Am Fam Physician. 2010;82(8):959-964
Author disclosure: Nothing to disclose.
For many years, there were no guidelines for evaluating patients with chronic neck pain. However, in the past 15 years, considerable research has led to recommendations regarding whiplash-associated disorders. This article summarizes the American College of Radiology Appropriateness Criteria for chronic neck pain. Imaging plays an important role in evaluating patients with chronic neck pain. Five radiographic views (anteroposterior, lateral, open-mouth, and both oblique views) are recommended for all patients with chronic neck pain with or without a history of trauma. Magnetic resonance imaging should be performed in patients with chronic neurologic signs or symptoms, regardless of radiographic findings. The role of magnetic resonance imaging in evaluating ligamentous and membranous abnormalities in persons with whiplash-associated disorders is controversial. If there is a contraindication to magnetic resonance imaging, computed tomography myelography is recommended. Patients with normal radiographic findings and no neurologic signs or symptoms, or patients with radiographic evidence of spondylosis and no neurologic findings, need no further imaging studies.
Patients with chronic neck pain present physicians with a diagnostic and therapeutic dilemma.1–4 There is considerable controversy in the literature regarding the etiology of chronic neck pain and the role of imaging in the evaluation of the condition. The literature focuses on two general etiologic categories: posttraumatic and degenerative. Posttraumatic etiologies include gross injuries and whiplash syndrome (i.e., any injury to the cervical vertebrae and adjacent soft tissues as a result of sudden jerking). Whiplash syndrome includes extension-flexion mechanisms sustained in rear-end motor vehicle collisions and abrupt lateral flexion mechanisms. Studies in Canada and Scandinavia have identified signs and symptoms that constitute whiplash-associated disorders.4–6 Degenerative etiologies of chronic neck pain include spondylosis, degenerative disk disease, and acute disk herniation. Degeneration may also be secondary to previous injury. In addition, many anecdotal reports of other etiologies exist, including carotid or vertebral artery dissection, arteriovenous malformations, and neoplasms.
Previously, there was little research on the use of imaging modalities in the evaluation of patients with chronic neck pain. Most studies cited the use of radiography, particularly to diagnose spondylosis, degenerative disk disease, or posttraumatic malalignment.4,7 From a radiologic standpoint, a diagnosis of spondylosis could be made if osteophytes, disk space narrowing, or facet disease are present. Other imaging options included facet injections8–10 and provocative tests using diskography. 11–14 More recent literature has focused on the use of magnetic resonance imaging (MRI), particularly in those with whiplash-associated disorders.5,6,15–21 However, the ability of MRI to identify specific soft tissue changes in persons with whiplash-associated disorders is controversial.
With many diagnostic imaging techniques available to evaluate patients with chronic neck pain, guidance is needed to prevent unnecessary studies (as demonstrated in the Clinical Example below). This article reviews the American College of Radiology (ACR) Appropriateness Criteria for chronic neck pain (Table 1).22 For each clinical scenario, the ACR Appropriateness Criteria indicate the optimal imaging study. The scenarios include patients younger than 40 years with or without a history of remote trauma, and patients of any age with a history of malignancy or remote surgery. Seven clinical scenarios were considered for these ACR Appropriateness Criteria, which included patients in whom radiographs were normal or showed cervical spondylosis, evidence of old trauma or deformity, or bony or disk margin destruction. Variants included patients with and without neurologic signs and symptoms.
| Variant (clinical scenario) | Most appropriate imaging study | RRL* |
|---|---|---|
| Patient of any age, no history of trauma | First study: five-view radiography† | |
| Patient of any age, history of malignancy | First study: five-view radiography† | |
| Patient of any age, history of surgery | First study: five-view radiography† | |
| Radiographs normal, no neurologic signs or symptoms | None recommended | O |
| Radiographs normal, neurologic signs or symptoms present | MRI | O |
| Radiographs normal, neurologic signs or symptoms present, MRI contraindicated | CT myelography | |
| Radiographs show spondylosis, no neurologic signs or symptoms | None recommended | O |
| Radiographs show spondylosis, neurologic signs or symptoms present | MRI | O |
| Radiographs show spondylosis, neurologic signs or symptoms present, MRI contraindicated | CT myelography | |
| Radiographs show previous trauma, no neurologic signs or symptoms | None recommended | O |
| Radiographs show previous trauma, neurologic signs or symptoms present | MRI | O |
| Radiographs show previous trauma, neurologic signs or symptoms present, MRI contraindicated | CT myelography | |
| Radiographs show bone or disk margin destruction | MRI | O |
| Radiographs show bone or disk margin destruction, MRI contraindicated | CT |
Clinical Example
A 52-year-old man presented with a history of progressive chronic neck pain. Ten years earlier, he had received a cross-check to the back of his head during a recreational ice hockey game. He had immediate pain that subsided after several days of treatment with heat and ibuprofen. Approximately five years later, he began experiencing stiffness in his neck in the morning that resolved after he moved around. Over the previous six months, however, the patient had a constant dull ache that responded to ibuprofen. He sought medical treatment because of paresthesias in his left hand along the distribution of the median nerve that began in the previous month.
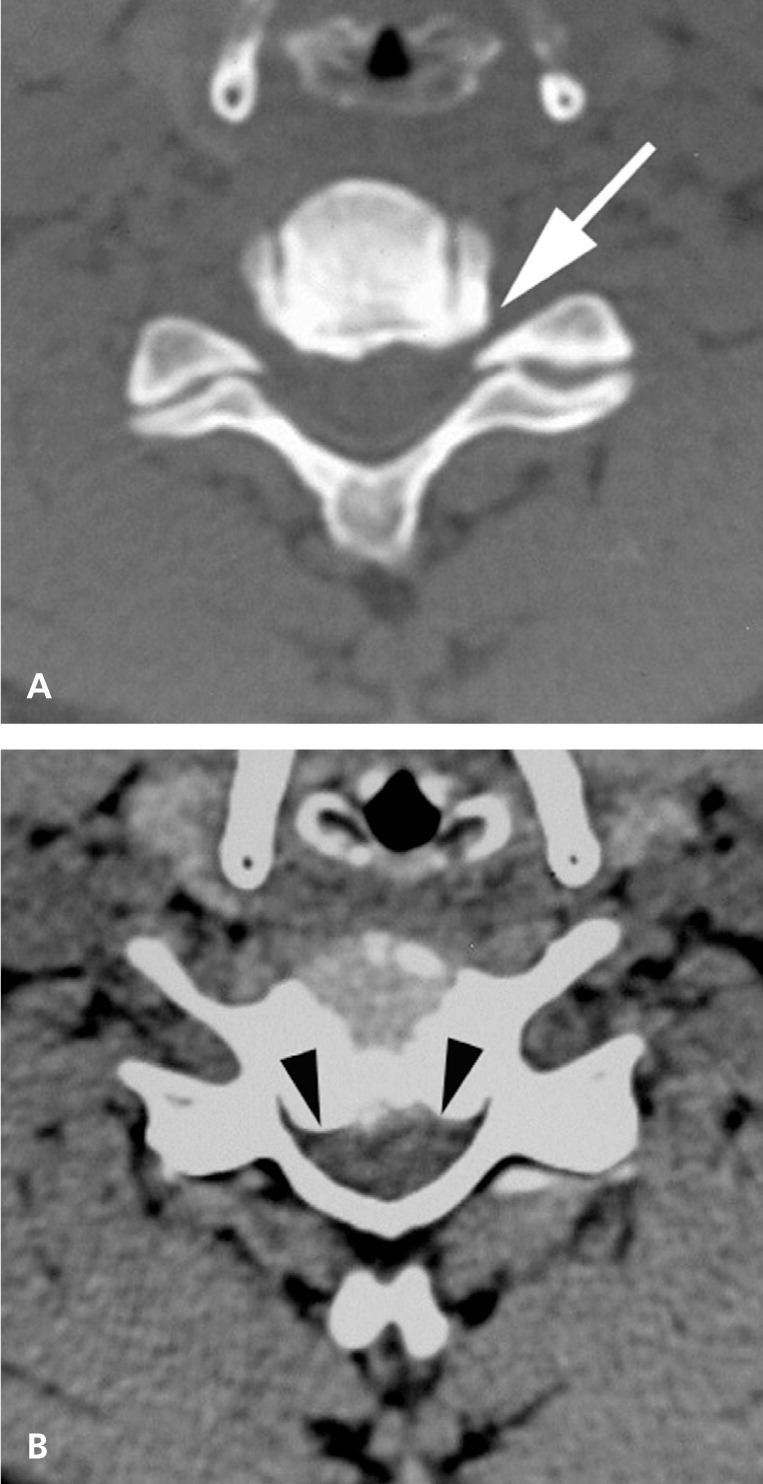
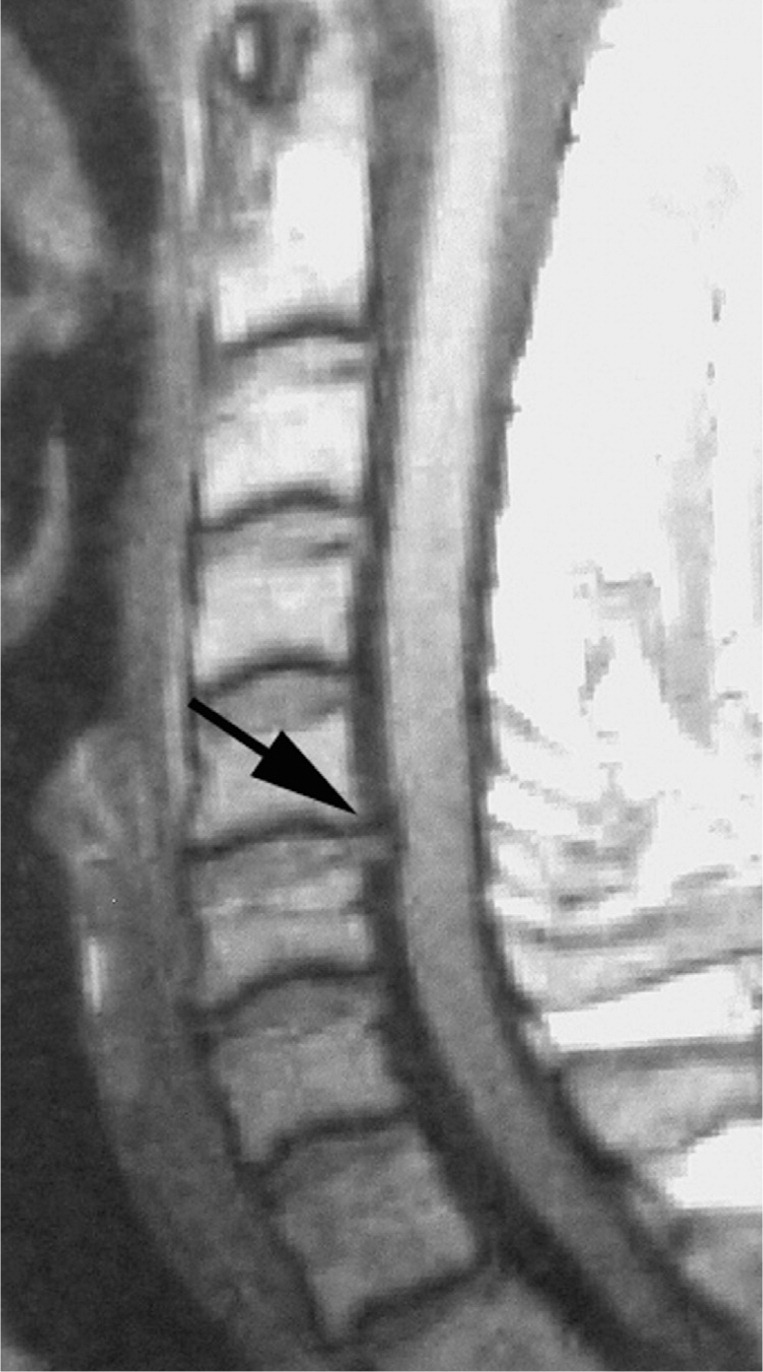
Physical examination was unremarkable, with the exception of a slight decrease in the left biceps reflex. Strength and sensory test results were normal. Initial lateral radiographs revealed narrowing of the C5-C6 disk space, and osteophytes protruding into the vertebral canal. Subsequent cervical computed tomography (CT) showed narrowing of the vertebral canal by the osteophytes (Figure 1). A cervical MRI showed a herniated disk (Figure 2). Of note, only radiography and MRI would have been indicated based on the ACR Appropriateness Criteria.
Approach to the Radiologic Evaluation of Chronic Neck Pain
For the ACR Appropriateness Criteria on chronic neck pain, the ACR Expert Panel on Musculoskeletal Imaging reviewed 27 studies of patients with chronic neck pain.22 The three largest studies evaluated 7,270,3 5,440,7 and 3,014 patients,4 respectively. One study focused only on whiplash,4 whereas the two other studies focused on the etiology of neck pain in relation to other contributing factors.3,7
In the first study, which included a representative group of Finnish adults, chronic neck syndrome occurred in 10 percent of men and 14 percent of women. Contributing factors included history of trauma, and mental and physical stress at work.3 The second study showed that disk disease is more likely to cause neck pain in men but not in women, which confirmed observations made in studies of smaller populations. The study also found that in patients with spondylosis, the presence of pain is more closely related to personality traits, neuroticism, and previous injury.7
The third study, which focused on whiplash, was a cooperative investigation using consensus methods similar to those used by the ACR. The study authors developed a flow sheet defining whiplash-associated disorders and made recommendations for diagnosis and management.4
Overall, the ACR's review found no reliable radiologic or laboratory findings to confirm or refute the diagnosis of whiplash. 22–24 Furthermore, there was little correlation between the presence of cervical spondylosis or degenerative disk disease and the severity or duration of symptoms. Although there are additional factors associated with chronic neck pain, such as personality traits and ongoing compensation claims (particularly in patients with posttraumatic neck pain), the ACR Expert Panel considered only the imaging parameters. Although spondylosis and disk disease increase with age and are usually asymptomatic, whiplash can accelerate these processes and lead to symptoms.1,18 For these reasons, no ACR Appropriateness Criteria variant specifically addresses whiplash. Rather, the variants cover specific clinical scenarios of chronic neck pain considering the etiology (trauma, arthritis, or neoplasm), radiographic findings, and presence of neurologic symptoms.
In the past, there was an increased emphasis on the use of provocative diagnostic diskography and facet joint injections for the evaluation of chronic neck pain.8,9,11–14 These techniques purportedly were indicated for patients with multilevel facet or disk disease if the offending disk or facet joint could not be identified. Facet injection, with or without arthrography, may help identify the location of the pain source. However, several studies of patients undergoing lumbar diskography have demonstrated that pain intensity during disk injection is most influenced by the emotional and psychological profile of the patient and any ongoing compensation claims.11,25,26 These studies concluded that diskography could not reliably confirm the pain source.
More recently, investigators have reported on the use of MRI for evaluating patients with chronic neck pain.5,6,15–21 Earlier studies suggest that MRI is the best method for detecting and distinguishing between the various etiologies of neck pain.5,15,16 However, more recent studies show that there is no consensus on the usefulness of MRI in evaluating the ligaments and membranes of the craniocervical junction in patients with whiplash-associated disorders.6,17–21,27,28 Krakenes and Kaale concluded that MRI can show structural changes in ligaments and membranes, and that there is a correlation between clinical impairment and morphologic findings.21 On the other hand, Kongsted and colleagues found that trauma-related MRI findings are rare in patients with whiplash-associated disorders.17 Myran and colleagues found no significant differences in the MRI findings of signal changes of the craniocervical ligaments and concluded that signal changes previously attributed to trauma are not sustainable.19 In Ichihara and colleagues' long-term study, MRI demonstrated progressive degenerative changes not associated with clinical symptoms, and the authors concluded that there is no statistically significant association between MRI findings and changes in clinical symptoms.18 Finally, a commentary reiterated the conclusions of the Task Force on Neck Pain and Its Associated Disorders that the validity of MRI in the upper cervical spine ligaments to detect acute whiplash injury has not been demonstrated.27,28
However, MRI is useful in patients with other abnormalities, including disk herniations, canal encroachment by osteophytes, tumor or infection, fractures, and posttraumatic ligament ruptures of the lower cervical column. Although MRI does not always detect the cause of chronic neck pain, particularly at the craniocervical junction, it is the preferred method for making most diagnoses.
Recommendations
A five-view radiographic examination (i.e., anteroposterior, lateral, open-mouth, and both oblique views) should initially be performed in patients of any age with chronic neck pain with or without a history of remote trauma,4 with a history of malignancy, or with a history of neck surgery in the remote past.
Patients with normal radiographic findings and no neurologic signs or symptoms need no further imaging.
Patients with normal radiographic findings and neurologic signs or symptoms should undergo MRI.5,15,16
Patients with whiplash-associated disorders should undergo MRI to evaluate for disk herniations, spur encroachment of the vertebral canal, or ligament abnormalities of the lower cervical region. The value of MRI of the craniocervical junction in patients with whiplash-associated disorders is controversial.6,17–21
If MRI is contraindicated (e.g., in patients with a cardiac pacemaker or severe claustrophobia), CT myelography with multiplanar reconstruction is recommended.
Patients with radiologic evidence of cervical spondylosis or a previous trauma without neurologic signs or symptoms need no further imaging.
Patients with radiographic evidence of cervical spondylosis or previous trauma and neurologic signs and symptoms should undergo MRI. If MRI is contraindicated, CT myelography is recommended.
Patients with radiographic evidence of bone or disk margin destruction should undergo MRI. If an epidural abscess is suspected, the examination should be performed with intravenous contrast media. CT is indicated only if MRI cannot be performed.
Facet injections and arthrography are useful for patients with multilevel disease diagnosed by any imaging modality to identify the specific disk level that is producing symptoms.
Diskography is not recommended in patients with chronic neck pain.