
Am Fam Physician. 2011;84(2):204-210
Patient information: See related handout on hemorrhoids, written by the authors of this article.
Author disclosure: No relevant financial affiliations to disclose.
Most patients with hemorrhoids experience only mild symptoms that can be treated with nonprescription topical preparations. Patients usually seek treatment when symptoms increase. Internal hemorrhoids typically present with prolapse or painless rectal bleeding. External hemorrhoids also bleed and can cause acute pain if thrombosed. Medical therapy should be initiated with stool softeners plus local therapy to relieve swelling and symptoms. If medical therapy is inadequate, surgical intervention is warranted. Rubber band ligation is the treatment of choice for grades 1 and 2 hemorrhoids. Rubber band ligation, excisional hemorrhoidectomy, or stapled hemorrhoidopexy can be performed in patients with grade 3 hemorrhoids. Rubber band ligation causes less postoperative pain and fewer complications than excisional hemorrhoidectomy and stapled hemorrhoidopexy, but has a higher recurrence rate. Excisional hemorrhoidectomy or stapled hemorrhoidopexy is recommended for treatment of grade 4 hemorrhoids. Stapled hemorrhoidopexy has a faster postoperative recovery, but a higher recurrence rate. Postoperative pain from excisional hemorrhoidectomy can be treated with nonsteroidal anti-inflammatory drugs, narcotics, fiber supplements, and topical antispasmodics. Thrombosed external hemorrhoids can be treated conservatively or excised.
Hemorrrhoids result from dilation of the submucosal vascular tissue in the distal anal canal. This vascular tissue is supported by connective tissue that, when weakened, leads to descent or prolapse of the hemorrhoids. Internal hemorrhoids originate above the dentate line (i.e., the junction between columnar and squamous epithelium) and are viscerally innervated and, therefore, painless. External hemorrhoids originate below the dentate line, have somatic innervation, and can cause pain. Some patients have both internal and external (mixed) hemorrhoids.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Fiber supplementation should be recommended to decrease symptoms in all patients with hemorrhoids. | A | 5 |
| Excision of thrombosed external hemorrhoids provides more rapid pain relief than conservative treatment. | B | 8 |
| Rubber band ligation causes less postoperative pain and fewer complications than stapled hemorrhoidopexy and excisional hemorrhoidectomy, and is the surgical treatment of choice for grades 1 and 2 hemorrhoids. | A | 11 |
| Excisional hemorrhoidectomy has a lower risk of recurrence than stapled hemorrhoidopexy. | A | 10, 25, 26, 28 |
| Stapled hemorrhoidopexy causes less postoperative pain, pruritus, and fecal urgency than excisional hemorrhoidectomy. | A | 10, 25, 26, 28 |
| Topical diltiazem (obtained from a compounding pharmacy) can be used to decrease postoperative pain after excisional hemorrhoidectomy. | B | 30 |
Internal hemorrhoids are classified according to their degree of prolapse. Grade 1 hemorrhoids may bleed but do not protrude; grade 2 hemorrhoids protrude with defecation but reduce spontaneously; grade 3 hemorrhoids protrude and must be reduced by hand; and grade 4 hemorrhoids are permanently prolapsed.1
Epidemiology
The prevalence of hemorrhoids has been estimated at 4.4 percent of U.S. adults, with the highest prevalence in those between 45 and 65 years of age.2 Factors that increase intra-abdominal pressure (e.g., prolonged straining, constipation, pregnancy, ascites) contribute to dilatation, engorgement, and prolapse of hemorrhoidal vascular tissue.
Clinical Features
Many persons treat the symptoms of hemorrhoids without medical advice. Patients may present to physicians when symptoms worsen. Both internal and external hemorrhoids can cause anal discharge and itching because of difficulty with hygiene. Internal hemorrhoids typically cause prolapse or painless rectal bleeding that is reported as blood on the toilet paper or bleeding associated with bowel movements. External hemorrhoids can cause anal discomfort because of engorgement. Thrombosis of external hemorrhoids can cause acute pain.
DIAGNOSIS
Several anorectal conditions may cause symptoms similar to those associated with hemorrhoids (Table 1). Factors that may indicate more serious conditions (e.g., cancer, inflammatory bowel disease) and that should prompt consideration of colonoscopy include change in bowel habit, abdominal pain, weight loss, rectal bleeding with blood in the stool, or a family history of colon cancer.
| Diagnosis | Historical features | Physical examination findings |
|---|---|---|
| Anal cancer | Pain around anus; weight loss in advanced cases | Ulcerating lesion of anus |
| Anal condylomata | Anal mass without bleeding; history of anal intercourse | Cauliflower-like lesions |
| Anal fissure | Tearing pain and bleeding with bowel movement | Painful rectal examination with fissure |
| Colorectal cancer | Blood in stool, weight loss, abdominal pain, change in bowel habit, family history | Abdominal mass or tenderness |
| Inflammatory bowel disease | Constitutional symptoms, abdominal pain, diarrhea, family history | Normal external rectal examination; rarely, fistula; colitis on anoscopy |
| Perianal abscess | Gradual onset of pain | Tender mass covered with skin as opposed to rectal mucosa |
| Skin tags | No bleeding; history of resolved | Tags visualized around anus covered |
| hemorrhoids | with normal skin, not mucosa |
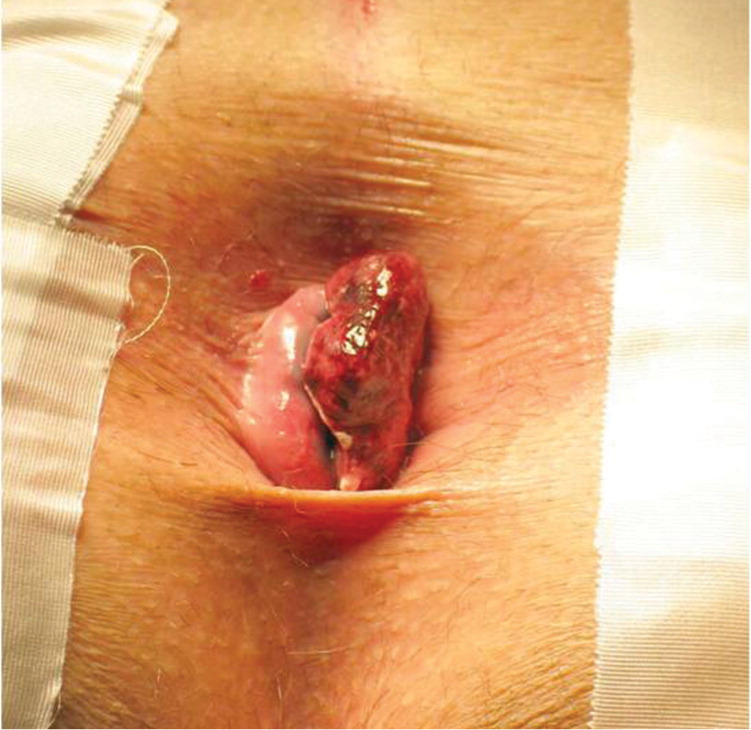
Physical examination should include an abdominal examination, inspection of the perineum, digital rectal examination, and anoscopy. Digital rectal examination alone can neither diagnose nor exclude internal hemorrhoids; anoscopy is required. On anoscopy, internal hemorrhoids appear as dilated purplish-blue veins, and prolapsed internal hemorrhoids appear as dark pink, glistening, and sometimes tender masses at the anal margin (Figure 1). External hemorrhoids appear less pink and, if thrombosed, are acutely tender with a purplish hue (Figure 2). Perianal skin tags, which are often remnants of previous external hemorrhoids, may be present. Some experts recommend colonoscopy for all patients older than 40 years who have hemorrhoidal symptoms and rectal bleeding.3 The American Society of Colon and Rectal Surgeons recommends taking the patient history and performing a physical examination with anoscopy and further endoscopic evaluation if there is concern for inflammatory bowel disease or cancer.4 A complete evaluation of the colon is warranted in the following groups:
Patients who are 50 years or older and have not had a complete examination of the colon within the past 10 years
Patients who are 40 years or older and have not had a complete examination of the colon within the past 10 years, and who have one first-degree relative in whom colorectal cancer or adenoma was diagnosed at age 60 years or younger
Patients who are 40 years or older and have not had a complete examination of the colon within the past five years, and who have more than one first-degree relative in whom colorectal cancer or adenoma was diagnosed at age 60 years or younger
Patients with iron deficiency anemia
Patients who have a positive fecal occult blood test.4

Management
MEDICAL TREATMENT
Medical management is appropriate for grade 1 hemorrhoids. All patients with hemorrhoids should maintain soft bulky stools that can be passed without straining. This is also important after surgery because straining and passage of hard stools increase pain and bleeding, and delay healing. Adequate intake of fluid and fiber helps soften the stool. A metaanalysis of seven randomized trials of patients with symptomatic hemorrhoids showed that fiber supplementation with psyllium, sterculia, or unprocessed bran decreased bleeding, pain, prolapse, and itching.5
Nonprescription topical preparations containing steroids, anesthetics, astringents, and/or antiseptics are often recommended for all grades of hemorrhoidal disease. However, no randomized studies support their use. Steroid-containing creams should not be used for prolonged periods because of their atrophic effects on skin. Sitz baths are commonly recommended, but a review of studies found no benefit for various anorectal disorders, including hemorrhoids.6
THROMBOSED EXTERNAL HEMORRHOIDS
Thrombosed external hemorrhoids cause acute, severe pain. Without intervention, the pain typically improves over two to three days, with continued improvement as the thrombus gradually absorbs over several weeks. Analgesics and stool softeners may be beneficial. Topical therapy with nifedipine and lidocaine cream (not available in the United States) is more effective for pain relief than lidocaine (Xylocaine) alone.7
In patients with severe pain from thrombosed hemorrhoids, excision or incision and evacuation of the thrombus within 72 hours of symptom onset provide more rapid pain relief than conservative treatment. 8 Both procedures can be performed under local anesthesia, and the resulting wound can be left open or sutured.9
HEMORRHOIDS IN PREGNANCY
Pregnancy predisposes women to symptomatic hemorrhoids that usually resolve after delivery. Surgical intervention is contraindicated because of the risk of inducing labor. Conservative treatment is recommended, with excision of thrombosed external hemorrhoids if necessary.
Surgical Treatment of Internal Hemorrhoids
Most patients with grade 1 or 2 hemorrhoids, and many with grade 3 hemorrhoids, can be treated in primary care offices. Patients in whom office-based treatment is ineffective and those with mixed hemorrhoids may require treatment in surgical suites with facilities for anesthesia. The most common surgical treatments are ligation or tissue destruction, fixation techniques (i.e., hemorrhoidopexy), and excision (i.e., hemorrhoidectomy; Table 2).
| Type of surgery | Procedure | Anesthesia | Comments |
|---|---|---|---|
| Excision | Excisional hemorrhoidectomy | Local with sedation or general | Hospital based; preoperative enema needed |
| Fixation | Stapled hemorrhoidopexy | Local with sedation or general | Hospital based; preoperative enema needed |
| Ligation and tissue destruction | Rubber band ligation | None | Office based; no preoperative enema needed |
| Infrared coagulation | None | Office based; no preoperative enema needed | |
| Injection sclerotherapy | None | Office based; no preoperative enema needed; higher failure rate than rubber band ligation, excisional hemorrhoidectomy, and stapled hemorrhoidopexy |
RUBBER BAND LIGATION
Rubber band ligation is a common office treatment for internal hemorrhoids and is often recommended as the initial surgical treatment for grades 1 to 3 hemorrhoids.10 The procedure involves placing a rubber band around a portion of redundant anorectal mucosa. This causes strangulation of the blood supply to the hemorrhoid, resulting in tissue necrosis and sloughing of the hemorrhoid in five to seven days. Healing of the small residual ulcer provides fixation of the local mucosa to underlying muscle. The procedure is performed through an anoscope, and a variety of devices are available to apply the bands. Because the bands are placed in the insensate region (above the dentate line), the procedure can be performed without anesthesia. Nevertheless, the area should be tested for sensation before applying the band because of anatomic variation in innervation. One to three bands can be applied per session, depending on the surgeon's preference and patient tolerance. Subsequent bandings can occur at four- to six-week intervals.11 Rates of success, defined as symptom relief for months to years, range from 70.5 to 97 percent.12–15
Complications such as vasovagal response, pain, abscess formation, urinary retention, bleeding, band slippage, and sepsis occur in less than 2 percent of patients undergoing rubber band ligation.16–18 Secondary thrombosis of the external hemorrhoidal component may occur in 2 to 11 percent of patients.19 Because of the risk of postoperative hemorrhage, rubber band ligation should not be performed in patients receiving warfarin (Coumadin). Aspirin and other antiplatelet agents should be discontinued five to seven days before the procedure and restarted five to seven days afterward.
INFRARED COAGULATION
Infrared coagulation involves the application by a polymer probe tip of radiation from a tungsten-halogen lamp to the base of the hemorrhoid. This creates an ulcer that subsequently heals, producing cicatrisation (scarring) that reduces blood flow to the hemorrhoid. The procedure is well tolerated, but success rates are lower than those with rubber band ligation.13 Infrared coagulation may be considered in patients who are on anticoagulant therapy.20
EXCISIONAL HEMORRHOIDECTOMY
In excisional hemorrhoidectomy, an elliptical incision is made over the hemorrhoidal complex, which is then mobilized from the underlying sphincter and excised. The wound is closed with sutures.20
Several randomized controlled trials (RCTs) and meta-analyses have shown that excisional hemorrhoidectomy is the most effective treatment to reduce recurrent symptoms in patients with grade 3 or 4 hemorrhoids.3,21 It is also recommended for patients with mixed hemorrhoids and for those with recurrent hemorrhoids in whom other treatments have been ineffective.21,22
A Cochrane review of three RCTs comparing excisional hemorrhoidectomy to rubber band ligation showed that ligation resulted in less postoperative pain and allowed patients to return to work and to their previous level of functioning faster.11 Patients who underwent excisional hemorrhoidectomy for grade 3 hemorrhoids had less symptom recurrence and reduced need for subsequent procedures compared with those who underwent rubber band ligation. For patients with grade 2 hemorrhoids, there was no difference in symptom recurrence between the procedures. The authors concluded that rubber band ligation can be considered the treatment of choice for grade 2 hemorrhoids, reserving excisional hemorrhoidectomy for grade 3 hemorrhoids or recurrence after rubber band ligation. There was no difference between the procedures in patient satisfaction or in the incidence of postoperative complications, such as urinary retention, anal stenosis, or hemorrhage. Other postoperative complications of excisional hemorrhoidectomy include skin tags, abscess, fistula, and anal leakage.20
STAPLED HEMORRHOIDOPEXY
Stapled hemorrhoidopexy is an alternative treatment for grades 2 to 4 hemorrhoids.23 The device removes a circumferential column of mucosa and submucosa immediately above the hemorrhoids, thus interrupting the blood supply. The ring of staples fixes the downwardly displaced vascular cushions back into their original locations to restore anatomy and function.24 Postoperatively, patients have a circular staple line above the dentate line, which becomes buried within the mucosa over time. Staples can be noted within the rectum for many months after the procedure and can cause rectal bleeding.
Compared with excisional hemorrhoidectomy, stapled hemorrhoidopexy is more favorable in terms of postoperative pain, time until return to work, and complications of pruritus and fecal urgency. However, it is associated with higher long-term risk of recurrent hemorrhoids and the need for additional procedures (Table 3). 25 A meta-analysis of RCTs comparing long-term results (12 to 84 months) of both procedures found that patients were twice as likely to require further treatment after stapled hemorrhoidopexy.26 Short- and long-term data show similar patient satisfactionbetween the procedures, suggesting that the early postoperative benefits of stapled hemorrhoidopexy may overridethe increased risk of additional surgery.26,27
| Outcome measure (trials included in assessment) | Favors excisional hemorrhoidectomy | Favors stapled hemorrhoidopexy |
|---|---|---|
| Long-term risk of hemorrhoid recurrence at all time points (n = 7)* | X | |
| Postoperative anal stenosis at all time points (n = 2)† | X | |
| Postoperative bleeding at all time points (n = 6)† | X | |
| Postoperative fecal urgency at final follow-up (n = 4)† | X | |
| Postoperative pain at all time points (n = 5)† | X | |
| Postoperative pruritus at all time points (n = 2)† | X | |
| Postoperative soiling or difficulty with hygiene (n = 5)† | X | |
| Postoperative symptom recurrence at final follow-up (n = 5)† | X |
OTHER PROCEDURES
POSTOPERATIVE CARE
Excisional hemorrhoidectomy causes significant postoperative pain, whereas rubber band ligation and stapled hemorrhoidopexy typically are not painful. The use of nonsteroidal anti-inflammatory drugs, supplemented with narcotics, is usually necessary. However, narcotics can cause constipation, leading to increased bleeding, pain, suture breakdown, and loose staples. Stool softeners and bulking agents are recommended after all procedures. Sitz baths and warm water sprays can be used to keep the site clean, particularly after excisional hemorrhoidectomy. Topical metronidazole (Metrogel) 10% applied three times per day and topical diltiazem have been shown to decrease postoperative pain29,30 ; these formulations are not available commercially but can be obtained from a compounding pharmacy. Topical nitroglycerin 0.2% applied twice per day decreases postoperative pain by relaxation of spasm in the internal anal sphincter.31
Choice of Procedure
The choice of procedure should be based on the patient's symptoms, the extent of the hemorrhoidal disease, and the experience of the surgeon. Rubber band ligation is usually the procedure of choice for grades 1 and 2 hemorrhoids. In patients with circumferential grade 2 disease, stapled hemorrhoidopexy is associated with a lower recurrence rate but a longer time until return to work, and more postoperative pain.23 Rubber band ligation can be used for grade 3 hemorrhoids; stapled hemorrhoidopexy and excisional hemorrhoidectomy are also options and have better long-term effectiveness, but cause more postoperative pain and complications and have longer recovery times. Excisional hemorrhoidectomy and stapled hemorrhoidopexy are options for grade 4 hemorrhoids. Excisional hemorrhoidectomy is recommended for mixed internal and external hemorrhoids, but infrared coagulation is a good option for patients who are on anticoagulation therapy (Table 4).
| Hemorrhoid type/grade | Office-based procedures | Hospital-based procedures |
|---|---|---|
| External (not graded) | In patients with severe symptoms, excision or incision under local anesthesia within 72 hours of onset; after 72 hours use medical treatment | — |
| Combined external and internal | — | Excisional hemorrhoidectomy |
| Internal grade 1 | Rubber band ligation, infrared coagulation | Rubber band ligation; excisional hemorrhoidectomy if primary treatment is ineffective |
| Internal grade 2 | Rubber band ligation, infrared coagulation | Rubber band ligation; stapled hemorrhoidopexy; excisional hemorrhoidectomy if primary treatment is ineffective |
| Internal grade 3 | Rubber band ligation | Rubber band ligation; excisional hemorrhoidectomy; stapled hemorrhoidopexy |
| Internal grade 4 | — | Excisional hemorrhoidectomy; stapled hemorrhoidopexy |
Data Sources: The following evidence-based medicine resources were searched using the key words stapled hemorrhoidopexy, hemorrhoidectomy, hemorrhoids, hemorrhoid treatment, rubber band ligation hemorrhoids, hemorrhoid surgery, hemorrhoids pregnancy, and thrombosed external hemorrhoids: Essential Evidence Plus, the Cochrane Database of Systematic Reviews, Pubmed, UpToDate, the National Guideline Clearinghouse, the Institute for Clinical Systems Improvement, and the Database of Abstracts of Reviews of Effects. Search date: January 12, 2010.
