
Am Fam Physician. 2013;87(12):877-879
Author disclosure: No relevant financial affiliations.
A 32-year-old woman presented to the emergency department with headaches and fevers that had persisted for the previous six weeks. The headaches were generalized and associated with nausea and photophobia. She had no focal weakness, numbness, or seizure activity. Her medical history was significant for AIDS, which was diagnosed three years earlier. She had not been taking antiretroviral drugs. Her last CD4 cell count was 282 per mm3 (0.28 × 109 per L), which was measured three months earlier.
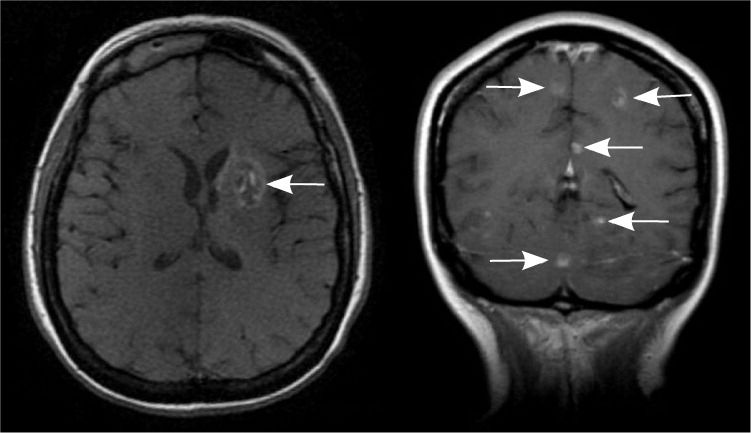
On examination, she had a temperature of 102°F (38.9°C) and marked wasting. She had no focal neurologic deficits. Magnetic resonance imaging of the brain showed multiple ring-enhancing lesions in the basal ganglia and cerebral hemispheres (see accompanying figure).
Question
Discussion
The correct answer is D: toxoplasmic encephalitis. Toxoplasmic encephalitis is the reactivation of disease from a prior parasitic infection. Patients may present with fevers, headaches, seizures, confusion, dementia, or focal neurologic deficits. Laboratory findings include polymerase chain reaction testing that is positive for Toxoplasma antigen in the cerebrospinal fluid, the presence of Toxoplasma antibodies indicative of past exposure, and a CD4 cell count less than 100 per mm3 (0.10 × 109 per L).
In this patient, a brain biopsy was positive for toxoplasmosis. Lesions are often multiple and localized to the parietal or frontal lobes, basal ganglia, or corticomedullary border.1 Magnetic resonance imaging demonstrates abscesses that are generally isodense or hypodense lesions, enhancing in a ring or nodular pattern with perifocal vasogenic edema and mass effect.2 Standard treatment is sulfadiazine and pyrimethamine (Daraprim), with leucovorin as needed, for a minimum of four to six weeks. Resumption of antiretroviral therapy is indicated to raise CD4 counts to more than 200 per mm3 (0.20 × 109 per L). If the lesions do not decrease in size within two weeks of initiating treatment, a brain biopsy is needed to exclude lymphoma.3
Human immunodeficiency virus encephalopathy presents with the triad of dementia, depression, and movement disorders. The most common finding on magnetic resonance imaging is cerebral atrophy. Multiple hyperintense lesions are nonenhancing, poorly demarcated, and localized bilaterally to the subcortical white matter.2 Lesions are usually symmetrical.
Primary central nervous system lymphoma is an extranodal non-Hodgkin lymphoma that can involve the brain, leptomeninges, eyes, or spinal cord without evidence of systemic disease. Patients present with confusion, memory loss, hemiparesis, aphasia, and seizures. Most patients have constitutional symptoms such as fever, night sweats, and weight loss. Epstein-Barr virus DNA may be found in the cerebrospinal fluid. The median CD4 cell count at the time of diagnosis is 50 per mm3 (0.50 × 109 per L). Lesions exhibit homogeneous contrast enhancement with edema and mass effect. Lesions that involve the corpus callosum, or the periventricular or periependymal area, and those larger than 3 cm are more likely to be caused by this condition.3,4 Brain biopsy is needed for definitive diagnosis.
Progressive multifocal leukoencephalopathy is a fatal demyelinating disease caused by reactivation of the JC virus in patients with severe immunosuppression. Patients present with rapidly progressive focal neurologic deficits and cognitive impairment. There are multifocal areas of demyelination, particularly in the periventricular areas and the subcortical white matter. On imaging, these lesions appear as bilateral, asymmetrical, hypodense, patchy or confluent white matter lesions.5 The lesions are nonenhancing without edema or mass effect. Diagnosis is made in patients with appropriate clinical features who have polymerase chain reaction testing positive for JC virus DNA in the cerebrospinal fluid.
Tuberculomas are granulomatous lesions that develop after recent or remote tuberculosis infection of the central nervous system. Patients present with focal neurologic symptoms and signs of an intracranial lesion, usually without evidence of systemic illness or meningeal inflammation. Tuberculomas may be solitary or multiple, and may show nodular enhancement.2
| Condition | Radiologic characteristics | Diagnosis |
|---|---|---|
| Human immunodeficiency virus encephalopathy | Nonenhancing, poorly demarcated, bilateral and symmetrical subcortical white matter lesions; cerebral atrophy | Clinical triad of dementia, depression, and movement disorder |
| Primary central nervous system lymphoma | Solitary or multiple lesions exhibit homogeneous contrast enhancement with mass effect; involve corpus callosum, or periventricular or periependymal areas | Brain biopsy shows diffuse B-cell lymphoma (rarely T-cell lymphoma) |
| Progressive multifocal leukoencephalopathy | Bilateral, asymmetrical, hypodense, patchy or confluent white matter lesions; nonenhancing without edema or mass effect; more common in periventricular areas and the subcortical white matter | PCR testing shows JC virus DNA in cerebrospinal fluid |
| Toxoplasmic encephalitis | Multiple ring-enhancing lesions with perifocal vasogenic edema and mass effect; more common in parietal basal ganglia, or corticomedullary border | PCR testing shows Toxoplasma antigen in cerebrospinal fluid |
| Tuberculoma | Solitary or multiple lesions are isointense, with a hyperintense ring on T1-weighted imaging and hypointense ring on T2-weighted imaging (but hyperintense lesions if there is liquefactive necrosis) | Recent or remote tuberculosis infection |
