
Am Fam Physician. 2011;83(7):786-792
Author disclosure: Nothing to disclose.
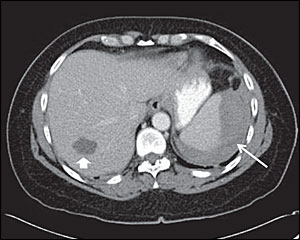
to the editor: A 56-year-old woman presented to the emergency department with left-sided pleuritic chest pain and upper abdominal pain that began the previous day after a reportedly uneventful diagnostic colonoscopy for occult blood positivity. The colonoscopy was done under propofol sedation and the only abnormal finding was mild diverticulosis of the left colon. On presentation to the emergency department, vital signs were normal and physical examination was notable for obesity and mild tenderness to palpation in the left upper abdominal quadrant. Laboratory tests revealed a hemoglobin level of 11.4 g per dL (114 g per L), International Normalized Ratio of 0.95, normal white blood cell and platelet counts, and normal blood chemistries. Computed tomography (CT) of the abdomen and pelvis with contrast (see accompanying figure) revealed a large splenic hematoma and an incidental hepatic cyst. She was treated conservatively and her symptoms gradually improved. A follow-up CT scan three days later showed no progression of the hematoma.
Splenic injury during colonoscopy is uncommon but can lead to splenic hematoma, splenic rupture, hemoperitoneum, and potentially death. Patients typically present within hours to several days after the procedure with abdominal pain and symptoms of hemodynamic instability.1 Possible predisposing factors include adhesions involving the splenocolic ligaments, splenomegaly, looping at the splenic flexure, excessive externally applied abdominal pressure, female sex, rapid completion time, smoking, propofol sedation, inadequate colon cleansing, and aspirin use.1–3 Imaging modalities such as ultrasonography and CT scan of the abdomen and pelvis with contrast are typically diagnostic.1,4 Based on the extent of the splenic injury and hemodynamic status, conservative management, splenic artery embolization, or surgical interventions are reported to be effective.1–5
Diagnosis of colonoscopy-associated splenic injury requires a high index of clinical suspicion and prompt abdominal imaging in a patient with unexplained abdominal pain or symptoms of hemodynamic instability after colonoscopy. It is important that colonoscopists, including family physicians who perform this procedure,6 recognize colonoscopy-associated splenic injury in a timely manner.
