
Am Fam Physician. 2009;80(6):639-640
Author disclosure: Nothing to disclose.
A 61-year-old man presented with a three-week history of progressive lower extremity weakness and gait instability. He did not report having fever or weight loss, and he had no history of bowel or bladder dysfunction, seizure, or trauma. He had a history of cocaine abuse and hypertension, and he was taking lisinopril (Zestril).
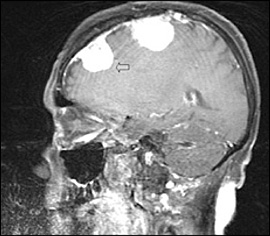
The patient's vital signs were normal. Neurologic examination demonstrated lower extremity weakness, hyperreflexia, and mild weakness bilaterally (movement was possible against some resistance, with full anti-gravity strength). His gait was ataxic. There was no evidence of sensory deficits, cranial nerve deficits, or dysmetria. Laboratory test results were unremarkable. T1-weighted magnetic resonance imaging (MRI) of the spinal cord revealed an enhancing lesion at T8, which was extradural and compressing the spinal cord (Figure 1). T1-weighted MRI of the brain revealed multiple homogenously enhancing lesions (Figure 2). Excision of the spinal cord lesion completely resolved the lower extremity weakness.

Question
Discussion
The answer is B: meningioma. The imaging studies demonstrate the presence of extra-axial brain and spinal tumors, which are well circumscribed and enhance with contrast. Testing of the surgical specimen confirms a meningioma. Meningiomas are the most common benign tumors of the central nervous system, accounting for 15 to 20 percent of all primary brain tumors.1 They arise from arachnoid cells in the dura mater. Meningiomas are more common in women and have a peak incidence between 60 and 80 years of age.2 Meningiomas have typical psammoma bodies on histopathology.
Less than 10 percent of meningiomas cause symptoms, and many are discovered incidentally. If there are presenting symptoms, seizure and weakness are most common. Meningiomas usually occur at the coronal suture; however, other common sites include the parasagittal region, sphenoid ridge, parasellar region, and olfactory groove. Less than 2 percent of meningiomas are extracranial. Tumor location and resectability are the most important factors in clinical outcome. On MRI, meningiomas are typically isointense with gray matter and display a strong postcontrast homogenous enhancement, and 60 percent have a dural tail. They can be easily distinguished from other tumors by presence of homogenous isointense enhancement, absence of central necrosis, and typical location.3
Lymphomas are rare, usually occur in men, and are cortical. They can have ring, heterogeneous, or homogenous enhancement and may have central necrosis or hemorrhage. They can involve the spinal nerve roots and the cranial nerves. Thickened nerves on imaging should always be considered abnormal. Although primary lymphomas exist, they are generally associated with immunodeficiency.
Metastatic lesions are irregular, nodular, typically cortical, and located near the gray-white matter junction. There is ring or irregular enhancement of the lesions. The lesions are commonly target-shaped and surrounded by vasogenic edema, which is hypointense on contrast computed tomography and MRI. Central necrosis is also often present on imaging.
Schwannomas are dumbbell-shaped lesions that originate in Schwann cells, which are present in cranial and spinal nerves. Schwannomas have radiologic features similar to those of meningiomas. The key to differentiating Schwannomas and meningiomas is location and histology. Schwannomas occur along the anatomic locations of cranial and spinal nerves, whereas meningiomas can be present anywhere on the neuraxis.
| Condition | Prevalence | Imaging findings |
|---|---|---|
| Lymphomas | Rare | Irregular, large lesions; may cross midline; hypointense on T1- and T2-weighted MRI with ring, heterogeneous, or homogenous contrast enhancement; surrounding vasogenic edema |
| Meningiomas | Very common | Multiple, extra-axial, well-circumscribed lesions; isointense on T1- and T2-weighted MRI with certain homogenous contrast enhancement; dural tail; calcifications |
| Metastasis | Common | Irregular, nodular brain lesions that are typically target shaped; ring or irregular enhancement; predominantly more cortical than extra-axial; vasogenic edema; located at gray-white matter junction; thickened nerve roots; central necrosis often present |
| Schwannomas | Common | Lobulated, well-circumscribed lesions; may show cystic degeneration; arise from cranial and spinal nerves; spindle cells with extradural, dumbbell-shaped lesions at typical locations; hyperintense and hypointense on T1- and T2-weighted MRI with contrast enhancement |