
Am Fam Physician. 2011;84(10):1157-1159
Author disclosure: No relevant financial affiliations to disclose.
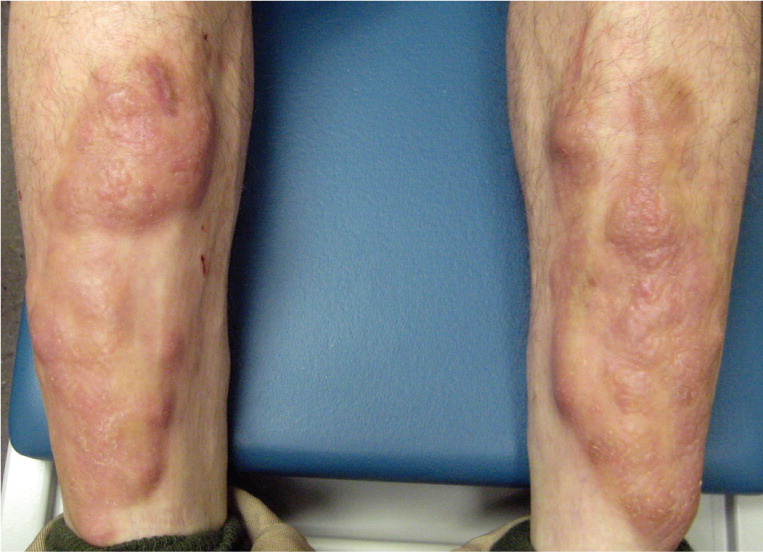
A 29-year-old man presented with a one-year history of progressive discoloration and thickening of the skin on both shins. He also had exophthalmos in both eyes, heat intolerance, slight tremor, diarrhea, and unintentional weight loss.
Physical examination revealed violaceous to yellow nodules on the anterior surfaces of the bilateral lower legs (see accompanying figure) that were boggy and nontender. The nodules had a peau d'orange texture.
Question
Discussion
The answer is D: pretibial myxedema (thyroid dermopathy) secondary to Graves disease. Graves disease is an autoimmune disorder that causes the excessive release of thyroid hormone through the action of thyrotropin receptor antibodies. Signs and symptoms include nervousness, heat intolerance, palpitations, frequent bowel movements, weight loss, proptosis, and tremor.1 The classic triad of Graves disease is hyperthyroidism, exophthalmos, and pretibial myxedema.
Pretibial myxedema occurs in up to 5 percent of patients with Graves disease.2 The cause is the immunologically mediated accumulation of glycosaminoglycans in the dermis.2 Pretibial myxedema is typically located in the pretibial region but can involve the dorsal feet, upper extremities, or face. It usually manifests as indurated nodules or plaques that are flesh-colored to violaceous.3 A peau d'orange appearance is possible because of the prominence of hair follicles. Less common presentations of pretibial myxedema include a diffuse brawny edema without nodules, and a verrucous form that may affect the entire extremity (elephantiasic pretibial myxedema).4 Severe pretibial myxedema is also associated with thyroid acropachy, which is characterized by digital clubbing, soft tissue swelling with pain in the hands and feet, and periosteal thickening.5
Elephantiasis nostras is a rare, deforming condition caused by chronic lymphedema and recurrent inflammation. It leads to hyperkeratotic plaques and nodules in a cobblestone pattern on the lower extremities.7 There are no associated systemic symptoms.
Erythema nodosum is an inflammatory process of the subcutaneous fat that presents as symmetric, tender, erythematous, subcutaneous nodules on both lower extremities. Although the condition is most often idiopathic or postinfectious, assessment for an underlying systemic disease or offending medication may be warranted. Possible triggers include sulfonamides, oral contraceptives, pregnancy, sarcoidosis, streptococcal pharyngitis, tuberculosis, and ulcerative colitis.8
Lichen myxedematosus (papular mucinosis) is a rare inflammatory disease of fibroblastic proliferation and dermal mucin deposition. It produces a fleshy, papular skin eruption that may coalesce into plaques, most commonly on the face, dorsal hands, and extensor surface of the extremities.9 The condition is usually associated with monoclonal gammopathy. Systemic symptoms, if present, affect the gastrointestinal, pulmonary, muscular, and neurologic systems.10
Sarcoidosis is a multisystem disease, with skin involvement in approximately 25 percent of cases.11 The cutaneous manifestation varies, including papules, plaques, nodules, scars, hypopigmented macules, erythroderma, or ulcerations affecting any part of the body.11 Up to 5 percent of patients with sarcoidosis have subcutaneous nodules (Darier-Roussy sarcoid), often involving the extremities.12 Characteristic noncaseating granulomas are visible on histopathologic examination. Systemic symptoms are typically pulmonary, ocular, or neurologic.13
| Condition | Characteristics |
|---|---|
| Elephantiasis nostras | Hyperkeratotic plaques and nodules in a cobblestone pattern on lower extremities |
| No systemic symptoms | |
| Erythema nodosum | Symmetric, tender, erythematous, subcutaneous nodules on both lower extremities |
| Often idiopathic and postinfectious; possible triggers include sulfonamides, oral contraceptives, pregnancy, sarcoidosis, streptococcal pharyngitis, tuberculosis, and ulcerative colitis | |
| Lichen myxedematosus | Fleshy papules or plaques on the face, dorsal hands, or extensor surface of extremities |
| Gastrointestinal, pulmonary, muscular, or neurologic symptoms may occur | |
| Pretibial myxedema | Indurated nodules or plaques on the lower extremities that are flesh-colored to violaceous |
| Endocrine, gastrointestinal, cardiovascular, ocular, or neurologic symptoms may occur | |
| Sarcoidosis | Varied manifestations, including papules, plaques, nodules, scars, hypopigmented macules, erythroderma, or ulcerations affecting any part of the body |
| Systemic symptoms are typically pulmonary, ocular, or neurologic |
