
Am Fam Physician. 2009;80(11):1231-1237
Patient information: See related handout on cosmetic procedures, written by the author of this article.
Author disclosure: Nothing to disclose.
Since the approval of botulinum toxin, dermal fillers, and lasers for cosmetic use, minimally invasive aesthetic procedures have rapidly become the treatments of choice for age-related facial changes. In the past 10 years, aesthetic procedures have increased nearly five-fold. Of the 10.2 million aesthetic treatments performed in 2008, 83 percent were minimally invasive procedures. Botulinum toxin and dermal filler injections, laser hair reduction, chemical peels, laser skin resurfacing, microdermabrasion, and intense pulsed light photorejuvenation were the most commonly performed procedures in 2008. These procedures are effective and associated with minimal discomfort, and they have a low incidence of adverse effects and short recovery times. High patient and physician satisfaction have contributed to their growing popularity and availability in the primary care setting. As patient demand for aesthetic treatments increases, family physicians should be familiar with common minimally invasive aesthetic procedures when advising patients or incorporating aesthetic care into office practice.
The number of aesthetic procedures has increased considerably in the United States over the past 10 years, with nearly a fivefold increase from 1997, according to statistics from the American Society for Aesthetic Plastic Surgery (Figure 1).1 Of the 10.2 million treatments performed in 2008, more than 80 percent were minimally invasive procedures, the most common of which were onabotulinumtoxinA (Botox; formerly known as botulinum toxin type A) and dermal filler injections, laser hair reduction, chemical peels, laser skin resurfacing, microdermabrasion, and intense pulsed light photorejuvenation (Figure 2).1
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| OnabotulinumtoxinA (Botox) is safe and effective for reduction of frown lines, crow's feet, and horizontal forehead lines. | A | 14, 23, 24 |
| Dermal fillers effectively reduce nasolabial folds. | A | 32–34 |
| Laser hair reduction effectively reduces unwanted darkly pigmented hair. | A | 36, 38 |
| Laser photorejuvenation effectively reduces benign epidermal pigmented and vascular lesions. | B | 45–47 |
| Microdermabrasion reduces benign epidermal pigmented lesions. | B | 50, 52 |
| Chemical peels (glycolic and salicylic acid) reduce acne vulgaris. | B | 53, 54 |
Minimally invasive procedures have become the primary treatment modalities for addressing mild to moderate age-related facial changes.2 In the past, treatment options were limited to surgical interventions, such as facelifts to redrape and lift lax skin, deep ablative laser resurfacing, and dermabrasion to improve texture, wrinkles, and hyperpigmentation.3,4 Surgery is still an option for many patients, particularly those with signs of advanced facial aging. However, there has been a trend away from invasive one-time procedures, which may radically alter appearance and have greater risks, toward minimally invasive nonsurgical procedures, which offer subtle enhancements.5 Minimally invasive aesthetic procedures reliably achieve good outcomes, have minimal recovery times6 and a low incidence of side effects, and are associated with high patient satisfaction7 (Table 18-15 ).
| Procedure | Indication | Treatments required and duration of action | Advantages | Disadvantages |
|---|---|---|---|---|
| Onabotulinum toxinA (Botox) injection | Dynamic facial lines and wrinkles in the upper one third of the face | One treatment every three to four months | Short procedure time, dramatic results | Small margin for technical error with injection placement; high patient expectations |
| Dermal filler injection | Facial wrinkles and folds in the lower two thirds of the face; lip enhancement | One treatment every three to 24 months; duration of action varies with product composition and treatment area (Table 2) | Immediate results | Postprocedure swelling and bruising; injection proficiency and consistency of outcomes require practice |
| Laser hair reduction | Unwanted hair | Series of six treatments with at least one-month intervals; long-term reduction in hair growth of 50 percent or more | Faster and less painful than other methods of permanent hair reduction, such as electrolysis | Risk of burns, hyperpigmentation, and hypopigmentation*; reduced effectiveness with fine, lighter-colored hair |
| Laser photo-rejuvenation | Benign epidermal pigmented and vascular lesions | Series of two to five treatments every two to four weeks, based on severity of lesions and device used; results last up to several years | Highly selective for lesions without damaging surrounding skin | Risk of burns, hyperpigmentation, and hypopigmentation* |
| Micro-dermabrasion | Benign epidermal pigmentation, rough skin texture, acne, fine lines, superficial acne scars | Series of six treatments every two to four weeks with monthly or quarterly maintenance treatments; short-term results | Safe for all skin types; few absolute contraindications | Worsening telangiectasias and erythema possible; minimal change with single treatment |
| Chemical peels | Benign epidermal pigmentation, rough skin texture, acne, fine lines, superficial acne scars | Series of six treatments per month with monthly to quarterly maintenance treatments; short-term results | Inexpensive | Less control over depth of exfoliation; postprocedure skin peeling; minimal change with single superficial treatment; risk of scarring, hyperpigmentation, and hypopigmentation* with deeper peels |
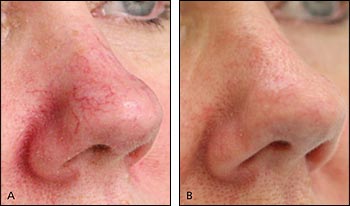
Assessment of aging changes can be approached by evaluation of facial regions. Frown lines, horizontal forehead lines, and crow's feet form in the upper one third of the face. Initially these are dynamic lines, visible during active muscle contraction, but over time they become deeper static lines that can be seen at rest. Prominent nasolabial folds and flattening of malar fat pads appear in the midface. The lower one third of the face exhibits later and more profound changes, with upper lip atrophy, perioral wrinkling, marionette lines, and jowl formation. Skin surface changes are evident in the 30s, with textural roughness and dryness, mottled pigmentation with solar lentigines around the periphery of the face, and telangiectasias around the nasal ala and cheeks16 (Online Figure A).
Minimally invasive procedures can target patients' specific aging complaints by relaxing overactive facial muscles, filling wrinkles, redefining facial contours, reducing unwanted hair, and improving epidermal hyperpigmentation and vascularities.17 When performed in an ongoing capacity, these procedures can promote and maintain a youthful appearance.6
This article is an overview of the most commonly performed minimally invasive aesthetic procedures and the evidence supporting their use, with an emphasis on procedures that family physicians can readily incorporate into office practice.
Botulinum Toxin
Botulinum toxin is a potent neurotoxin protein derived from Clostridium botulinum. It exerts its effect at the neuromuscular junction by inhibiting the release of acetylcholine, causing temporary chemical denervation. Injection of small quantities into specific overactive facial muscles causes localized muscle relaxation, with smoothing of the overlying skin and reduction of wrinkles.
Although onabotulinumtoxinA was first noted for its toxic properties, it is now routinely used as a medicine to treat clinical conditions such as blepharospasm, strabismus, cervical dystonia, hyperhidrosis, migraines, and muscle spasticity.18-20 OnabotulinumtoxinA was approved by the U.S. Food and Drug Administration (FDA) for cosmetic use in 2002 as Botox to treat the glabellar complex muscles that form frown lines. It is now the treatment of choice for lines and wrinkles occurring in the upper one third of the face.21,22 A similar product, abobotulinumtoxinA (Dysport; formerly known as botulinum toxin type A) was approved by the FDA in 2009 for the treatment of glabellar frown lines as well.
There are many aesthetic indications for onabotulinumtoxinA, but treatment of frown lines23 and off-label treatment of horizontal forehead lines14 and crow's feet24 offer the most predictable results, with the greatest effectiveness and fewest adverse effects.2,8 Figure 3 shows a woman attempting to contract glabellar complex muscles before treatment with botulinum toxin and one month after treatment, with significant reduction in dynamic frown lines.

Dermal Fillers
Dermal fillers are injectable products that temporarily restore soft-tissue volume. They are the treatment of choice for facial lines and contour defects in the lower two thirds of the face.9
Dermal fillers vary by composition, duration of action, palpability, ease of administration, complications, and other factors, all of which affect treatment results.25,26 Achieving desirable outcomes with dermal fillers depends on the physician's knowledge of filler products and injection skills, as well as an appreciation for aesthetic facial proportions and symmetry. The administration of dermal fillers has a steeper learning curve than that of botulinum toxin and requires practice to consistently achieve desirable results.27
Bovine collagen was one of the first dermal fillers used in the 1980s; however, these products had a duration of action of only three to four months.28 Dermal fillers recently have grown in popularity as new products have been developed, with durations of action from six months to more than one year (Table 2).9,25,26
| Agent (brand name) | Manufacturer | Active component | Duration of action |
|---|---|---|---|
| Cosmoplast | Allergan Inc. | Collagen | 3 to 4 months |
| Restylane | Medicis Aesthetics | Hyaluronic acid | 6 to 9 months |
| Perlane | Medicis Aesthetics | Hyaluronic acid | 6 to 9 months |
| Juvéderm | Allergan Inc. | Hyaluronic acid | 9 to 12 months |
| Radiesse | Bioform Medical Inc. | Calcium hydroxylapatite | 12 to 18 months |
| Sculptra | Dermik Laboratories | Poly-l-lactic acid | 12 to 24 months |
Hyaluronic acid is one of the most versatile dermal fillers available with regard to depth of placement and treatment areas.29 Hyaluronic acid is a naturally occurring glycosaminogly-can found in the dermal extracellular matrix; it provides structural support, facilitates transport of cellular nutrients and wastes, and adds volume and fullness to the skin through its hydrophilic capacity. After injecting small quantities (1 to 2 mL) into the dermis, facial wrinkles and folds are temporarily reduced and smoothed.30 Some of the most commonly treated areas include the nasolabial folds (Figure 4), lips, oral commissures, and marionette lines9,31–34; however, treatment of the nasolabial fold area is the only FDA-approved indication.

Laser Hair Reduction
Unwanted hair growth is a common aesthetic complaint of men and women10 (Figure 5). The density of body hair is predetermined at birth; however, most hairs are nonvisible because they are thin, nonpigmented vellus hairs, or they are dormant. Nonvisible hairs may become visible, pigmented terminal hairs as a result of hormonal changes that occur with age. During menopause, these hairs commonly appear on the chin, upper lip, and anterior neck. In men, new terminal hairs are common on the back and shoulders.35 These changes can be distressing for patients and may affect self-image and self-esteem.

There are numerous laser and other light-based technologies (for the purposes of this article, collectively referred to as lasers) available for hair reduction.10,36-38 The basic principle behind these technologies is selective photothermolysis. Energy is absorbed and concentrated in the target by a light-absorbing pigment called a chromophore. The target is heated and damaged, whereas the surrounding skin, which absorbs minimal energy, is unaffected.39,40 During hair-reduction treatments, the melanin chromophore in the hair bulb absorbs energy, thereby damaging and impairing the hair growth structures.41
Treatment effectiveness is based on patients' skin color and hair characteristics. The best candidates are those with fair skin and coarse, dark hair. Hairs lacking a significant melanin chromophore (e.g., blonde or red hair) are not significantly affected by laser treatments; white and gray hairs do not respond at all.
The safest hair reduction technologies are those with internal cooling mechanisms that provide contact cooling to the skin. These devices maintain a constant temperature of the laser tip throughout treatment. High energies are required to penetrate deeply into the dermis and damage the hair bulb, and cooling mechanisms protect the epidermis from thermal injury and reduce potential complications.42
Laser Photorejuvenation
Many of the skin changes that occur with aging are the result of extrinsic environmental factors, such as cumulative sun exposure, that accelerate the natural aging process.43 These photoaging changes are clinically apparent as benign epidermal pigmented lesions with mottled hyperpigmentation and solar lentigines; benign vascular lesions with telangiectasias, erythema, cherry angiomas, and poikiloderma of Civatte; textural changes with fine lines and laxity; and dysplastic changes with benign and malignant neoplasia44 (Online Figure A).
Photorejuvenation refers to the laser treatment of benign epidermal pigmented and vascular lesions in photoaged skin11,45-47 (Figures 6 and 7). Treatments may be performed on virtually any sun-damaged area, and are commonly performed on the face, neck, chest, and hands.48 Laser photorejuvenation selectively removes lesions without injuring the surrounding skin by targeting the melanin chromophore in pigmented lesions and the oxyhemoglobin chromophore in vascular lesions.39,40 As with laser hair reduction, devices that provide contact skin cooling have the greatest safety profiles.42

Microdermabrasion and Chemical Peels
Microdermabrasion and chemical peels are exfoliation procedures used to superficially resurface the skin. Skin rejuvenation with exfoliation treatments is based on the principles of wound healing. By wounding and removing superficial skin layers in a controlled manner, cell renewal is stimulated, with regeneration of a healthier epidermis and dermis.49 After a series of exfoliation treatments, histologic changes in the skin are evident: a compacted stratum corneum, smoother epidermis, increased dermal thickness with fibroblast production of new collagen and elastin, and increased skin hydration with improved epidermal barrier function.50,51 The result is a clinical improvement in benign epidermal pigmented lesions50,52 and skin texture, and possible improvements in fine lines, pore size, superficial acne scars, and acne vulgaris.12,49,52-56
Exfoliation procedures can be classified as mechanical or chemical. Microdermabrasion is a method of mechanical exfoliation whereby the stratum corneum is removed using a refined abrasive element, such as diamond-tipped pads or a constant flow of aluminum oxide crystals across the skin. Recent advances in microdermabrasion technology combine exfoliation with simultaneous application of topical products.12
Chemical peels are a means of wounding the skin through the application of chemical compounds, such as acids and enzymes. Common agents include alpha hydroxy acids (e.g., glycolic and lactic acids) and beta hydroxy acids (e.g., salicylic acid).57,58 The concentration of active ingredients, pH, time, and method of application determine the depth of skin injury and define the procedure as superficial, medium, or deep exfoliation.13
Final Comment
The number of aesthetic procedures performed in the United States continues to increase annually because of patient demand and advancements in products and technologies. Minimally invasive aesthetic procedures, including botulinum toxin and dermal filler injections for lines and wrinkles; lasers and intense pulsed light for hair reduction, skin resurfacing, and photorejuvenation; and chemical peels and microdermabrasion for exfoliation are the most common treatments, and have become the basis for facial rejuvenation. They offer patients a means to enhance their appearance in a subtle, natural way, and can help maintain a youthful appearance when performed in an ongoing capacity. From the physician's perspective, these procedures can reliably achieve good outcomes, have a low incidence of side effects, and may be readily incorporated into office practice.