
Am Fam Physician. 2011;83(4):417-422
Patient information: See related handout on adhesive capsulitis, written by the author of this article.
Author disclosure: Nothing to disclose.
Adhesive capsulitis is a common, yet poorly understood, condition causing pain and loss of range of motion in the shoulder. It can occur in isolation or concomitantly with other shoulder conditions (e.g., rotator cuff tendinopathy, bursitis) or diabetes mellitus. It is often self-limited, but can persist for years and may never fully resolve. The diagnosis is usually clinical, although imaging can help rule out other conditions. The differential diagnosis includes acromioclavicular arthropathy, autoimmune disease (e.g., systemic lupus erythematosus, rheumatoid arthritis), biceps tendinopathy, glenohumeral osteoarthritis, neoplasm, rotator cuff tendinopathy or tear (with or without impingement), and subacromial and subdeltoid bursitis. Several treatment options are commonly used, but few have high-level evidence to support them. Because the condition is often self-limited, observation and reassurance may be considered; however, this may not be acceptable to many patients because of the painful and debilitating nature of the condition. Nonsurgical treatments include analgesics (e.g., acetaminophen, nonsteroidal anti-inflammatory drugs), oral prednisone, and intra-articular corticosteroid injections. Home exercise regimens and physical therapy are often prescribed. Surgical treatments include manipulation of the joint under anesthesia and capsular release.
Adhesive capsulitis is a common, painful condition of the shoulder that is associated with loss of range of motion in the glenohumeral joint. It results from contraction of the glenohumeral joint capsule and adherence to the humeral head.1,2 The term “frozen shoulder” commonly used to describe adhesive capsulitis and other conditions associated with loss of range of motion at the joint. Although adhesive capsulitis is often self-limited, it can persist for years and may never fully resolve.
Adhesive capsulitis has traditionally been characterized as primary (idiopathic), or secondary (resulting from an underlying condition). Its incidence as a primary, isolated entity may not be as high as previously thought. The orthopedic literature emphasizes diagnosis and treatment of concomitant conditions, such as diabetes mellitus, rotator cuff tendinopathy or tear, subacromial bursitis, biceps tendinopathy, recent shoulder surgery or trauma, and inflammatory diseases.3–5
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Acetaminophen, nonsteroidal anti-inflammatory drugs, and rehabilitation are commonly used to treat adhesive capsulitis. However, there is a lack of high-level evidence to support their use. | B | 21, 24, 25 |
| Oral corticosteroids provide short-term pain relief and improve range of motion in patients with adhesive capsulitis, but the effect may not extend beyond six weeks. | B | 22, 23 |
| Compared with oral glucocorticoid therapy, intra-articular corticosteroid injections provide better short-term pain relief and improved range of motion in patients with isolated adhesive capsulitis. However, the effect may not extend beyond six weeks. | B | 25, 27, 28 |
| Radiographically guided capsular distension, with or without corticosteroid injection, provides short-term benefit in the treatment of adhesive capsulitis. Its effectiveness is similar or superior to manipulation under anesthesia, and carries less risk. | B | 32, 33 |
| Acupuncture may be helpful in the treatment of shoulder pain, but further study is needed before it can be recommended for treatment of adhesive capsulitis. | B | 34 |
Epidemiology
The incidence of adhesive capsulitis is approximately 3 percent in the general population.6,7 It is rare in children,8 and peaks between 40 and 70 years of age.7 Women are more often affected than men, but there is no known genetic or racial predilection. It is common in persons with insulin-dependent and non-insulin-dependent diabetes, and in those with prediabetes (glucose intolerance).6,7
Persons with a history of adhesive capsulitis are at increased risk of developing the condition on the contralateral side. Recurrence on the affected side is also possible, especially in patients with diabetes.
Pathophysiology and Natural History
The pathophysiology of adhesive capsulitis is poorly understood. Analysis of surgical specimens suggests that capsular hyperplasia and fibrosis have a role. The presence of cytokines suggests a possible autoimmune process, but the relationship is not well established.9
Adhesive capsulitis has been described as having three sequential phases: a painful stage, a freezing stage, and a thawing or recovery stage. There is, however, no evidence to validate this classification, and its clinical utility is questionable. Pain and limited range of motion can occur in all phases of adhesive capsulitis, which often does not follow a stepwise course. Pain and decreased range of motion can persist for one to two years,10–13 and up to 10 percent of patients never recover full range of motion. However, this loss of motion is seldom functionally limiting.2
Clinical Presentation
The hallmark of adhesive capsulitis is decreased range of motion and shoulder pain. There often is no identifiable cause or trigger. The pain is often described as a poorly localized, deep ache. If the pain is localized, it is usually in the area of the anterior or posterior capsule. The pain may radiate to the biceps area. Patients may have progressive pain and stiffness when reaching overhead, away, and behind the back. Weakness is often related to pain or concomitant tendinopathy. Crepitus may be present on the involved side. As with many shoulder conditions, pain may impair sleep. Unlike more serious causes of shoulder pain, adhesive capsulitis does not cause red flag symptoms such as fever, night sweats, and unexplained weight loss. Neuropathic symptoms in the forearm and hand suggest another diagnosis, such as cervical radiculopathy.
Differential Diagnosis
The diagnosis of adhesive capsulitis is usually clinical. Other conditions that should be considered in a patient who presents with a stiff, painful shoulder include acromioclavicular arthropathy, autoimmune disease (e.g., systemic lupus erythematosus, rheumatoid arthritis), biceps tendinopathy, glenohumeral osteoarthritis, neoplasm, rotator cuff tendinopathy or tear (with or without impingement), cervical disk degeneration, and subacromial and subdeltoid bursitis. Table 1 includes conditions that can mimic adhesive capsulitis, but may also occur concomitantly. Adhesive capsulitis in the presence of associated conditions is most appropriately described as painful shoulder syndrome.
| Condition | Distinguishing physical examination findings | Distinguishing historical findings | Diagnostic tests |
|---|---|---|---|
| Acromioclavicular arthropathy | Positive cross-arm adduction and compression testing; glenohumeral range of motion is preserved | Localizes over acromioclavicular joint (superiorly); history of repetitive overuse (e.g., weight lifting) | Plain radiography |
| Autoimmune disease (e.g., systemic lupus erythematosus, rheumatoid arthritis) | Malar rash; synovitis (tenderness and effusions) in other joints | Multisystem involvement; multiple joints involved | Antinuclear antibody testing; rheumatoid factor test |
| Biceps tendinopathy | Tenderness over long head of the biceps tendon; positive Speed or Yergason test | Localizes anteriorly | MRI (radiography may determine whether calcifications are present) |
| Cervical disk degeneration | Limited range of motion in neck and pain with active movement; intrinsic hand weakness; impaired light touch | Localizes posteriorly; hand numbness and weakness in radiculopathy | Cervical spine radiography |
| Glenohumeral osteoarthritis | Similar to adhesive capsulitis; shoulder girdle atrophy may be present | History of shoulder trauma or surgery; older age | Plain radiography |
| Neoplasm | Similar to adhesive capsulitis | Fevers, night sweats, unexplained weight loss (if advanced); dyspnea or cough (if Pancoast tumor present) | Plain radiography, MRI |
| Rotator cuff tendinopathy or tear, with or without impingement | Passive range of motion is preserved; painful arc, focal tenderness, positive Hawkins and Neer tests | Possible history of repetitive overuse; often localizes anteriorly or laterally | MRI (radiography may determine whether calcifications are present) |
| Subacromial and subdeltoid bursitis | Passive range of motion is preserved | Possible history of repetitive overuse | Diagnostic subacromial lidocaine (Xylocaine) injection, MRI |
Physical Examination
The challenges in diagnosing adhesive capsulitis are differentiating true glenohumeral loss of motion from pain-related guarding, and identifying any concomitant conditions.
Patients with advanced adhesive capsulitis may have lost the natural arm swing that occurs with walking. Muscle atrophy of the shoulder girdle may be present. As a result of impaired motion in the glenohumeral joint, abnormal scapular movement may be observed with active forward flexion of the affected shoulder. The physical examination of a patient with adhesive capsulitis can be uncomfortable, and the patient may need to briefly rest or gently “shake out” the shoulder between maneuvers.
Palpation may yield vague, diffuse tenderness over the anterior and posterior shoulder. Focal tenderness over a specific structure is rare; its presence suggests another diagnosis or concomitant pathology, such as rotator cuff or biceps tendinopathy.
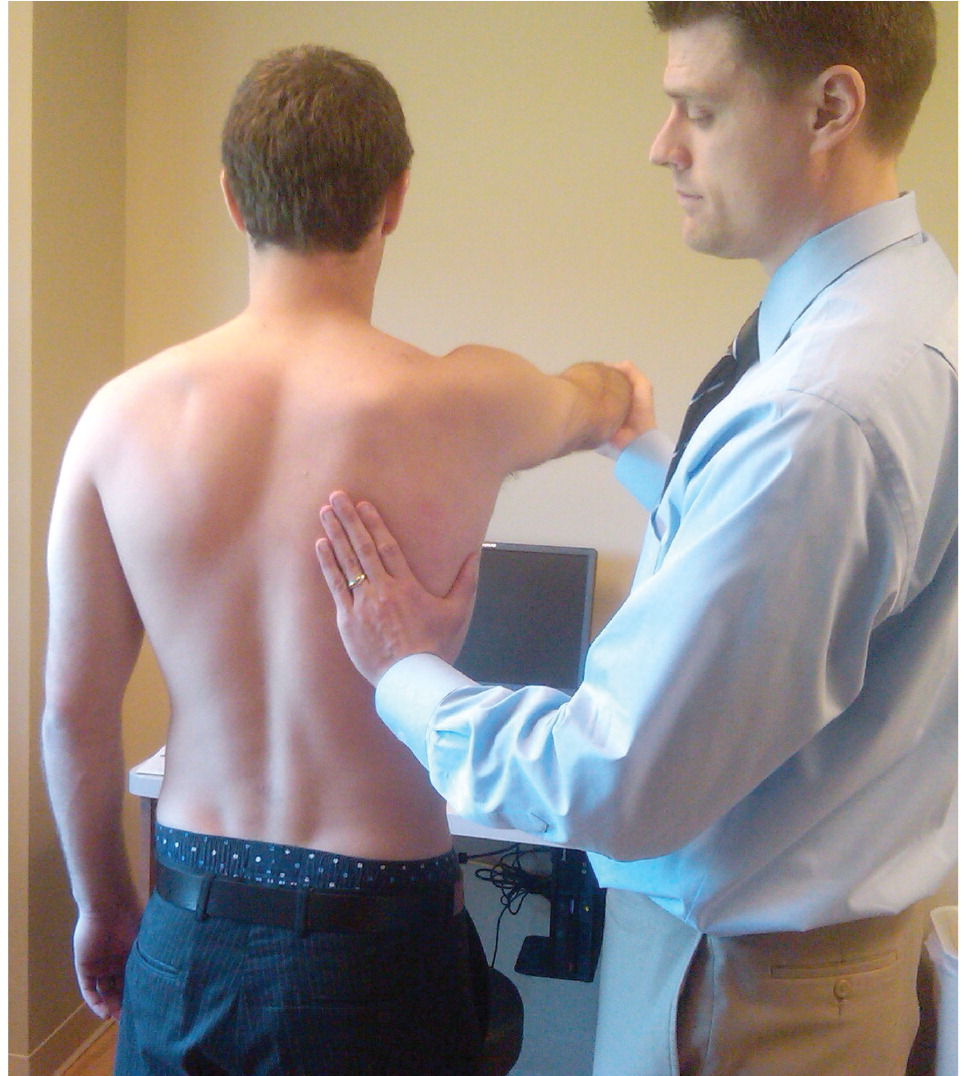
Loss of motion with forward flexion, abduction, and external and internal rotation should raise suspicion for adhesive capsulitis. It is important to compare these maneuvers on the affected and unaffected sides to accurately assess deficits. The patient should initially be asked to actively test the limits of motion (Figure 1); if loss of motion is observed, the physician may assist passively, with scapular stabilization to ensure an accurate measurement of movement (Figure 2). The most widely accepted method for measuring internal rotation is the Apley scratch test, usually expressed in terms of the highest vertebral level reached (Figure 3). Full range of motion in any plane suggests another diagnosis.


Because adhesive capsulitis does not affect the dynamic stabilizers of the shoulder (i.e., rotator cuff, biceps tendon, and deltoid muscle), strength should theoretically be preserved in all planes. However, patients with adhesive capsulitis may not have enough range of motion to perform strength testing. Resisted strength testing can result in pain-related “breakaway” weakness that mimics true weakness. Patients with advanced adhesive capsulitis may also have muscular atrophy that can cause weakness.
Testing should be performed to assess for other conditions, such as acromioclavicular arthropathy (cross-arm adduction and compression testing), rotator cuff tendinopathy and impingement (Hawkins and Neer tests), and biceps tendinopathy (Yergason and Speed tests).2,14–16 Video demonstrations of these tests are available at http://www.youtube.com/watch?v=2mSv7gLXyYg (Hawkins test); http://www.youtube.com/watch?v=k21FNtBjQ14 (Neer test); http://www.youtube.com/watch?v=rQ2Mp6aSi88 (Yergason test); and http://www.youtube.com/watch?v=N00gA4Pvsbw (Speed test). Neurovascular testing should be performed on the upper extremity of the involved side to rule out neurologic conditions such as cervical radiculopathy. Palpation and range-of-motion testing of the cervical spine should also be performed.
Diagnostic Testing
LABORATORY TESTING
Because of the high prevalence of diabetes and prediabetes in patients with adhesive capsulitis, physicians should consider fasting glucose testing in patients who have not been diagnosed with diabetes. Additional serologies are usually not indicated, but may be performed if autoimmune or infectious conditions are suspected. Erythrocyte sedimentation rate and C-reactive protein levels may be elevated in patients with primary adhesive capsulitis, but these tests are not sensitive or specific.17
IMAGING
Definitive diagnosis of adhesive capsulitis is achieved only through direct surgical observation. However, this is not usually necessary; other imaging modalities can be used to supplement the history and physical examination.
The glenohumeral joint capsule is comprised of soft tissue and is therefore not visible on plain radiography. However, radiography can rule out other conditions and detect concomitant pathology; it is also useful to assess for Pancoast tumors, advanced glenohumeral arthritis, pathologic fracture, avascular necrosis, and calcific rotator cuff and biceps tendinopathy.
Magnetic resonance imaging is not diagnostic for adhesive capsulitis, but can be helpful in identifying other conditions, such as rotator cuff tendinopathy and subacromial bursitis. Capsular thickening can sometimes be observed on magnetic resonance imaging in patients with adhesive capsulitis18–20 (Figure 4).

Treatment
There is no high-level evidence to support or refute many of the commonly used treatments for adhesive capsulitis. Because the condition is often self-limited, observation and reassurance alone can be considered for patients in whom concomitant conditions have been excluded. However, patients should be counseled that it may take many months (or even years) to resolve. The painful and debilitating nature of adhesive capsulitis makes this option unacceptable for many patients.
NONSURGICAL TREATMENT
Most patients with adhesive capsulitis will recover with nonsurgical treatment. Immobilization should be avoided. The best initial treatment depends on the duration and severity of the condition.
Acetaminophen and nonsteroidal anti-inflammatory drugs are first-line options for pain relief in patients with no contraindications. However, there is little evidence of their effectiveness. One systematic review of nonsteroidal anti-inflammatory drugs for painful shoulder conditions (not only adhesive capsulitis) showed significant improvement compared with placebo, but because the studies were generally small and of poor or moderate quality, these results are of questionable clinical relevance.21 For more severe cases, a tapering course of oral prednisone is often prescribed, usually over two to three weeks. Starting dosages typically range from 40 to 60 mg per day, and are tapered by 10 mg every four to seven days. Oral corticosteroids provide short-term benefit in pain relief and improved range of motion (up to six weeks) in patients with adhesive capsulitis, but they have not been proven to shorten the duration of the condition.22,23
Rehabilitation, as a home exercise program or physical therapy, has traditionally been a cornerstone of treatment for adhesive capsulitis. However, there are no high-level studies that clearly demonstrate benefit over observation or medical therapy alone.24 Physical therapy in conjunction with corticosteroid injections is more effective than physical therapy alone.25 Aggressive physical therapy can exacerbate pain and diminish adherence to the treatment plan; therefore, caution should be used in patients who have a high degree of pain and stiffness. Initial therapy typically includes gentle range-of- motion exercises, although evidence is lacking. Other therapies, such as ultrasound, massage, iontophoresis, and phonophoresis, have not been proven effective for adhesive capsulitis.26
Subacromial corticosteroid injection can be considered if concurrent rotator cuff or subacromial bursitis is suspected. Compared with oral glucocorticoid therapy, intra-articular corticosteroid injections provide better short-term pain relief and improved range of motion in patients with isolated adhesive capsulitis.25,27,28 However, this effect may not extend beyond six weeks. Because the glenohumeral joint lies deep within the shoulder, correct technique and placement can be challenging. Ultrasound guidance may be helpful to ensure correct placement. There is evidence to support the use of up to three injections over the course of four months without significant risk of complications.29
Another treatment option for patients with adhesive capsulitis is radiographically guided capsular distension with saline, with or without corticosteroid injection. This treatment is as effective or better than manipulation under anesthesia, and carries less risk. However, the benefit may not last beyond six to 12 weeks.30–33
There is limited evidence that acupuncture can improve pain and function for two to four weeks in patients with shoulder pain, but there is no definitive evidence of benefit in patients with adhesive capsulitis.34
SURGERY
Patients with adhesive capsulitis who have little or no improvement after six to 12 weeks of conservative treatment and who cannot tolerate their symptoms should be referred to an orthopedic surgeon. Those who improve but then plateau at an unacceptable level after longer courses of nonsurgical therapy can also be considered for surgical referral.
Surgical options for adhesive capsulitis include joint manipulation under anesthesia and capsular release. Manipulation involves placing the patient under general anesthesia and manipulating the humerus to disrupt adhesions. There is moderate evidence that this alleviates pain and facilitates recovery of motion when it is followed by early physical therapy.35,36 Manipulation under anesthesia is associated with a risk of iatrogenic proximal humeral fracture, glenohumeral dislocation, and rotator cuff tearing. It generally should be avoided in patients with osteoporosis or significant osteopenia, with a history of glenohumeral instability, or who have previously undergone manipulation with subsequent recurrence.
