proper dosages. Ultrasonographic guidance may increase the accuracy of the injection and has been shown to produce a fivefold increase in analgesic effect.29,30 Ultrasonography may also be used to aspirate and disperse calcific deposits within the tendons of the rotator cuff.28,31
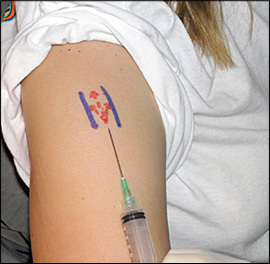
| 1. Obtain oral or written informed consent. The potential risks of the injection include infection; bleeding; skin atrophy and depigmentation; allergic reaction to medication; or temporarily increased pain. |
| 2. Assemble the necessary equipment. The injection requires a 21-or 22-gauge 1.5-inch needle, 8 mL of 1% lidocaine (Xylocaine), 1 mL of 8.4% sodium bicarbonate to decrease the sting of the injection, one 10-mL syringe, one 1- or 3-mL syringe, corticosteroid solution (Table 2), alcohol wipes, povidone-iodine wipes or swabs, some 2- × 2-inch pieces of gauze, a plastic bandage, gloves (sterile or nonsterile), and a marking pen. |
| 3. Sterilize the injection area and use the thumb to palpate the point that is most painful over the bicipital groove. Confirm this is the biceps tendon by externally rotating the arm and placing the elbow in 90 degrees of flexion. Insert the 10-mL syringe of 1% lidocaine plus sodium bicarbonate with the 21- or 22-gauge 1.5-inch needle subcutaneously parallel to the bicipital groove. Inject approximately 5 mL of lidocaine plus sodium bicarbonate around the biceps tendon sheath in a fan-like distribution after aspirating and checking to avoid blood vessels. Ensure that the injection is not into the tendon itself because of the risk of rupture. |
| 4. If a corticosteroid injection is required, use a hemostat between the needle and skin to hold the needle in place while changing to the 1- or 3-mL syringe containing the corticosteroid solution. |
| 5. After the corticosteroid solution is injected, remove the syringe and reattach the 10-mL syringe with lidocaine and sodium bicarbonate. Slowly withdraw the needle while injecting the remaining lidocaine and sodium bicarbonate. This will flush any remaining corticosteroid solution out of the needle, lessening the chance that any remaining solution might cause skin atrophy or depigmentation. An alternative technique is to combine the lidocaine with sodium bicarbonate and corticosteroid solution in the same syringe to avoid changing syringes. |
| 6. Apply the plastic bandage. Instruct the patient to keep it on for eight to 10 hours and watch for signs of infection, which may include erythema, increased pain, pus at the injection site, and a low-grade fever of 100.4°F (38°C) or higher. |
| 7. Reexamine the patient after 15 to 20 minutes. Pain relief indicates a diagnosis of biceps tendinitis. Confirm the diagnosis by performing the Yergason test. It should be negative. A patient may also report pain relief if there is instability or subluxation of the biceps tendon. If the shoulder is still painful, consider problems with the rotator cuff, adhesive capsulitis, calcific tendinitis, or subacromial bursitis. |
| Corticosteroid | Preparation strength (mg per mL) | Common dosages for tendon sheath injection (mg) |
|---|---|---|
| Triamcinolone acetonide (Kenalog) | 10 | 5.0 to 10.0 |
| Methylprednisolone (Depo-Medrol) | 20 | 5.0 to 10.0 |
| Dexamethasone | 4 | 0.8 to 2.0 |
| Betamethasone acetate, betamethasone sodium phosphate (Celestone Soluspan) | 6 | 1.5 to 3.0 |
RADIOLOGIC EXAMINATION
Radiologic evaluation to diagnose biceps tendinitis or tendinosis should begin with radiography of the shoulder to rule out primary causes of impingement (Table 35,10,12,14,32–41 ). Negative results on radiography should be followed by ultrasonography of the shoulder, which is the best method by which to extra-articularly visualize the biceps tendon. Suspected accompanying anatomic lesions may be seen with magnetic resonance imaging (MRI).3,5,14,33–41 Many surgeons prefer obtaining MRI arthrography or computed tomography arthrography before surgery to visualize the intraarticular tendon and related pathology. If the patient demonstrates shoulder weakness and pain with an intact rotator cuff and labrum, electromyography should be performed to rule out a neuropathy.3
| Imaging study | Advantages | Disadvantages |
|---|---|---|
| Arthrography (used with MRI or CT to visualize the joint capsule and glenoid labrum)39 | CT arthrography shows biceps tendon subluxations, ruptures, dislocations, and SLAP lesions14 MRI arthrography is preferable for diagnosing biceps lesions and SLAP lesions14 because the agreement between MRI and arthroscopy for biceps lesions is only 37 percent and 60 percent for rotator cuff lesions | Invasive Filling of the biceps tendon sheath is unreliable40 Sharp images of the tendon may be lost41 Ionizing radiation |
| Bicipital groove view radiography33 | Shows the width and medial wall angle of the bicipital groove, spurs in the groove, and supertubercular bone spur or ridge Inexpensive12 | Does not show possible intra-articular disorders of the labrum (soft tissue injuries)32 |
| MRI | Excellent evaluation of the superior labral complex and biceps tendon39 | Partial tears of the biceps tendon are more difficult to detect than complete ruptures Expensive5 Poorly correlated with arthroscopy14 |
| Radiography (anteroposterior views of the shoulder and acromioclavicular joint, lateral axilla, outlet view, and ALVIS view)10 | Rules out shoulder fracture and strains or dislocations of the acromioclavicular joint and arthritis of the glenohumeral and acromioclavicular joint Inexpensive Cystic changes in the lesser tuberosity are a sign of biceps tendinosis or upper subscapularis tear14 In impingement syndrome, a subacromial spur is usually visible on the outlet and ALVIS views | Shows only bony origins of impingement syndrome and not soft tissue |
| Ultrasonography | Relatively inexpensive May be used for patients with metallic implants Dynamic Widely available No ionizing radiation Offers better spatial resolution than MRI and may be used for local anesthetic or corticosteroid injections into the biceps tendon sheath14,33–39 An overall sensitivity of 49 percent and a specificity of 97 percent | Requires an experienced operator High frequency array transducer Blind areas Difficult to scan patients who are obese14,33–39 |
Treatment
CONSERVATIVE
Biceps tendinitis or tendinosis may respond to analgesia with nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen (to avoid side effects from NSAIDs), ice, rest from overhead activity, or physical therapy.14 Rehabilitation of an athlete's shoulder involves four phases: rest; stretching exercises of the scapula, rotator cuff, and posterior capsule; strengthening; and a progressively difficult throwing program. The patient may begin exercises after the shoulder is pain-free. The goal of stretching is to regain a balanced range of motion without stiffness or pain in any position. The stretching program should include the hamstrings and low back as well.3 A subtle loss of motion in the low back and hamstrings may lead to a major imbalance of the shoulder-stabilizing ligaments and the scapula. A throwing program may be started after the rotator cuff, scapular rotators, and prime humeral movers (i.e., pectoralis major, latissimus dorsi, and deltoid) are strong enough.
The same program applies to the nonathlete, but with less emphasis on throwing.4 If additional therapy is needed for pain relief, or if the diagnosis is in doubt, an injection of local anesthetic (e.g., 1% lidocaine with or without a mild corticosteroid solution) into the biceps tendon sheath may be considered.
SURGICAL
Surgery should be considered if conservative measures fail after three months. Structures causing primary and secondary impingement may be removed, and the biceps tendon may be repaired if necessary. Debridement should be performed if less than 50 percent of the biceps tendon is torn.14 Biceps tenodesis may be considered in serious tears or rupture.14,35,42 This involves the attachment of the cut biceps tendon to the bicipital groove or transverse humeral ligament with suture anchors or screws. A biceps tenotomy may be performed to remove the ruptured biceps tendon from the glenohumeral joint, and tenodesis may be avoided without significant loss of arm function.43 Tenotomy is the procedure of choice for inactive patients 60 years and older with a ruptured biceps tendon.43 Tenodesis is a reasonable option for patients younger than 60 years, as well as active patients, athletes, manual laborers, and patients who object to a muscle bulge above the elbow.14,42,43