
Am Fam Physician. 2010;81(1):73-74
Author disclosure: Nothing to disclose.
A 32-year-old man presented with bilateral blurriness in his distant vision that had worsened over several months. Results of a routine eye examination several years before were normal. The blurriness in his left eye was worse than that in his right eye and was accompanied by cloudiness. He did not have pain, itching, discharge, floaters, blind spots, or nocturnal visual impairment. He had had diabetes for 13 years and was taking insulin.
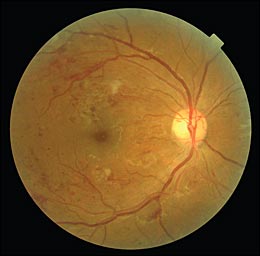
He was undergoing hemodialysis for chronic kidney disease and had hypertension, dyslipidemia, and peripheral vascular disease that led to amputation below his left knee. The patient's visual acuity was 20/50 in his right eye and 20/100 in his left. Scattered hemorrhages, cotton-wool spots, atherosclerosis of the retinal arterioles, and venous engorgement and beading were noted in his right retina (see accompanying figure). Although visualization of the left retina was obscured by posterior subcapsular cataract, hemorrhages and cotton-wool spots were discernible.
Question
Discussion
The answer is C: diabetic retinopathy. In the United States, diabetic retinopathy is the leading cause of blindness in persons 20 to 74 years of age and affects about 800,000 adults with diabetes.1,2 Retinopathy affects 29 percent of persons who have had type 2 diabetes for less than five years, and 78 percent of those who have had type 2 diabetes for 15 or more years.3,4 Diabetic retinopathy is classified as proliferative or nonproliferative, depending on the presence or absence of neovascularization. Nonproliferative retinopathy is further classified based on the severity of microaneurysms, hemorrhages, microvascular abnormalities, and retinal vein dilation.5 Proliferative retinopathy is further classified based on the degree of neovascularization and the presence of vitreous hemorrhage.5 Other findings, including cotton-wool spots, macular edema, and exudates, occur with both types of diabetic retinopathy.
Age-related macular degeneration is the most common cause of irreversible visual loss in persons older than 60 years in the United States.6,7 Macular degeneration occurs when the macular portion of the retina is damaged because of accumulation of drusen within the macula or choroidal neovascularization beneath the macula.7,8 The exudative form of age-related macular degeneration accounts for about 10 percent of cases, but causes most of the visual loss related to the disease.6,7
About 75 percent of central retinal vein occlusion is nonischemic.6 Retinal images show dramatic retinal changes due to hemorrhages, tortuosity, and dilation of all branches of the central retinal vein. The retinal image may have a “blood and thunder” appearance.9 Central retinal vein occlusion can lead to severe optic disc and macular edema, ischemia, hyperemia, and visual loss.6
Drusen are caused by the accumulation of deposits beneath the retinal pigment epithelium.6 The deposits occur throughout the retina and within the optic disc and have unknown etiology. Drusen commonly occur between 45 and 60 years of age,6 and the size and number increase with age. There are several types of drusen, including hard, soft, basal laminar, and calcified.6 Hard drusen are small, discrete, round, yellow-white spots. Soft drusen are larger and have undefined borders. Basal laminar drusen are numerous, uniform, small, round nodules.6 Calcification leads to the glistening appearance of calcified drusen.
Retinitis pigmentosa is a group of hereditary disorders characterized by progressive loss of photoreceptor and retinal pigment epithelium function.6,10 It has a wide range of inheritance patterns and is characterized by diffuse, bilateral retinal dystrophic changes. Black clumps of irregular pigment in the retinal periphery lead to a “bone spicules” pattern.
| Condition | Characteristics |
|---|---|
| Age-related macular degeneration | Macular drusen or neovascularization; distorted vision; blind spots and loss of central vision |
| Central retinal vein occlusion | Dramatic retinal vascular changes leading to a “blood and thunder” appearance; severe retinal edema and hyperemia; tortuous and dilated central retinal vein branches; risk of visual impairment or loss |
| Diabetic retinopathy | Cotton-wool spots; macular edema, exudates; microaneurysms; intraretinal, preretinal, or vitreal hemorrhages; attenuation of arterioles; neovascularization; visual impairment or loss. |
| Drusen | Retinal or optic accumulation of deposits of varying size, shape, border appearance, and number |
| Retinitis pigmentosa | Poor nocturnal vision; retinal pigmentation of a “bone spicules” pattern; dystrophic retinal pigment epithelium; waxy disc pallor; arteriolar attenuation |
