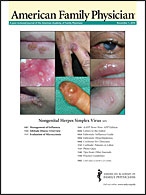
Am Fam Physician. 2010;82(9):1103-1110
Patient information: See related handout on altitude illness.
Author disclosure: Nothing to disclose.
Altitude illness affects 25 to 85 percent of travelers to high altitudes, depending on their rate of ascent, home altitude, individual susceptibility, and other risk factors. Acute mountain sickness is the most common presentation of altitude illness and typically causes headache and malaise within six to 12 hours of gaining altitude. It may progress to high-altitude cerebral edema in some persons. Onset is heralded by worsening symptoms of acute mountain sickness, progressing to ataxia and eventually to coma and death if not treated. High-altitude pulmonary edema is uncommon, but is the leading cause of altitude illness–related death. It may appear in otherwise healthy persons and may progress rapidly with cough, dyspnea, and frothy sputum. Slow ascent is the most important measure to prevent the onset of altitude illness. If this is not possible, or if symptoms occur despite slow ascent, acetazolamide or dexamethasone may be used for prophylaxis or treatment of acute mountain sickness. Descent is mandatory for all persons with high-altitude cerebral or pulmonary edema. Patients with stable coronary and pulmonary disease may travel to high altitudes but are at risk of exacerbation of these illnesses. Medical management is prudent in these patients.
Altitude illness is quite common in persons traveling to high-altitude destinations (8,200 ft [2,500 m] or above). Approximately 25 percent of travelers to Colorado ski areas, 50 percent of travelers to the Himalayas, and nearly 85 percent of those who fly directly to the Mount Everest region report symptoms of acute mountain sickness.1–3 High-altitude cerebral and pulmonary edema, the more severe types of altitude illness, are much less common than acute mountain sickness, with incidences of approximately 0.1 to 4 percent.4 Risk factors for altitude illness include rapid ascent, strenuous physical exertion, young age, living at a low altitude, and a history of altitude illness.4–8 Rapid ascent is the most important—and modifiable—risk factor.5,9–11 Recommendations for reducing the risk of altitude illness are listed in Table 1.1,2,4,7,8,11
| Recommendation | Evidence rating | References | Comments |
|---|---|---|---|
| Slow ascent is the most effective method to prevent altitude illness. | C | 5, 7–11 | Expert opinion |
| Medications for prevention and treatment of acute mountain sickness and high-altitude cerebral edema include acetazolamide and dexamethasone. | B | 8, 16–19, 29 | Small RCTs, meta-analysis |
| Descent is mandatory in persons with high-altitude cerebral or pulmonary edema. If descent is not possible, supplemental oxygen, rest, and placement in a portable hyperbaric oxygen chamber may stabilize patients. | C | 4, 7, 8, 21, 26, 27 | Expert opinion |
| Prophylaxis with salmeterol (Serevent), nifedipine (Procardia), dexamethasone, or phosphodiesterase-5 inhibitors (tadalafil [Cialis], sildenafil [Viagra]) may reduce the incidence of high-altitude pulmonary edema. | B | 24, 25 | Small RCTs |
| Uncontrolled congestive heart failure, severe chronic obstructive pulmonary disease, and pulmonary hypertension are contraindications to altitude exposure. | C | 42–44 | — |
| Activity restriction at high altitudes is not necessary in patients with stable coronary artery disease. | C | 44 | — |
| Avoid flying or driving to high altitudes unless necessary. Hiking is best because it allows for acclimatization. |
| Do not ascend if you have symptoms of altitude illness. |
| When at altitudes higher than 9,800 ft (3,000 m), sleep no more than 1,000 to 2,000 ft (300 to 600 m) above the previous night's elevation. |
| Descend if symptoms do not improve within 12 hours. |
| Be aware that persons acclimatize at different rates. |
Consensus definitions for acute mountain sickness and high-altitude cerebral and pulmonary edema were developed at the International Hypoxia Symposium, known as the Lake Louise Conference (Table 2).12,13 Scoring tools based on these criteria may be useful for trip leaders and physicians (Figure 1).14,15
| Condition | Criteria* |
|---|---|
| Acute mountain sickness | Headache and at least one of the following symptoms: fatigue or weakness; dizziness or lightheadedness; gastrointestinal symptoms (nausea or vomiting, anorexia); difficulty sleeping |
| High-altitude cerebral edema | Change in mental status or ataxia in a person with acute mountain sickness, or change in mental status and ataxia in a person without acute mountain sickness |
| High-altitude pulmonary edema | At least two of the following symptoms: dyspnea at rest; cough; weakness or decreased exercise performance; chest tightness or congestion and At least two of the following signs: crackles or wheezing in at least one lung field; central cyanosis; tachypnea; tachycardia |
Acute Mountain Sickness and High-Altitude Cerebral Edema
Although the pathophysiology of acute mountain sickness and high-altitude cerebral edema is not completely understood, current evidence suggests that hypobaric hypoxemia leads to relative fluid retention, in contrast with the usual response of marked diuresis in nonaffected climbers. This may lead to the mild cerebral edema that occurs in persons with moderate to severe acute mountain sickness and high-altitude cerebral edema. Proposed mediators of this response include vascular endothelial growth factor, nitric oxide synthase, and bradykinin.4,9
DIAGNOSIS
Symptoms of acute mountain sickness and early high-altitude cerebral edema include headache and at least one of the following: anorexia, nausea or vomiting, dizziness or lightheadedness, difficulty sleeping, and fatigue or weakness. These symptoms can easily be misinterpreted as a viral illness.12 The key criteria, however, are a recent gain in altitude and (although not specifically stated) the absence of other causes of the symptoms. Symptoms of acute mountain sickness typically occur within six to 12 hours of gaining altitude, and range from mild with spontaneous resolution (especially at altitudes less than 11,400 ft [3,500 m]) to severe with progression to high-altitude cerebral edema.4,12 High-altitude cerebral edema is considered end-stage acute mountain sickness and is defined by ataxia (as assessed by heel-to-toe walking) or altered mental status, usually in a person with acute mountain sickness.6,7,12 High-altitude cerebral edema can progress in a matter of hours from mild ataxia to coma and death.7
PREVENTION AND TREATMENT
The most accepted method of preventing acute mountain sickness and high-altitude cerebral edema is to ascend slowly. However, many climbers have difficulty following this advice. The general rule of thumb for persons at altitudes higher than 9,800 ft (3,000 m) is not to sleep more than 1,000 to 2,000 ft (300 to 600 m) above the previous night's elevation.7
Acetazolamide, a carbonic anhydrase inhibitor, may be used as prophylaxis8; it should be started at least one day before climbing and continued until acclimatization at the highest sleeping elevation (Table 33,7,16–29 ). Although a systematic review in 2001 found that lower dosages are not effective, more recent studies support the use of 125 mg twice daily for prophylaxis.16,17,29 Adverse effects may include paresthesias (common), mild diuresis, and an aversion to carbonated beverages because of the inhibition of salivary carbonic anhydrase. Acetazolamide is contraindicated in persons with sulfa allergies.
| Medication | Indication | Typical dosage | |
|---|---|---|---|
| Acetazolamide | Prevention and treatment of acute mountain sickness (first-line therapy)* | 125 mg twice daily (prophylaxis) 250 mg twice daily (treatment) | |
| Dexamethasone | Prevention of acute mountain sickness† | 4 mg every 6 to 12 hours | |
| Treatment of acute mountain sickness† | 4 mg every 6 hours | ||
| Prevention of high-altitude cerebral edema† | 4 mg every 6 hours | ||
| Treatment of high-altitude cerebral edema†‡ | 8 mg, then 4 mg every 6 hours | ||
| Nifedipine (Procardia) | Prevention and treatment of high-altitude pulmonary edema† | 20 mg every 8 to 12 hours | |
| Salmeterol (Serevent) | Prevention and treatment of high-altitude pulmonary edema† | 125 mcg every 12 hours | |
| Sildenafil (Viagra) | Prevention and treatment of high-altitude pulmonary edema† | 20 mg every 6 to 8 hours | |
| Tadalafil (Cialis) | Prevention and treatment of high-altitude pulmonary edema† | 10 mg every 12 hours | |
Dexamethasone is also effective for prophylaxis and treatment of acute mountain sickness as a second-line agent, but it does not assist in acclimatization and therefore may lead to rebound acute mountain sickness when it is discontinued.18,19 A small study showed that low-dose theophylline is also beneficial for prevention of acute mountain sickness.20
Treatment of high-altitude cerebral edema starts with immediate descent, if possible. Descent of 1,000 ft (300 m) may be all that is required.4,7 If descent is not possible (e.g., because of weather conditions), supplemental oxygen should be administered, and the patient should be placed in a portable hyperbaric oxygen chamber until descent is possible.21 Portable hyperbaric chambers are fairly lightweight and are typically carried by high-altitude rescue teams. They may be used on major expeditions, and are often available at rescue stations. Dexamethasone should also be given until descent is possible and until symptoms have resolved.8
Ginkgo has been studied for prophylaxis and treatment of acute mountain sickness and high-altitude cerebral edema, but results are varied, and it is not recommended.22,23 Although descent and treatment are not required for persons with mild acute mountain sickness, persons with moderate to severe sickness should be treated as if they have early high-altitude cerebral edema.
High-Altitude Pulmonary Edema
The pathophysiology of high-altitude pulmonary edema is not completely understood, but the primary mechanism is thought to be exaggerated hypoxic pulmonary vasoconstriction that causes increased pulmonary capillary pressure.30 Elevated pulmonary capillary pressure leads to mechanical disruption of the pulmonary capillaries and subsequent extravasation of fluid into the interstitial and alveolar spaces without inflammation.31,32 Limited availability of nitric oxide may increase pulmonary arterial pressure, and impaired sodium and water transportation within the lung may also contribute to the pathophysiology.24,25
INCIDENCE AND RISK FACTORS
The incidence of high-altitude pulmonary edema in unacclimatized mountaineers at 15,000 ft (4,600 m) is approximately 4 percent.33 As with acute mountain sickness and high-altitude cerebral edema, risk factors for the development of high-altitude pulmonary edema include individual susceptibility, history of altitude illness, rapid ascent, altitude attained, and strenuous physical exertion.4,7,31,33 Acute mountain sickness is not a prerequisite for the development of high-altitude pulmonary edema.34
DIAGNOSIS
High-altitude pulmonary edema often develops overnight, approximately one to four days after rapid ascent to altitudes above 8,000 ft (2,400 m).35 Affected persons may initially report fatigue, weakness, dyspnea, decreased exercise tolerance, and delayed recovery from exertion. Physical signs include frothy sputum with associated cough, cyanosis, rales, reduced oxygen saturation, tachypnea, and tachycardia.36 When high-altitude pulmonary edema is clinically suspected, decreased oxygen saturation (as measured by portable pulse oximetry, which is generally available at support camps) may confirm the diagnosis. If available, chest radiographs may show asymmetric patchy infiltrates in variable locations.35
PREVENTION AND TREATMENT
High-altitude pulmonary edema is the leading cause of death from altitude illness, but it is avoidable with careful ascent and reversible with early recognition and treatment. Small randomized trials have shown that when started one day before ascent, prophylactic dexamethasone, nifedipine (Procardia), salmeterol (Serevent), and phosphodiesterase-5 inhibitors (tadalafil [Cialis], sildenafil [Viagra]) reduce the incidence of high-altitude pulmonary edema in persons with a history of the condition, whereas acetazolamide does not.24,25,35,37 No comparative studies have shown one type of prophylactic agent to be superior to another.
Case reports consistently show that supplemental oxygen, relative rest, and descent lead to improvement in persons with high-altitude pulmonary edema.26 Immediate descent is the treatment of choice. Supplemental oxygen may be administered if available, and simulated descent by placing the patient in a portable hyperbaric chamber may be helpful temporarily. When descent is not possible, limited evidence suggests that treatment with acetazolamide, bed rest, nifedipine, supplemental oxygen, salmeterol, or phosphodiesterase-5 inhibitors may improve oxygen saturation and pulmonary edema.27 There is no strong evidence that medications improve outcomes or facilitate resolution of high-altitude pulmonary edema better than descent alone.
Other High-Altitude Medical Conditions
A dry cough in the absence of other symptoms of high-altitude pulmonary edema is common at high altitudes, and can be severe enough to cause extreme discomfort or rib fractures. The cause of high-altitude bronchitis and cough is likely multifactorial, consisting of a combination of irritation of the respiratory cilia and mucosa, rhinorrhea resulting in mouth breathing, bronchoconstriction, respiratory tract infection, and minimal amounts of pulmonary edema. Breathing through a face mask or sucking on candy is recommended to alleviate cough.28
Peripheral edema, which rarely signals significant disease, is also associated with high altitudes. It is usually transient, resolves with descent, and can be controlled with diuretics, if needed.38
High-altitude retinopathy is a common, typically benign condition that is thought to be caused by increased retinal blood flow in response to hypoxic conditions at altitudes above 16,400 ft (5,000 m).38 Although usually asymptomatic, it may be associated with other altitude-related illnesses and may predict acute mountain sickness and high-altitude cerebral and pulmonary edema. Ultraviolet keratitis (snow blindness), which results from corneal epithelial injury from ultraviolet radiation exposure, is another common condition at high altitudes, and may be disabling. Wearing ultraviolet-protectant sunglasses with large lenses and side shields is recommended when traveling in snowy conditions at high altitudes. Treatment is aimed at decreasing pain and preventing infection while the corneal epithelium heals. Medications include nonsteroidal anti-inflammatory drugs and other analgesics, ophthalmic antibiotics, and topical cycloplegics. Ophthalmic nonsteroidal anti-inflammatory drugs are effective analgesics for corneal abrasions and do not interfere with the healing process.39,40 Contact lenses, if used, should be removed, and the affected eye is often patched. Climbers who have undergone radial keratotomy are at risk of severe and sudden refractive shift; however, persons who have had photorefractive keratectomy do not seem to be at risk.41
Acute Altitude Exposure and Chronic Illness
Chronic medical conditions may worsen as elevation increases and arterial oxygen saturation decreases. Therefore, certain conditions (e.g., pulmonary hypertension, severe chronic obstructive pulmonary disease, uncontrolled congestive heart failure) are contraindications to high altitudes42 (Table 44,7,41–45 ). With the exception of chronic obstructive pulmonary disease, these conditions do not increase the risk of acute mountain sickness.43
| Condition | Recommendation |
|---|---|
| Arrhythmias | There is a lower threshold for increased incidence of arrhythmias at high altitudes; provide supplemental oxygen and limit activity. |
| Asthma | Exacerbation does not seem to be related to altitude; continue usual treatment. |
| Chronic obstructive pulmonary disease | Risk is dependent on disease severity; consider pulse oximetry and adjust supplemental oxygen as needed. |
| Patients with severe disease should not travel to high altitudes. | |
| Congestive heart failure | Risk of decompensation depends on disease severity, activity level, and elevation; supplemental oxygen may need to be increased. |
| Patients with symptoms should use caution with any change in altitude; patients with uncompensated congestive heart failure should not travel to high altitudes. | |
| Coronary artery disease | Individualized evaluation is necessary; provide appropriate chemoprophylaxis (e.g., dexamethasone, acetazolamide); consider exercise stress testing before ascent. |
| Patients should acclimatize properly, and should be able to recognize symptoms of angina, acute mountain sickness, high-altitude pulmonary edema, and high-altitude cerebral edema. | |
| Hypertension | Mild, transient elevations in blood pressure are expected and do not require treatment; maintain blood pressure control at sea level and continue all medications. |
| Pulmonary hypertension | Travel to high altitudes is contraindicated in patients with pulmonary hypertension because of the hypoxic environment and risk of high-altitude pulmonary edema; if travel is necessary, calcium channel blockers, isoproterenol, and supplemental oxygen may be beneficial. |
| Sickle cell disease | Travel to high altitudes is contraindicated because of the increased incidence of splenic infarct and sickle cell crisis. |
Changes in barometric pressure also affect persons with pre-existing hypertension, coronary artery disease, and arrhythmias. Despite the additional stress that high altitudes pose to the cardiovascular system, activity restriction is not justified in patients with stable coronary artery disease.44,45 Acute mountain sickness, high-altitude cerebral edema, and high-altitude pulmonary edema can exacerbate cardiovascular instability; informing patients about the warning signs of these conditions is important. Proper acclimatization and appropriate prophylaxis are advised.43,44
Diabetes mellitus, especially type 1 diabetes, presents a unique challenge to the physician counseling a patient traveling to a high altitude. Although there is no increased risk of altitude illness in climbers with diabetes, they must be aware of the potential for glycemic management issues that can be complicated by being in a remote—and often very cold—environment. Glucose meters may not function properly at high altitudes or in cold environments.48