
Am Fam Physician. 2012;85(6):647-649
Author disclosure: No relevant financial affiliations to disclose.
A 13-year-old boy presented with left anterolateral knee pain, stiffness, and slight weakness. The pain and stiffness worsened with prolonged sitting and climbing stairs. The symptoms began after he tripped and fell on his knee 12 months prior. Other than a superficial cut, he had no other obvious injury after the fall.
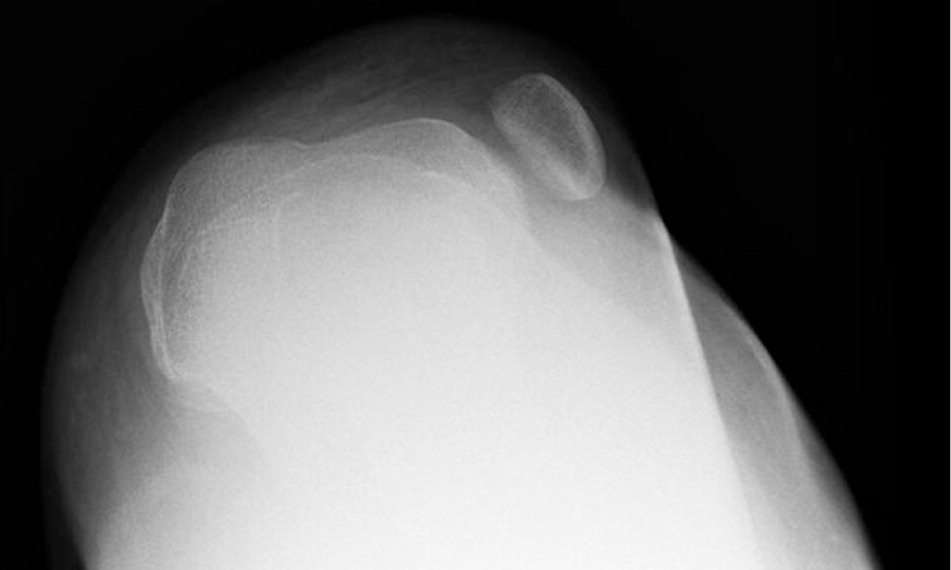
Examination revealed subtle swelling over the anterolateral aspect of his left knee (Figure 1). His left patella was nontender but palpable over the lateral epicondyle. He had decreased strength in his left quadriceps. During strength testing, he placed his right foot behind his left ankle to assist in extending his left lower leg. Results of apprehension, McMurray, Lachman, and varus and valgus stress testing were negative. Plain radiography was performed (Figure 2).


Question
Discussion
The answer is A: developmental dysplasia and dislocation of the patella. Developmental dysplasia of the patellofemoral joint primarily occurs in adolescents. The malformation contributes to patellar instability, dislocation, and anterior knee pain.1 The patient's diagnosis was confirmed with radiography showing abnormal flattening of the trochlear groove, which was not congruent with the patella (Figure 3). Developmental dysplasia has been reported in up to 85 percent of patients with recurrent patellar dislocation.2 The etiology of the dysplasia is poorly understood, but it can be congenital or acquired, suggesting a spectrum of disease.3 The prevalence of developmental dysplasia of the patellofemoral joint has been estimated at 0.7 to 2 percent.4
The annual incidence of acute patellar dislocation is estimated at 43 cases per 100,000 adolescents.5 Patellar dislocation is usually lateral. Patients with an acute dislocation have a painful, flexed knee with apprehension.5 Palpation can be useful in both acute and nonacute settings. The femoral condyle is easily identified medially, and the patella can be visualized laterally or palpated as a mass. In the nonacute setting, the patient often has tenderness over the medial patellofemoral ligament at the adductor tubercle.5 There may be atrophy of the quadriceps because the patient relies less on the extensor muscles of the affected leg. Risk factors include an increased Q angle, increased distance between the tibial tuberosity and trochlear groove, insufficiency of the medial patellofemoral ligament, hypoplasia of the vastus medialis oblique muscle, ligamentous laxity, and patella alta.4,5
Iliotibial band syndrome is an overuse condition that is more common in adults. It results from increased friction between the iliotibial band and the lateral femoral condyle.6 Pain occurs at the lateral aspect of the knee joint and is aggravated by activity, especially running and climbing stairs. On examination, there is tenderness to palpation over the lateral femoral condyle with flexion and extension of the leg (a positive finding on the Noble test).
Osgood-Schlatter lesion (tibial apophysitis) is an overuse injury in which the quadriceps pulls the apophysis of the tibial tubercle. It leads to anterior knee pain and usually occurs in an adolescent after a recent growth spurt.7 The pain is aggravated by prolonged sitting and by activities that cause forceful contractions of the quadriceps, such as climbing or descending stairs, squatting, or jumping. On examination, the tibial tuberosity is usually tender and swollen, and may be warm. Radiography is usually unremarkable but may show small spicules anterior to tuberosity.
Patella alta, or high-riding patella, is one of several skeletal abnormalities associated with patellar instability. In patella alta, the patella is situated superior to its usual anatomic location, but is not laterally displaced. This placement of the patella engages the femoral trochlea at increased angles of flexion, decreasing the amount of bony constraint on the patella at a given angle and predisposing it to dislocation.5
Patellofemoral pain syndrome usually affects active patients between 10 and 30 years of age.7 It is an overuse injury involving the patella and retinaculum, usually leading to anterior knee pain that increases with flexion and extension. Patients have pain with compression of the patella, as well as tenderness of the patella and retinaculum. Swelling and locking rarely occur, and the patellofemoral joint space appears normal on radiography. Patellofemoral pain syndrome is a diagnosis of exclusion and should be differentiated from intraarticular and patellar processes.
| Condition | Characteristics |
|---|---|
| Developmental dysplasia and dislocation of the patella | Radiography shows abnormal flattening of the trochlear groove, which is not congruent with the patella; dislocation is usually lateral; femoral condyle is easily visualized, and the patella can be visualized or palpated as a mass; knee maintained in flexed position |
| Iliotibial band syndrome | Overuse injury more common in adults; results from increased friction between the iliotibial band and the lateral femoral epicondyle; pain occurs at the lateral aspect of the knee joint and is aggravated by activity; positive Noble test result |
| Osgood-Schlatter lesion | Overuse injury in adolescents; quadriceps pulls the apophysis of the tibial tubercle, leading to anterior knee pain; pain increased with activity and prolonged sitting; radiographs are usually unremarkable, but may show small spicules anterior to the tuberosity |
| Patella alta | Common risk for recurrent dislocations; inferior pole of patella is superior to Blumensaat line, and tendon length is 20 percent longer than patella length |
| Patellofemoral pain syndrome | Overuse injury involving the patella and retinaculum, usually leading to anterior knee pain; increased pain with flexion-extension; swelling and locking rarely occur; normal patellofemoral joint space on imaging |
