
Am Fam Physician. 2013;87(9):645-646
Author disclosure: No relevant financial affiliations.
A 64-year-old man presented with lesions on the right side of his scrotum (Figure 1); they had been present for nearly 20 years. The patient reported no pain, oozing, or itching, and he had no history of trauma, injury, radiotherapy, surgery, or venereal infection.

Examination revealed multiple f luid-filled, translucent vesicles and bullae. The lesions were intact and were not fragile. A shave biopsy was obtained.
Question
Discussion
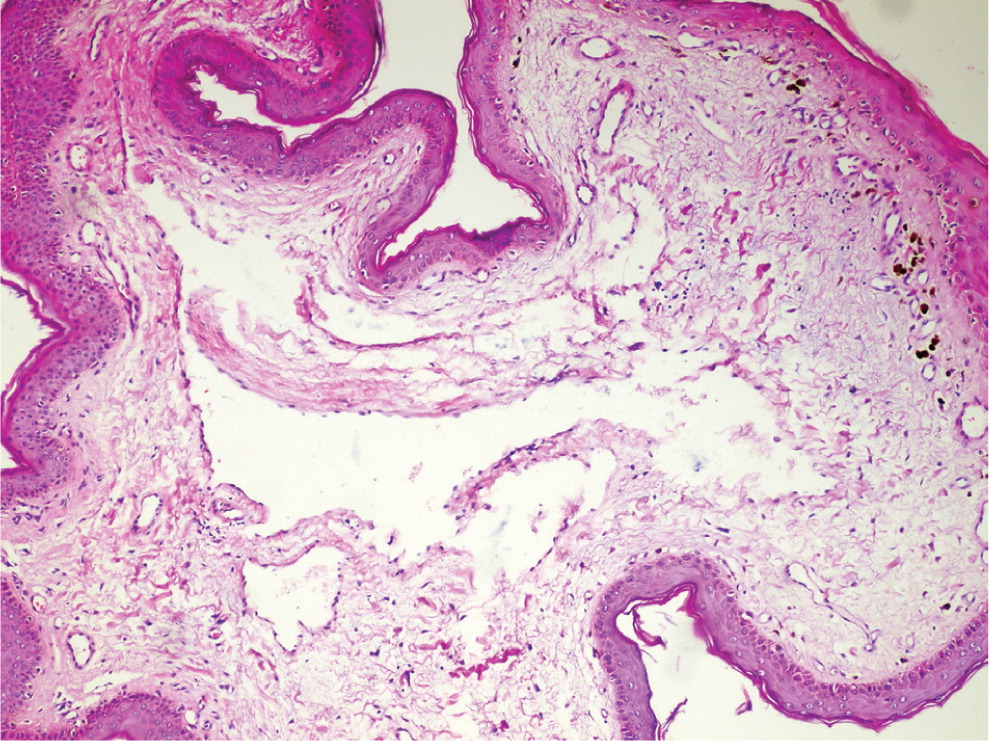
The answer is D: lymphangioma circumscriptum. Shave biopsy showed slight acanthosis in the epidermis and multiple dilated lymphatic vessels in the papillary dermis (Figure 2).
Lymphangiomas can be classified into three main types: cavernous, circumscriptum (capillary), and cystic.1 Lymphangioma circumscriptum, the most common type, is the benign dilatation and malformation of inner lymphatic channels located in the deep dermal and subcutaneous tissues.1,2 The disease often affects the proximal portions of the extremities, but scrotal, vulvar, and mucosal lesions are rare. Lymphangioma circumscriptum is more common in women than in men. It can occur at any age, but usually appears at or soon after birth.1
The clinical presentation is characterized by thin-walled vesicles and bullae, which are filled with translucent lymphatic fluid. The lesions range from 1 to 5 mm in size. Histopathologic features include numerous cystic lymphatic spaces lined with a flattened endothelium in the dermis. There may be overlying hyperkeratosis, acanthosis, hemorrhage, and mononuclear inflammatory cells.1,3
Angiokeratomas of Fordyce are well-circumscribed, vascular lesions characterized by red or blue papules (i.e., dilated vessels). They are commonly associated with severe varicosity or varicocele. Patients often report bleeding after sexual intercourse or excoriation of the lesions.4
Idiopathic scrotal calcinosis is a rare, benign condition that causes hard, yellowish nodules. The dermal nodules consist of calcium deposits under a normal epidermis. They are usually asymptomatic, but may itch or produce discharge.5
Leukemia cutis is the infiltration of neoplastic leukocytes into the skin, causing clinically identifiable cutaneous lesions. It is associated with a poor prognosis. The lesions consist of papules, but mostly nodules that are usually asymptomatic and typically seen with the nodular morphology. Leukemia cutis can be accompanied by hepatosplenomegaly or a high serum leukocyte count. Histopathology shows diffuse, band-like or nodular infiltration of leukemic cells.6
Steatocystoma multiplex is characterized by multiple dermal cysts involving the pilosebaceous units. The dermal cysts may be localized or widespread, and asymptomatic or inflammatory. Histopathology shows well-encapsulated cysts with cyst walls.7
| Condition | Characteristics |
|---|---|
| Angiokeratomas of Fordyce | Red or blue papules; bleeding after sexual intercourse or excoriation of the lesions; associated with severe varicosity or varicocele |
| Idiopathic scrotal calcinosis | Hard, yellowish dermal nodules consisting of calcium deposits under a normal epidermis; usually asymptomatic, but may itch or produce discharge |
| Leukemia cutis | Papules, but mostly nodules; accompanied by hepatosplenomegaly or a high serum leukocyte count; histopathology shows diffuse, band-like or nodular infiltration of leukemic cells |
| Lymphangioma circumscriptum | Thin-walled vesicles and bullae filled with translucent lymphatic fluid; histopathology shows numerous cystic lymphatic spaces lined with a flattened endothelium in the dermis |
| Steatocystoma multiplex | Multiple dermal cysts that are localized or widespread; asymptomatic or inflammatory; histopathology shows well-encapsulated cysts with cyst walls |
