
Am Fam Physician. 2009;80(10):1143-1144
Author disclosure: Nothing to disclose.
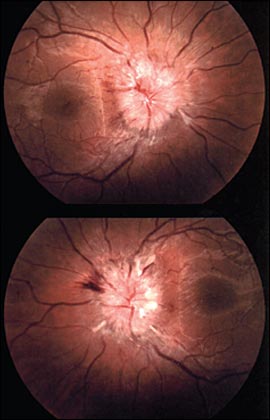
A healthy-appearing 23-year-old woman with no notable medical history presented with a headache, neck stiffness, and visual changes that have persisted for 10 days. The patient reported double vision, blurred vision, and transient visual changes when opening her eyes; however, she had normal visual acuity. She also reported paresthesia in her left arm and hand. She denied having fevers, myalgias, or incontinence. She was afebrile at presentation. Examination revealed tachycardia (heart rate of 110 beats per minute), a body mass index of 35 kg per m2, and nuchal rigidity. Her pupils were equal in size, round, and reactive to light and accommodation. Her vision was 20/20 in both eyes. Funduscopic examination was performed (see accompanying figure).
Question
Discussion
The answer is C: idiopathic intracranial hypertension. The accompanying figure shows widening and blurring of the optic disc margin with compensatory reduction of cup diameter, which is consistent with papilledema. Idiopathic intracranial hypertension, or pseudotumor cerebri, is a syndrome of increased intracranial pressure without a space-occupying lesion. Patients typically present with headache, visual changes, tinnitus, and paresthesia. Brain imaging should be performed initially to rule out a space-occupying lesion and to ensure normal ventricular size. It is then safe to perform a lumbar puncture to demonstrate an elevated opening pressure (greater than 25 cm of water) in the lateral decubitus position.1 When performing a lumbar puncture, it is appropriate to send cerebrospinal fluid for cytology and culture, although specific tests for herpes simplex virus, viral, and Lyme infections are necessary only if the presentation suggests these diagnoses.
Although idiopathic intracranial hypertension is rare, with an incidence of one in 100,000 persons per year, it is 20 times more common in women 20 to 44 years of age who are more than 20 percent above their ideal body weight.2 The syndrome is very rare in persons older than 45 years.
Headache with nuchal rigidity suggests meningeal inflammation, even without a fever. However, papilledema occurs in less than 5 percent of acute bacterial meningitis cases and is very rare with aseptic meningitis.3
Although a complicated migraine headache may be associated with neurologic findings, it does not lead to papilledema.
Multiple sclerosis is more common in young women and can cause a variety of neurologic symptoms, including visual complications from optic neuritis. Optic neuritis causes a papillitis that is difficult to distinguish from papilledema, but papillitis leads to decreased visual acuity.4
A brain tumor must be considered as a cause of papilledema before performing the lumbar puncture. However, in a young woman who is obese with no known cancer history, the probability of a brain tumor is less than that of idiopathic intracranial hypertension.5
| Condition | Characteristics |
|---|---|
| Meningitis | Headache, nausea, and nuchal rigidity, with or without fever; papilledema is rare, especially in aseptic meningitis |
| Complicated migraine headache | Typically, photophobia, phonophobia, and nausea; neurologic changes may occur, but papilledema is not present |
| Idiopathic intracranial hypertension (pseudotumor cerebri) | Headache, nuchal rigidity, papilledema; sensory changes include tinnitus, visual changes, and paresthesia; elevated opening pressure on lumbar puncture; normal visual acuity in acute presentation |
| Multiple sclerosis | Optic changes and urinary retention are often present, and multiple distinct motor or sensory deficits may occur; papillitis with optic neuritis, but decreased visual acuity |
| Brain tumor | May cause headache, nuchal rigidity, sensory changes, papilledema, fever, fatigue, and weight loss; must be considered before idiopathic intracranial hypertension |