
Am Fam Physician. 2011;83(6):753-754
Author disclosure: Nothing to disclose.
A 50-year-old woman presented with a plaque on her thigh that had been slowly growing for several months. It was mildly pruritic and scaly, and sometimes appeared irritated. The patient was treated with clotrimazole 1% (Lotrimin) compounded with betamethasone dipropionate 0.05%, applied twice daily for more than three months. This preparation relieved the pruritus, but did not resolve the plaque. She had no personal or family history of psoriasis or atopic dermatitis. She was taking no other medications and was otherwise healthy.
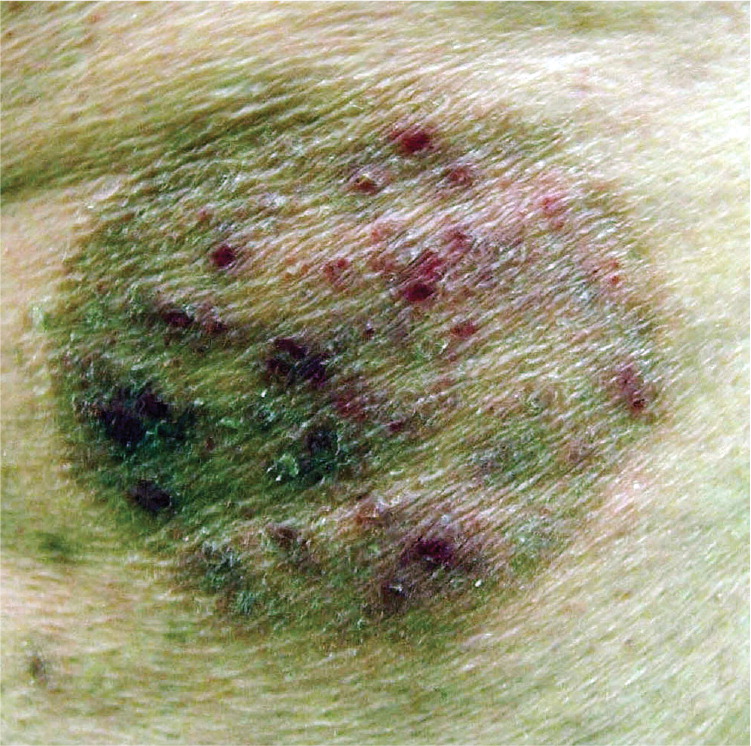
Examination revealed a 5 × 7 -cm erythematous plaque with a raised, scaly border (Figure 1). The central portion of the plaque had scattered, follicularly based, erythematous papules and postinflammatory hyperpigmentation. A potassium hydroxide (KOH) preparation of scale from the plaque revealed innumerable branching hyphae. The patient began a four-week course of topical econazole cream twice daily. The scaling resolved by the end of the treatment, but multiple erythematous papules remained within the affected area (Figure 2).

Question
Discussion
The answer is C: Majocchi granuloma. A Majocchi granuloma is caused by the invasion of follicles by a dermatophyte. It leads to a well-circumscribed, annular plaque that is sometimes boggy or crusty, with overlying pustules. Majocchi granuloma can appear anywhere, but usually occurs on the shins or wrists. It is associated with occluded areas, shaving, or topical steroid use.
During the course of treatment, the patient developed the granuloma because of inappropriately potent topical steroids used to treat dermatophyte infection.1,2 This has also been called tinea incognito because of the lack of classical findings, such as peripheral scale. The potent steroid blunts the host response, allowing the fungus to grow and invade the follicles despite the presence of the antifungal. Potent topical steroid use may lead to other potential complications, including steroidinduced atrophy and perioral dermatitis.3,4
To fully treat follicular dermatophyte infections, systemic antifungals, such as terbinafine (Lamisil), griseofulvin, or itraconazole (Sporanox), are necessary. Topical antifungals are unable to adequately penetrate the follicle. Superficial dermatophyte infections that do not affect the follicles usually respond to appropriate treatment using a topical antifungal alone.5 If pruritus is the main symptom, an over-the-counter, menthol-containing lotion or cream can be added.
An allergic response to a medication is an important consideration when the dermatitis seems resistant; however, it is uncommon for allergic contact dermatitis to have a follicular pattern—it is more commonly eczematous in appearance.4 Allergic contact dermatitis is usually a localized, but sometimes generalized, eczematous or morbilliform eruption. Vesicles may be present. Other morphologies—rarely urticarial—sometimes occur.
Bacterial folliculitis can occasionally cause pruritus, but it is more often painful.4 A localized, annular pattern would be an unusual presentation for bacterial folliculitis. Bacterial folliculitis causes follicular papules and pustules that can occur anywhere on the body, but usually on the scalp or extremities. The condition is often caused by staphylococcal species, but can be caused by gram-positive and gram-negative organisms.
Pityrosporum folliculitis, or Malassezia folliculitis, is not annular. It usually occurs on the upper back and chest, and less commonly on the face and scalp. The condition leads to mild to moderately pruritic, dome-shaped follicular papules and pustules. It is caused by commensal yeast that has overgrown and invaded the follicles. Like Majocchi granuloma, it is often unresponsive to topical antifungals alone and may require systemic treatment.4
Steroid-induced acne is typically caused by systemic steroid use, but can occasionally be caused by inhaled or topical formulations. Classically, it presents as a monomorphous acneiform eruption with small, firm, follicular papules, usually on the forehead, cheeks, and chest.4
| Condition | Characteristics |
|---|---|
| Allergic contact dermatitis | Localized (sometimes generalized), eczematous or morbilliform eruption; vesicles may be present; other morphologies—rarely urticarial—sometimes occur |
| Bacterial folliculitis | Follicular, painful papules and pustules; usually occurs on the scalp or extremities; often caused by staphylococcal species, but can be caused by gram-positive and gram-negative organisms |
| Majocchi granuloma | Well-circumscribed annular plaque; sometimes boggy and crusted, with overlying pustules; usually occurs on the shins or wrists; associated with occluded areas, shaving, or topical steroid use |
| Pityrosporum folliculitis | Mild to moderately pruritic, dome-shaped follicular papules and pustules; usually occurs on the upper back and chest, and less commonly on the face and scalp |
| Steroid-induced acne | Small, firm, follicular papules; usually occurs on the forehead, cheeks, and chest; commonly associated with systemic steroids, and occasionally inhaled or topical steroids; resolves with discontinuation of causative steroid |
