
Am Fam Physician. 2009;80(7):697-704
A more recent article on Henoch-Schönlein Purpura (IgA Vasculitis) is available.
Patient information: See related handout on Henoch-Schönlein purpura, written by the authors of this article.
Author disclosure: Nothing to disclose.
Henoch-Schönlein purpura is an acute, systemic, immune complex-mediated, leukocytoclastic vasculitis. It is characterized by a triad of palpable purpura (without thrombocytopenia), abdominal pain, and arthritis. Most patients have an antecedent upper respiratory illness. More than 90 percent of Henoch-Schönlein purpura cases occur in children younger than 10 years; however, adults with this condition are more likely to experience complications than children. All patients with Henoch-Schönlein purpura develop a purpuric rash, 75 percent develop arthritis, 60 to 65 percent develop abdominal pain, and 40 to 50 percent develop renal disease. Because Henoch-Schönlein purpura spontaneously resolves in 94 percent of children and 89 percent of adults, supportive treatment is the primary intervention. Oral prednisone at 1 to 2 mg per kg daily for two weeks has been used to treat abdominal and joint symptoms. A meta-analysis found that corticosteroid use in children reduced the mean time to resolution of abdominal pain and decreased the odds of developing persistent renal disease. Early aggressive therapy with high-dose steroids plus immunosuppressants is recommended for patients with severe renal involvement. Long-term prognosis depends on the severity of renal involvement. End-stage renal disease occurs in 1 to 5 percent of patients.
Henoch-Schönlein purpura is an acute, systemic, immune complex-mediated, leukocytoclastic vasculitis. It is characterized by a clinical triad of palpable purpura (without thrombocytopenia), abdominal pain, and arthritis. Glomerulonephritis and gastrointestinal bleeding are common complications.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Early oral prednisone treatment at 1 to 2 mg per kg daily for two weeks reduces the intensity of joint and abdominal pain from Henoch-Schönlein purpura in children. | B | 30 |
| Early prednisone treatment for Henoch-Schönlein purpura does not prevent renal disease, although it is effective in treating renal involvement and reduces the odds of developing persistent renal disease in children. | A | 30, 31 |
| Early prednisone treatment reduces the mean resolution time of abdominal pain from Henoch-Schönlein purpura in children. | A | 30, 31 |
| In patients with a normal initial urinalysis or with isolated hematuria, a monthly urinalysis should be continued for six months to detect signs of renal involvement. | C | 33 |
Epidemiology
Henoch-Schönlein purpura occurs in approximately 10 to 22 persons in 100,000 each year.1-4 It is most commonly seen from late autumn to early spring, but it may occur at any time.5 More than 90 percent of patients are children younger than 10 years, with a peak incidence at six years of age.2-5 However, it is also seen in infants, adolescents, and adults. Henoch-Schönlein purpura is milder in infants and children younger than two years.6 It is more severe and more likely to cause long-term renal disease in adults.7,8 Henoch-Schönlein purpura is the most common vasculitis in children and has a slight predominance in males.3-5,9
Pathophysiology
In patients with Henoch-Schönlein purpura, immunoglobulin A (IgA) immune complexes are deposited in small vessels, which causes petechiae and palpable purpura. When immune complexes occur in small vessels of the intestinal wall, gastrointestinal hemorrhage may develop. If the immune complexes affect the renal mesangium, it may produce mild proliferative to severe crescentic glomerulonephritis.10
Exposure to an antigen from an infection, medication, or other environmental factor may trigger antibody and immune complex formation. Group A streptococcus has been found in cultures of more than 30 percent of children with Henoch-Schönlein nephritis, and serum antistreptolysin-O titers are more likely to be positive in patients with Henoch-Schönlein nephritis.4,11 Other postulated viral and bacterial triggers of Henoch-Schönlein purpura include parvovirus B19, Bartonella henselae, Helicobacter pylori, Haemophilus parainfluenza, Coxsackie virus, adenovirus, hepatitis A and B viruses, mycoplasma, Epstein-Barr virus, varicella, campylobacter, and methicillin-resistant Staphylococcus aureus.12-15
Clinical Presentation
The onset of purpura, abdominal pain, and arthritis may be in any sequence, although abdominal pain and arthritis are not universally present. The timing of symptoms may be within days or insidious over a period of weeks.5 Henoch-Schönlein purpura usually follows an upper respiratory infection.11,16 Fatigue and low-grade fever are also common.
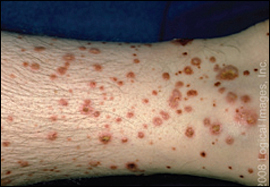
All patients with Henoch-Schönlein purpura develop a nonpruritic rash that starts briefly as erythematous papules or urticarial wheals, and then matures into crops of petechiae and purpura16 (Figure 1). Purpura is defined as nonblanching cutaneous hemorrhages that are greater than 10 mm in diameter. The purpura can enlarge into palpable ecchymoses. The lesions change from red to purple to rust-colored before fading over a period of approximately 10 days (Figure 2). The rash is most commonly located in dependent areas that are subject to pressure, such as the lower extremities, belt line, and buttocks (Figure 3). The purpura is usually seen on the extensor surfaces of the extremities.


A nonmigratory arthritis occurs in 75 percent of patients with Henoch-Schönlein purpura.13,16 The knees and ankles are more commonly involved than small joints. The arthritis symptoms include swelling, warmth, and tenderness. The symptoms are transient, leave no deformity, and may precede the purpuric rash in 15 to 25 percent of patients.2,3
Abdominal pain occurs in 60 to 65 percent of patients, and may mimic an acute abdomen in terms of severity.13,16 The pain is typically colicky, and occurs about one week after the onset of the rash. Vomiting and gastrointestinal bleeding (occult and gross) will develop in 30 percent of patients.17 In rare cases, gastrointestinal hemorrhage may be severe.17 Intussusception may also occur, with a mural hematoma serving as the lead point for bowel telescoping.17
Renal disease is the most serious sequela of Henoch-Schönlein purpura, occurring in 40 to 50 percent of patients.18 Although death from Henoch-Schönlein purpura is rare, renal disease is the leading cause of death in these patients.18 Risk of renal disease is greatest in persons older than 10 years with persistent purpura, severe abdominal pain, or relapsing episodes.8,19 Unlike abdominal pain or arthritis that may precede the rash, renal disease is a late sequela. It usually starts within the first month and rarely occurs more than six months after the illness begins.16 Signs of Henoch-Schönlein purpura-associated renal disease are microscopic hematuria, red cell casts, and proteinuria. Renal disease will spontaneously remit in most patients. However, progressive glomerulonephritis may develop; patients with persistent proteinuria are at the highest risk of this complication.18
Diagnosis
There is no definitive test to diagnose Henoch-Schönlein purpura. The clinical triad of purpura, abdominal pain, and arthritis should raise concern. Palpable purpura in the absence of thrombocytopenia is most suggestive and is present in all patients.5 Punch biopsy of the skin is useful to show the characteristic leukocytoclastic vasculitis.5 Renal biopsy will demonstrate a membranoproliferative glomerulonephritis similar to IgA nephropathy.
In 1990, the American College of Rheumatology defined criteria for the diagnosis of Henoch-Schönlein purpura.20 The criteria required the presence of two out of four features, and yielded a diagnostic sensitivity of 87.1 percent and specificity of 87.7 percent.20-22 The criteria were: patient 20 years or younger at onset, palpable purpura (without thrombocytopenia), bowel angina (diffuse abdominal pain or diagnosis of bowel ischemia), and histologic changes showing granulocytes in small walls of arterioles and venules (leukocytoclastic vasculitis).20 In 2006, the criteria were revised to make palpable purpura a mandatory feature, remove the age criterion, add arthritis as a criterion, and replace granulocytes in biopsy specimens with IgA deposition.23,24 These criteria have been accepted by expert organizations but still await validation in prospective trials (Table 120,21,23).
| American College of Rheumatology, 1990 |
Presence of two or more of the following:
|
| International Consensus Conference, 2006 |
Palpable purpura in the presence of one or more of the following:
|
Because there are no definitive serologic tests for Henoch-Schönlein purpura, the purpose of laboratory evaluation is to identify complications or exclude other diseases (Table 2).3,11,16 Useful baseline studies include renal function tests (e.g., electrolytes, blood urea nitrogen, creatinine, urinalysis), complete blood count with platelet count, coagulation profile (e.g., prothrombin time, partial thromboplastin time, fibrinogen, fibrin degradation products), and IgA levels.3,11,16 A normal platelet count, leukocytosis, eosinophilia, azotemia, elevated serum IgA levels, hematuria, proteinuria, and red blood cell casts are commonly seen. The need for blood cultures, antistreptolysin-O titers, renal biopsy, and tests to identify other infectious agents depends on the presence of clinical indicators of specific infections or progressive renal disease.
| Laboratory test | Indication |
|---|---|
| Antistreptolysin-O titers | Previous streptococcal infection implicated as predisposing factor in many patients |
| Basic metabolic panel (e.g., electrolytes, blood urea nitrogen, creatinine) | Monitor for renal insufficiency or failure |
| Electrolyte imbalance may exist in patients with significant gastrointestinal involvement | |
| Blood culture | Evaluate for bacteremia or sepsis as possible cause |
| Coagulation profile (PT/aPTT) | Evaluate for bleeding diathesis |
| Complete blood count | Thrombocytopenia suggests alternate diagnosis |
| Evaluate for anemia because of risk of gastrointestinal bleeding | |
| Mild leukocytosis typically seen with Henoch-Schönlein purpura | |
| IgA levels | Elevated IgA levels support diagnosis of Henoch-Schönlein purpura over other forms of leukocytoclastic vasculitis, but is nonspecific |
| Skin or renal biopsy | Assess for IgA deposition to assist in diagnosis |
| Aid in prognosis in patients with renal involvement | |
| Urinalysis | Assess for renal involvement (microscopic or gross hematuria, with or without proteinuria) |
Imaging studies are not performed routinely in the evaluation of Henoch-Schönlein purpura.17 Arteriography may be required to localize hemorrhage, and gastrointestinal endoscopy may be needed to evaluate gastrointestinal bleeding.17 Abdominal ultrasonography or computed tomography may be needed to assess abdominal pain.17,25 Barium enema may be used safely to diagnose and treat suspected intussusception, although the location is usually ileoileal and less amenable to nonsurgical correction by barium enema.25
Differential Diagnosis
Key differential diagnostic considerations of Henoch-Schönlein purpura are shown in Table 3.26,27 These include polyarteritis nodosa, juvenile rheumatoid arthritis, acute hemorrhagic edema of infancy, Wegener granulomatosis, meningococcemia, Kawasaki disease, and thrombocytopenic purpura.26,27 All causes of acute surgical abdomen are diagnostic considerations in patients with severe abdominal pain. Prominent purpuric ecchymoses in the absence of other symptoms may be mistaken for child abuse. Other causes of palpable purpura include Rocky Mountain spotted fever and bacterial endocarditis. Henoch-Schönlein purpura may occur with other forms of autoimmune disease, such as familial Mediterranean fever or inflammatory bowel disease. One study reported that 5 percent of patients with familial Mediterranean fever will get Henoch-Schönlein purpura.28
| Diagnosis | Clinical features | Key diagnostic tests |
|---|---|---|
| Acute abdomen | Acute or subacute onset of abdominal pain or rigidity | CBC, hCG, amylase, liver function tests, urinalysis, abdominal CT scan |
| Acute hemorrhagic edema | Small vessel leukocytoclastic vasculitis affecting children four to 24 months of age; rapid onset of purpuric lesions on face, ears, and extremities; associated edema of limbs and face | Skin biopsy, CBC, coagulation studies, urinalysis |
| Bacterial endocarditis | Acute or subacute onset of fever; vascular phenomena (e.g., arterial emboli, septic pulmonary infection); immunologic phenomena (e.g., glomerulonephritis, Osler nodes, Roth spots); new valvular regurgitation | Blood cultures drawn more than two hours apart, CBC, ESR, echocardiography |
| Child abuse | Worrisome skin marks (e.g., ecchymosis, shaped contusions, burns, bites, lacerations); blunt abdominal or other trauma; fractures; immersion injuries | Detailed history and physical examination; appropriate laboratory tests and imaging |
| Familial Mediterranean fever* | Paroxysms of fever and polyserositis (e.g., abdominal pain, peritonitis, pleurisy, pericarditis, synovitis) | Mutation analysis for the MEFV gene mutation |
| Hypersensitivity (leukocytoclastic) vasculitis | Small-vessel vasculitis associated with abrupt onset of a rash (palpable purpura most common); fever, malaise, myalgia, and anorexia after exposure to triggering antigen (e.g., drug, infectious agent) | Skin biopsy, CBC, ESR |
| Inflammatory bowel disease* | Diarrhea (bloody or nonbloody), abdominal pain, cramping, fever, and weight loss | CBC, ESR, electrolytes, stool studies, colonoscopy with biopsy |
| Juvenile rheumatoid arthritis | Insidious or abrupt onset of morning stiffness or arthralgia that may be associated with spiking fevers and an evanescent salmon-pink rash | ESR, CBC, antinuclear antibody |
| Kawasaki disease | Child with fever of 102.9°F to 104.9°F (39.4°C to 40.5°C) for five days or longer; associated with extensive polymorphous rash, bilateral conjunctival injection, changes of the lip and oral cavity, unilateral cervical lymphadenopathy, and extremity changes | CBC, CRP, ESR, echocardiography, electrocardiography |
| Leukemia | Nonspecific symptoms of fever, easy bleeding, skin findings (e.g., petechiae, purpura), bone pain, fatigue, hepatosplenomegaly, lymphadenopathy | CBC, ESR, coagulation profile, bone marrow biopsy |
| Meningococcemia | Malaise, fever, rash (e.g., maculopapular rash, petechiae, ecchymosis), and hypotension with possible associated symptoms of meningitis or tenosynovitis | CBC, PT/aPTT, fibrinogen, fibrin degradation productions, blood culture, CSF analysis and culture |
| Polyarteritis nodosa | Multisystem involvement from segmental inflammatory, necrotizing vasculitis of the small- and medium-sized muscular arteries leading to general symptoms of fever, weakness, weight loss, malaise, myalgia, rash (e.g., livedo reticularis, purpura), headache, and abdominal pain | Biopsy of involved organ, urinalysis, CBC, ESR, CRP, angiography |
| Rocky Mountain spotted fever | Headache; fever associated with a centripetal rash (involving palms and soles, spreading to arms, legs, and trunk) that is often petechial; report of recent tick bite or outdoor activity in endemic area | Immunofluorescence staining of tissue specimen or serologic analysis for Rickettsia rickettsii, CBC, electrolytes |
| Thrombocytopenic purpura | Thrombocytopenia associated with petechia or purpura; bleeding (e.g., gingival, gastrointestinal, mucocutaneous); symptoms of end-organ ischemia (in patients with thrombotic disease) | CBC with peripheral smear, coagulation studies, platelet-associated antibody (immunoglobulin G), electrolytes, BUN, creatinine, liver function tests, LDH, urinalysis |
| Wegener granulomatosis | Granulomatous vasculitis with a characteristic triad of involvement of the upper airway (e.g., otitis media, sinusitis, rhinitis), lungs (e.g., pulmonary infiltrates), and kidneys; rash, arthritis/arthralgias, and nervous system (peripheral and central) | Biopsy of involved organ, c-ANCA, CBC, ESR, electrolytes, BUN, creatinine, urinalysis, chest radiography |
Potential Complications
Orchitis and scrotal swelling may occur in up to 35 percent of boys with Henoch-Schönlein purpura.5 Severe scrotal edema may cause testicular torsion, which requires emergent surgical exploration. Fewer than 10 percent of patients with Henoch-Schönlein purpura experience myocardial infarction, pulmonary hemorrhage, or central nervous system involvement with seizures and hemorrhage (Table 45,10,13,16).13,16
| Renal |
| Glomerulonephritis |
| Hemorrhagic cystitis |
| Nephrotic syndrome |
| Renal failure |
| Ureteral obstruction |
| Gastrointestinal |
| Bowel infarction |
| Bowel perforation |
| Duodenal obstruction |
| Gastrointestinal hemorrhage |
| Intestinal stricture |
| Intussusception |
| Pulmonary |
| Alveolar hemorrhage |
| Interstitial infiltrate |
| Pulmonary effusion |
| Central nervous system |
| Aphasia |
| Ataxia |
| Cerebral hemorrhage |
| Chorea |
| Cortical blindness |
| Neuropathy |
| Paresis |
| Seizure |
| Other |
| Anterior uveitis |
| Myocarditis |
| Myositis |
| Orchitis |
| Scrotal edema |
| Testicular torsion |
Management
Because Henoch-Schönlein purpura spontaneously resolves in 94 percent of children and 89 percent of adults, supportive treatment is the primary intervention.5,22,29 Acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDS) may be used to alleviate arthralgia, although NSAIDS may aggravate gastrointestinal symptoms and should be avoided in patients with known renal involvement. Relative rest and elevation of affected extremities during the active phase of the illness may help prevent purpura. Patients should be advised that they may experience recurrent purpura as they increase their activity level.
Hospitalization may be required when adequate outpatient monitoring is unavailable or if dehydration, hemorrhage, or pain control require inpatient management. Nephrology referral is recommended with significant renal involvement.29 In patients with severe renal disease, renal biopsy is needed to provide a definitive diagnosis and guide therapy.29
Early steroid treatment is most appropriate for children with renal involvement or severe extrarenal symptoms.30 It may also help relieve scrotal swelling.5 Oral prednisone at 1 to 2 mg per kg daily for two weeks has been used to treat moderate to severe abdominal and joint symptoms, and to hasten the resolution of Henoch-Schönlein purpura in children.30 A double-blind randomized trial found that early treatment with prednisone reduced abdominal and joint pain severity in children.30 Although prednisone did not prevent renal disease, it was useful in treating renal disease after it started.30 A meta-analysis found that corticosteroid use in children with Henoch-Schönlein purpura reduced the mean time to resolution of abdominal pain and decreased the odds of developing persistent renal disease.31 Steroids did not affect the resolution of the purpura, and no harms were demonstrated.31
Early aggressive therapy is recommended for children and adults with severe renal involvement.30-32 Treatment options include high-dose steroids with immunosuppressants, high-dose intravenous immunoglobulin, plasmapheresis, and renal transplant. A recent trial found that cyclophosphamide (Cytoxan) was effective in patients with overt nephritis, although cyclosporine (Sandimmune) was not helpful (Table 55,16,30,31).32
| Symptom severity | Treatment |
|---|---|
| Minimal | Supportive care |
| Mild (mild arthralgias or abdominal pain) | Acetaminophen or nonsteroidal anti-inflammatory drug |
| Moderate (significant arthritis, abdominal pain, or early renal involvement) | Corticosteroids* |
| Consider subspecialty consultation† | |
| Severe (progressive renal disease, pulmonary hemorrhage) | Corticosteroids* plus adjunctive immunosuppressant (e.g., azathioprine [Imuran], cyclophosphamide [Cytoxan], intravenous immunoglobulin) or plasmapheresis |
| Arrange subspecialty consultation† |
Follow-up Care and Prognosis
Henoch-Schönlein purpura is a self-limited illness that demonstrates no clinical sequelae in most patients without renal involvement. Most patients recover fully within four weeks.16 Recurrences of Henoch-Schönlein purpura occur in up to one third of patients within the first six months after onset and are more common in patients with renal involvement.
Long-term prognosis depends on the severity of renal involvement; end-stage renal disease occurs in 1 to 5 percent of patients.12,29 One systematic review revealed that the onset of renal disease in patients with Henoch-Schönlein purpura developed within four weeks in 85 percent of patients, six weeks in 91 percent of patients, and six months in 97 percent of patients.33 Permanent renal impairment did not develop in patients with a normal urinalysis, although it occurred in 19.5 percent of patients with nephritic or nephrotic syndrome.33
A blood pressure measurement and urinalysis should be performed at the time Henoch-Schönlein purpura is diagnosed and at each return physician office visit.33 Serum blood urea nitrogen and creatinine determination are needed if hematuria or proteinuria are identified.33 If the initial urinalysis is normal, or if there is isolated hematuria (without nephritic or nephrotic syndrome), a monthly urinalysis should be performed for the first six months after the diagnosis of Henoch-Schönlein purpura.33 This will detect the first signs of renal involvement, and facilitate early nephrology consultation and the initiation of steroids.33