
This is a corrected version of the article that appeared in print.
Am Fam Physician. 2012;85(1):49-56
Related letter: Effectiveness of Glucosamine and Chondroitin for Osteoarthritis
Patient information: See related handout on osteoarthritis, written by the author of this article.
Author disclosure: No relevant financial affiliations to disclose.
Osteoarthritis is a common degenerative disorder of the articular cartilage associated with hypertrophic bone changes. Risk factors include genetics, female sex, past trauma, advancing age, and obesity. The diagnosis is based on a history of joint pain worsened by movement, which can lead to disability in activities of daily living. Plain radiography may help in the diagnosis, but laboratory testing usually does not. Pharmacologic treatment should begin with acetaminophen and step up to nonsteroidal anti-inflammatory drugs. Exercise is a useful adjunct to treatment and has been shown to reduce pain and disability. The supplements glucosamine and chondroitin can be used for moderate to severe knee osteoarthritis when taken in combination. Corticosteroid injections provide inexpensive, short-term (four to eight weeks) relief of osteoarthritic flare-ups of the knee, whereas hyaluronic acid injections are more expensive but can maintain symptom improvement for longer periods. Total joint replacement of the hip, knee, or shoulder is recommended for patients with chronic pain and disability despite maximal medical therapy.
Osteoarthritis is a common degenerative disorder of the articular cartilage associated with hypertrophic changes in the bone.1 Risk factors include genetics, female sex, past trauma, advancing age, and obesity.2 As the U.S. population ages and becomes more obese, family physicians can expect to see more patients with osteoarthritis.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Physical therapy using land-based or water-based exercise can help reduce pain and improve function in patients with osteoarthritis. | B | 10–12 |
| Acetaminophen should be used as first-line therapy for mild osteoarthritis. | A | 16 |
| Nonsteroidal anti-inflammatory drugs are superior to acetaminophen for treating moderate to severe osteoarthritis. | A | 16 |
| Intra-articular corticosteroid injections can be beneficial for short-term (i.e., less than eight weeks) relief of osteoarthritis pain of the knee. | A | 21, 22 |
| Compared with intra-articular corticosteroids, intra-articular hyaluronic acid injections of the knee are less effective in the short term, equivalent in the intermediate term (i.e., four to eight weeks), and superior in the long term. | B | 26, 27 |
| The combination of glucosamine and chondroitin may decrease pain in patients with moderate to severe knee osteoarthritis, although the evidence for this effect is limited and inconsistent. | B | 30 |
| Patients who have continued pain and disability from osteoarthritis of the hip, knee, or shoulder despite maximal medical therapy are candidates for total joint replacement. | B | 35 |
Diagnosis
The most common symptom of osteoarthritis is joint pain. The pain tends to worsen with activity, especially following a period of rest; this has been called the gelling phenomenon. Osteoarthritis can cause morning stiffness, but it usually lasts for less than 30 minutes, unlike rheumatoid arthritis, which causes stiffness for 45 minutes or more.3 Patients may report joint locking or joint instability. These symptoms result in loss of function, with patients limiting their activities of daily living because of pain and stiffness.
The joints most commonly affected are the hands, knees, hips, and spine, but almost any joint can be involved. Osteoarthritis is often asymmetric. A patient may have severe, debilitating osteoarthritis of one knee with almost normal function of the opposite leg.
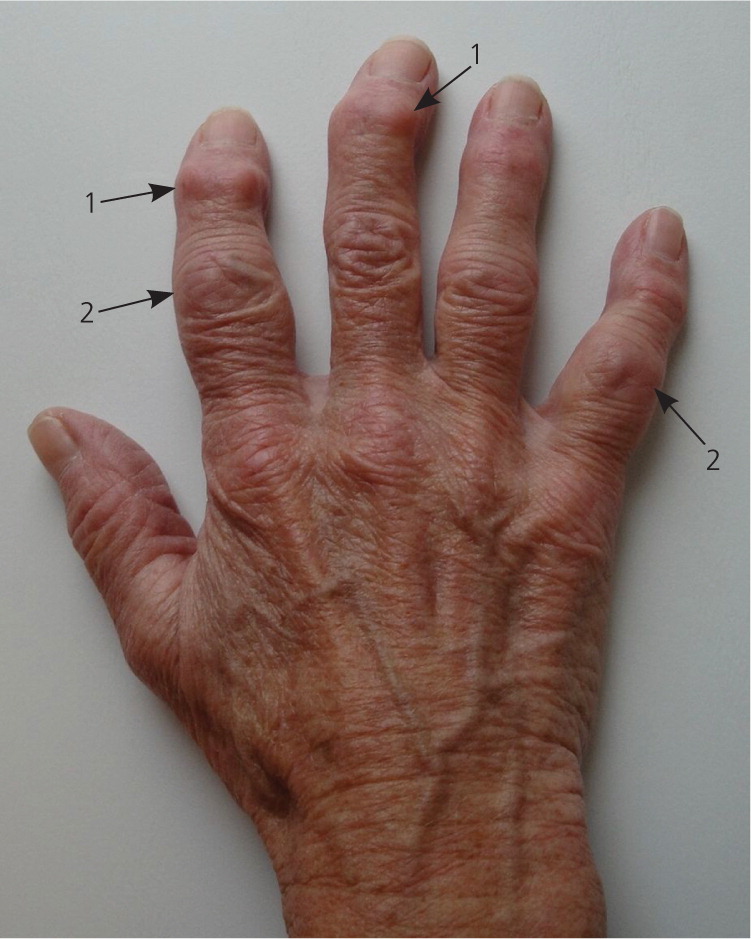
Physical examination is important in making the diagnosis. Pain on range of motion and limitation of range of motion are common to all forms of osteoarthritis, but each joint has unique physical examination findings (Table 1). [corrected] Figure 1 shows a hand with typical changes of osteoarthritis.
| Hand |
| Pain on range of motion |
| Hypertrophic changes at distal and proximal interphalangeal joints (Heberden nodes and Bouchard nodes; Figure 1) |
| Tenderness over carpometacarpal joint of thumb |
| Shoulder |
| Pain on range of motion |
| Limitation of range of motion, especially external rotation |
| Crepitus on range of motion |
| Knee |
| Pain on range of motion |
| Joint effusion |
| Crepitus on range of motion |
| Presence of popliteal cyst (Baker cyst) |
| Lateral instability |
| Valgus or varus deformity |
| Hip |
| Pain on range of motion |
| Pain in buttock |
| Limitation of range of motion, especially internal rotation |
| Foot |
| Pain on ambulation, especially at first metatarsophalangeal joint |
| Limited range of motion of first metatarsophalangeal joint, hallux rigidus |
| Hallux valgus deformity |
| Spine |
| Pain on range of motion |
| Limitation of range of motion |
| Lower extremity sensory loss, reflex loss, motor weakness caused by nerve root impingement |
| Pseudoclaudication caused by spinal stenosis |
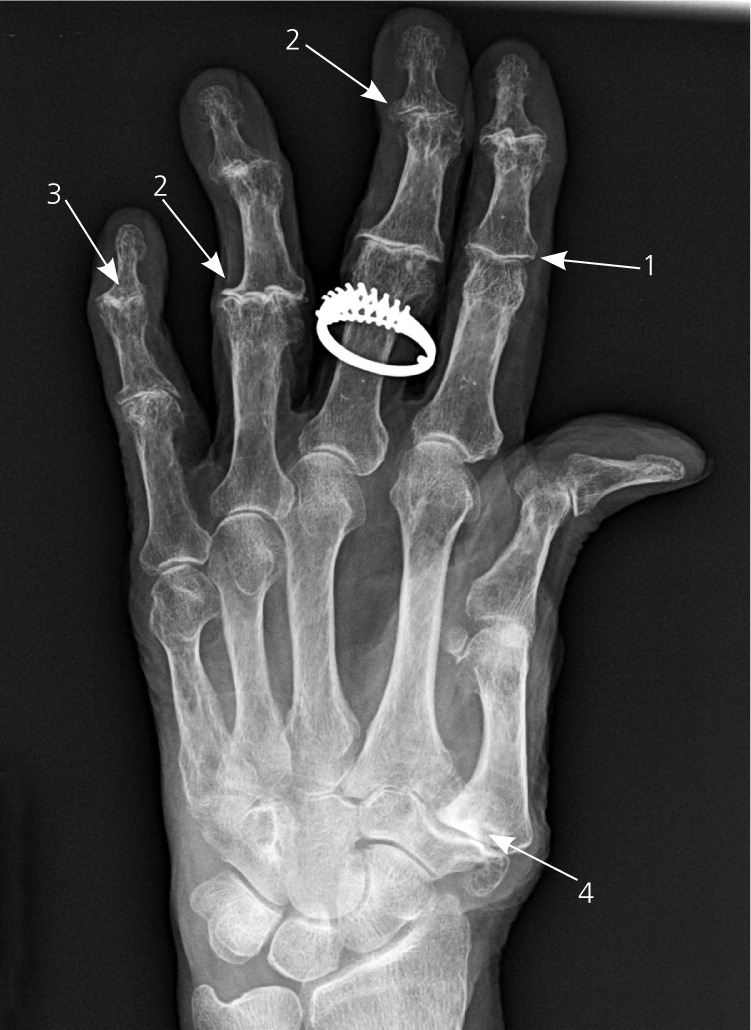
Because osteoarthritis is primarily a clinical diagnosis, physicians can confidently make the diagnosis based on the history and physical examination. Plain radiography can be helpful in confirming the diagnosis and ruling out other conditions.1 Advanced imaging techniques, such as computed tomography or magnetic resonance imaging, are rarely needed unless the diagnosis is in doubt and there is a strong suspicion for another etiology, such as a meniscal injury. Figures 2 through 4 show examples of radiography of the hand, hips, and knee.


Laboratory testing usually is not required to make the diagnosis. Markers of inflammation, such as erythrocyte sedimentation rate and C-reactive protein level, are typically normal. Immunologic tests, such as antinuclear antibodies and rheumatoid factor, should not be ordered unless there is evidence of joint inflammation or synovitis, which makes autoimmune arthritis a more likely diagnosis. A uric acid level is recommended only if gout is suspected. Because false-positive results are possible, ordering some of these tests may add unnecessary confusion if the pretest probability of gout or an autoimmune arthritis is low.4,5 Rheumatic panels (e.g., erythrocyte sedimentation rate, rheumatoid factor, antinuclear antibodies, uric acid, Lyme serology in some areas) have an especially high rate of false-positive results in primary care populations. An American College of Rheumatology clinical guideline recommends against the routine ordering of arthritis panels for patients with joint problems.6
Treatment
Treatment choices fall into four main categories: nonpharmacologic, pharmacologic, complementary and alternative, and surgical. In general, treatment should begin with the safest and least invasive therapies before proceeding to more invasive, expensive therapies. All patients with osteoarthritis should receive at least some treatment from the first two categories. Surgical management should be reserved for those who do not improve with behavioral and pharmacologic therapy, and who have intractable pain and loss of function.
NONPHARMACOLOGIC
Nonpharmacologic therapy often starts with exercise. A randomized clinical trial compared supervised home-based exercise with no exercise in 786 patients with osteoarthritis of the knee. The exercise program consisted of muscle strengthening and range-of-motion exercises. The researchers found statistically significant improvements in a validated arthritis symptom score at six, 12, 18, and 24 months.9
A Cochrane review of exercise for osteoarthritis of the knee concluded that land-based exercise can result in short-term reduction of pain and improvement in physical function.10 A similar Cochrane review of water-based exercise for knee and hip osteoarthritis showed improvement, but the results were not as robust.11 A randomized controlled trial of 200 persons compared education by a primary care physician to exercise supervised by a physical therapist. The supervised exercise program had better short-term outcomes, but the differences were no longer noted at 36 weeks.12
Therapeutic ultrasound is a physical therapy modality often used in osteoarthritis treatment. A Cochrane review of this modality concluded that although statistically significant improvements were noted in visual analog pain scales following therapeutic ultrasound for knee osteoarthritis, the clinical significance of these changes is questionable.13 The authors found that the studies were underpowered to properly determine the effectiveness of therapeutic ultrasound for knee or hip osteoarthritis. A Cochrane review on transcutaneous electrical nerve stimulation found no clinically significant improvement in knee osteoarthritis pain.14
Because obesity is considered a major risk factor for osteoarthritis, studies have investigated whether weight loss improves patient outcomes. A meta-analysis of weight reduction and knee osteoarthritis concluded that weight loss of 5 percent from baseline was sufficient to reduce disability.15 Additionally, pain and disability were reduced if patients lost more than 6 kg (13.2 lb).15 Aerobic exercise is important for weight loss, but can be challenging in persons with osteoarthritis of weight-bearing joints. Swimming, elliptical training, cycling, and upper body exercise may help in such cases.
Other nonpharmacologic treatments include bracing and splinting to help support painful or unstable joints. A cane can help reduce the weight load in persons with hip or knee osteoarthritis, but it needs to be properly fitted and used on the side contralateral to the affected joint.3
PHARMACOLOGIC
The mainstay of treatment for mild osteoarthritis is acetaminophen.16 It is inexpensive, safe, and effective. A 2006 Cochrane review concluded that acetaminophen is better than placebo for treating mild osteoarthritis, and equal to nonsteroidal anti-inflammatory drugs (NSAIDs), but with fewer gastrointestinal adverse effects.16 Patients should be instructed to take 650 to 1,000 mg of acetaminophen up to four times per day to relieve osteoarthritis symptoms. The U.S. Food and Drug Administration recommends no more than 4,000 mg of acetaminophen per day to avoid liver toxicity. It further cautions patients to be aware of coincident use of other over-the-counter or prescription medications that may contain acetaminophen.17
When acetaminophen fails to control symptoms, or if symptoms are moderate to severe, NSAID therapy is recommended. NSAIDs as a class are superior to acetaminophen for treating osteoarthritis.16 Patients taking NSAIDs should be cautioned about adverse effects, which may include gastrointestinal bleeding, renal dysfunction, and blood pressure elevation (number needed to harm = 12).16 There have not been many head-to-head studies comparing nonsteroidal agents, so less expensive, generic products are appropriate (e.g., ibuprofen, naproxen, diclofenac). Cyclooxygenase-2 inhibitors, such as celecoxib (Celebrex), have an improved safety profile for gastrointestinal adverse effects,18 but are costly and confer an increased cardiovascular risk.19 Table 2 lists medications commonly used to treat osteoarthritis, typical dosing, and relative costs.
| Medication | Typical dosage | Cost of generic (brand)* |
|---|---|---|
| Acetaminophen | 650 to 1,000 mg four times per day | $17 ($20) |
| Celecoxib (Celebrex) | 200 mg per day | NA ($141) |
| Diclofenac sodium | 50 mg two to three times per day | $46 (NA) |
| Diclofenac/misoprostol (Arthrotec) | 50 mg/200 mcg two to three times per day | NA ($195) |
| Ibuprofen, over-the-counter | 400 to 600 mg three times per day | $28† ($30) |
| Meloxicam (Mobic) | 7.5 to 15 mg per day | $16† ($155) |
| Nabumetone | 500 mg two times per day | $40 (NA) |
| Naproxen, over-the-counter (Aleve) | 220 to 440 mg two times per day | $5 ($5) |
| Naproxen (Naprosyn) | 250 to 500 mg two times per day | $20† ($151) |
| Oxaprozin (Daypro) | 1,200 mg per day | $26 ($206) |
| Sulindac (Clinoril) | 150 to 200 mg two times per day | $19 ($92‡) |
Opioids are often used to treat pain and are an option for osteoarthritis pain. Because of the potential for abuse, opioids should be an option only if the patient has not responded to acetaminophen or NSAID therapy, or cannot tolerate them because of adverse effects. Opioids should be prescribed first at low dosages and carefully monitored to evaluate for potential dependence. Opioids also may cause chronic constipation and can place older patients at risk of falls.3,20
Intra-articular injections of corticosteroids or hyaluronic acid are another option for treating osteoarthritis. The use of intra-articular corticosteroids primarily provides short-term relief lasting four to eight weeks. It has proven effectiveness in osteoarthritis of the knee,21,22 but may not be as effective for osteoarthritis of the shoulder 23 or hand.24 Many physicians inject a corticosteroid and a local anesthetic, such as lidocaine (Xylocaine). The lidocaine can provide some immediate relief, which confirms that the medication was injected into the correct area. Patients should be warned of a potential flare-up of symptoms within the first 24 hours, followed by an improvement from baseline at 48 hours. Repeat injections are possible in the same joint, but usual practice is limited to four injections annually.25
Intra-articular hyaluronic acid injections, also known as viscosupplementation, are widely used by orthopedic surgeons to treat osteoarthritis of the knee. There has been some debate about the effectiveness of viscosupplementation in earlier studies, most of which were manufacturer-sponsored studies. However, a Cochrane review of 76 clinical trials concluded that viscosupplementation was effective for treating knee osteoarthritis.26 The treatment effect often lasted for up to four months and led to improvements in pain and function.26 The biggest drawback of hyaluronic acid injections is the cost. Table 3 provides a cost comparison of intra-articular injections.
| Code | Description | Self-pay fee | Private insurance reimbursement | Medicare allowable fee |
|---|---|---|---|---|
| J3301 | Injection, triamcinolone acetonide (Kenalog), not otherwise specified, 10 mg | $17.00 | $4.50 | $1.54 |
| J7324 | Hyaluronan or derivative, Orthovisc, for intra-articular injection, per dose | $880.00 | $342.00 | $181.10 |
| 20610 | Arthrocentesis, aspiration, and/or injection: major joint or bursa (e.g., shoulder, hip, knee joint; subacromial bursa) | $182.00 | $139.00 | $59.81 |
There have been head-to-head trials of corticosteroid injections versus hyaluronic acid. A meta-analysis of knee injections found that corticosteroids had a better short-term response rate and were equal to hyaluronic acid in the intermediate four- to eight-week range, but were inferior to hyaluronic acid after eight weeks from the time of injection.27 Therefore, in stable patients with an acute flare-up of osteoarthritis symptoms, corticosteroids may be preferred. For patients experiencing chronic osteoarthritis pain, hyaluronic acid should be considered. The technique of injection is the same for either medication.
COMPLEMENTARY AND ALTERNATIVE MEDICINE
The most widely used supplements for osteoarthritis are glucosamine and chondroitin. The literature consisted of small clinical trials until the release of the Glucosamine/Chondroitin Arthritis Intervention Trial (GAIT), which included more than 1,500 patients. The trial had five arms comparing glucosamine alone, chondroitin alone, a combination of glucosamine and chondroitin, celecoxib, and placebo. The results were favorable only for the combination of glucosamine and chondroitin, which appeared to be effective for moderate to severe osteoarthritis of the knee.30 Chondroitin alone did not show benefit for osteoarthritis of the knee or hip in a meta-analysis.31
Balneotherapy is a heterogeneous group of treatments also known as spa therapy or mineral baths. A Cochrane review concluded that mineral baths were of some benefit to patients with osteoarthritis, but the authors addressed methodologic flaws in the studies and urged caution in interpreting the findings.32 Capsaicin cream is a topical analgesic derived from chili peppers. It has been found to be superior to placebo in treating osteoarthritis pain. It is widely available, is relatively inexpensive, and can be used as an adjunct to standard osteoarthritis treatments.33 There also is evidence supporting the use of the supplement S-adenosylmethionine (SAM-e) to reduce functional limitation, but not compared with placebo in patients with osteoarthritis pain. The effectiveness of SAM-e is comparable to that of NSAIDs in some studies but with fewer adverse effects.34
SURGICAL
Surgery should be reserved for patients whose symptoms have not responded to other treatments. The well-accepted indication for surgery is continued pain and disability despite conservative treatment. The most effective surgical intervention is total joint replacement, with excellent patient outcomes following total joint replacement of the hip, knee, and shoulder.1,35 Many different prosthetic devices are available; however, controlled trials comparing the various devices are lacking. Patients can expect that most current joint prostheses will function well for 15 to 20 years.35
There are other surgical approaches to osteoarthritis treatment, but they have not equaled the success of total joint replacement. Randomized trials of arthroscopic debridement for osteoarthritis of the knee have consistently failed to show an advantage over maximal medical therapy combined with physical therapy.36
Data Sources: The database Essential Evidence Plus was searched on February 24, 2010. A PubMed search using the key word osteoarthritis was performed in March 2010. The Cochrane Database of Systematic Reviews was searched for various osteoarthritis treatments. Additional articles were found using the search engine in MD Consult, as well as articles found in the reference section of several of the articles previously read.
