
Am Fam Physician. 2013;88(8):515-519
Author disclosure: No relevant financial affiliations.
Ocular emergencies such as retinal detachments, mechanical globe injuries, and chemical injuries can cause permanent vision loss if they are not recognized and treated promptly. Family physicians should be familiar with the signs and symptoms associated with each condition, and be able to perform a basic eye examination to assess the situation. The assessment includes measurement of visual acuity, pupillary examination, visual field testing, slit lamp or penlight examination of the anterior segment of the eye, and direct funduscopic examination. Patients with symptomatic floaters and flashing lights require a dilated fundoscopic examination and prompt referral to an ophthalmologist for evaluation of a retinal tear or detachment. A globe laceration or rupture should be suspected in patients with a recent history of trauma from a blunt or penetrating object. Prophylactic oral antibiotics can be administered after a globe injury to prevent endophthalmitis, and the eye should be covered with a metal shield until evaluation by an ophthalmologist. Chemical injuries require immediate irrigation of the eye to neutralize the pH of the ocular surface.
Ocular emergencies have the potential to cause permanent vision loss if they are not promptly recognized and treated. Ocular emergencies include retinal detachments, mechanical globe injuries, and chemical injuries (Table 1). Family physicians should be familiar with the signs and symptoms associated with each condition, and be able to perform a basic eye examination to assess the situation.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Patients who notice symptomatic floaters and flashing lights should be referred immediately to an ophthalmologist for evaluation of a retinal tear or detachment. | C | 5 |
| Patients with a suspected globe injury should be referred immediately to an ophthalmologist. | C | 16, 17 |
| Prophylactic systemic antibiotics should be administered to prevent endophthalmitis after a globe rupture or laceration. | C | 20 |
| A chemical eye injury should be irrigated with lactated Ringer's solution or normal saline until the pH of the ocular surface is within the normal range. | C | 22, 27 |
| Emergency | Initial management | Ophthalmic management |
|---|---|---|
| Retinal tear or detachment | Refer to ophthalmologist immediately | Dilated fundoscopic examination; retinal laser for small retinal tear with no detachment; surgical repair with pneumatic retinopexy, scleral buckle, or vitrectomy for retinal detachment |
| Mechanical globe injury | Place metal shield over eye; prescribe antiemetics and systemic antibiotics; update tetanus immunization; refer immediately to ophthalmologist or emergency department | Orbital computed tomography to evaluate for fractures and intraocular foreign bodies; immediate surgery to repair the laceration; monitor for endophthalmitis and sympathetic ophthalmia |
| Chemical eye injury | Irrigate eye with normal saline or lactated Ringer's solution with at least 2 L of fluid; continue irrigation until pH is normal, then refer immediately to ophthalmologist or emergency department | Topical antibiotics and artificial tears for mild burns (grade I or II); topical antibiotics, artificial tears, steroids, ascorbate, and citrate drops for severe burns (grade III or IV) |
Retinal Detachment
ILLUSTRATIVE CASE
A 53-year-old man presents with a one-week history of acute vision loss in his right eye. He initially noticed several new floaters and a series of flashing lights. His central visual acuity was not affected, but he noticed a black spot in the inferior visual field that progressively enlarged. His visual acuity on presentation is 20/40, with a dense inferior scotoma on confrontational visual field testing (i.e., assessment in which the patient looks straight ahead as an object is brought in from the periphery).
BACKGROUND
Retinal detachment occurs when the neurosensory layer of the retina is separated from the underlying retinal pigment epithelium. Most retinal detachments are preceded by a posterior vitreous detachment, which causes traction on the retina and, potentially, a retinal tear. The liquefied vitreous can then seep through the tear and under the retina, causing it to detach. Retinal detachments may be localized initially, but without treatment they may progress and lead to irreversible vision loss.
The annual incidence of retinal detachment is estimated to be 12 in 100,000 persons.1 Risk factors include age, ocular trauma, cataract surgery, family history of retinal detachments, and a previous retinal detachment in the contralateral eye.2,3 Myopia is also a risk factor; patients with more than three diopters of refractive error have a 10-fold increased risk.4
DIAGNOSIS
Patients with a retinal detachment may initially notice unilateral flashing lights and an increase in floaters in the affected eye. They may have only a posterior vitreous detachment, but approximately one in five symptomatic patients develops retinal complications.5 In patients with only a retinal tear, vision may be unaffected or slightly cloudy. If a retinal detachment develops, they may have a visual defect in the peripheral vision that may expand over a few days. If the detachment involves the macula, it can cause a significant decrease in vision.
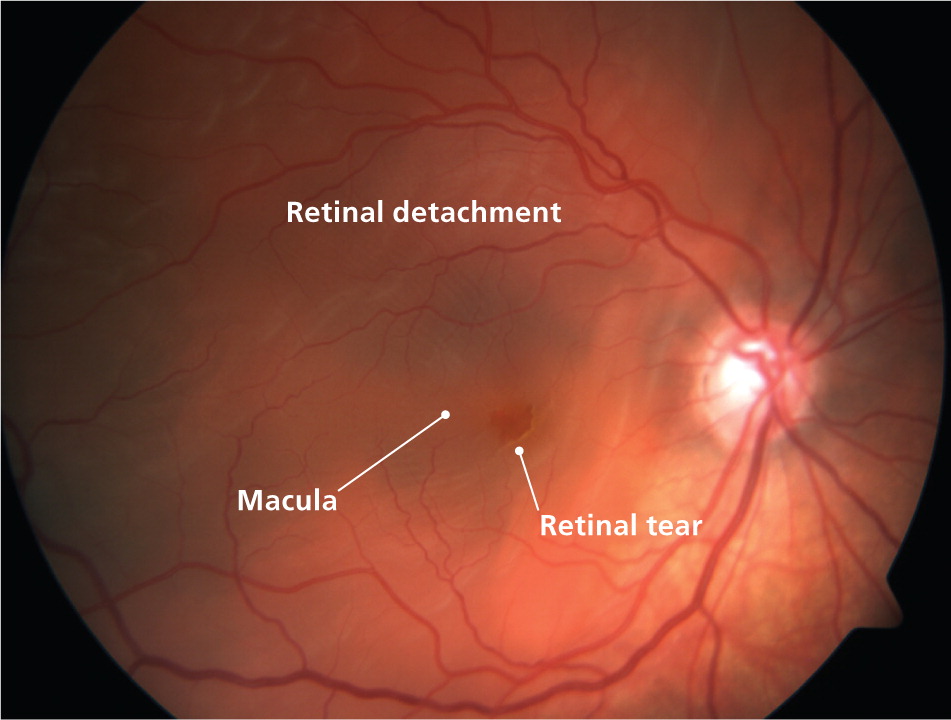
Dilated funduscopic examination can identify a retinal detachment. A retinal tear may be visible, and the surrounding retina may appear elevated (Figure 1). Diagnostic testing and imaging are not necessary if there is a good view of the fundus. If the retina cannot be adequately visualized because of a cataract, corneal scar, or vitreous hemorrhage, ocular ultrasonography is necessary to detect a retinal detachment.6
TREATMENT
Immediate ophthalmology referral is indicated if a retinal detachment is detected on initial examination and in patients with symptoms such as flashing lights, floaters, or a decrease in visual acuity.5 The only treatment for retinal detachment is surgery using laser photocoagulation to seal the retinal tear, then reattachment of the retina to the underlying retinal pigment epithelium. Surgical options, which are successful in more than 95% of cases, include pneumatic retinopexy, scleral buckle, pars plana vitrectomy, or a combination of these methods.7–10
PROGNOSIS
There is no consensus on the optimal surgical intervention to repair retinal detachments.11 However, untreated patients risk permanent and severe vision loss. Final visual acuity depends on whether the macula is attached at the time of diagnosis and intervention. Repair of retinal detachments results in a final visual acuity of at least 20/40 in approximately 75% of patients with an attached macula, compared with only 40% of those with a detached macula.12 One in four patients develops a retinal detachment in the contralateral eye; therefore, follow-up is necessary to examine the unaffected eye and to monitor for signs of proliferative vitreoretinopathy, which may cause a recurrent retinal detachment.13
Mechanical Globe Injury
ILLUSTRATIVE CASE
A 34-year-old man presents with acute right eye pain, redness, and loss of vision. Earlier that day, he was hammering a nail when he felt a foreign body strike his eye. His visual acuity on presentation is 20/200. Evaluation for corneal abrasion was performed with fluorescein staining. No corneal staining was visible under a cobalt blue light, but the fluorescein was rapidly diluted and a dark stream of fluid appeared.
BACKGROUND
Mechanical globe injuries occur when there is a full-thickness rupture or laceration through the cornea and/or sclera. Globe ruptures occur after blunt injury to the eye, such as from a thrown ball, motor vehicle crash, or assault. Globe lacerations occur after trauma from a sharp penetrating object, such as a knife or small, high-velocity projectile.
The annual incidence of mechanical globe injuries is 3.5 per 100,000 persons; most of these injuries occur in the workplace or during recreational activities.14 The type and cause of open globe injuries also vary with sex and age. Most mechanical globe injuries occur in males, who are more likely to have a penetrating injury early in life compared with females, who have more blunt trauma injuries later in life.15
DIAGNOSIS
Patients with a mechanical globe injury will often experience eye pain, redness, tearing, or decreased vision soon after blunt or sharp object trauma to their eye. If the patient does not have these symptoms but has a history of trauma via one of these mechanisms, the physician should consider the possibility of an occult injury.
An anterior segment examination with a penlight or, preferably, a slit lamp can help identify a globe injury. A subconjunctival hemorrhage, irregular pupil, and iris prolapse through a corneal or scleral wound are possible findings. If a foreign body is visible and protruding out of the globe, it should not be removed. Pupillary dilation and tonometry are not recommended. In uncertain situations, a wet fluorescein dye strip can be applied near the site of a possible rupture or laceration for examination under a cobalt blue light (part of the slit lamp evaluation; also may be found on some ophthalmoscopes). Dilution of the fluorescein by aqueous flow from the eye indicates a globe injury (i.e., positive Seidel test; see demonstration at http://www.youtube.com/watch?v=GlFcAv0DR4c). Computed tomography of the orbits is necessary to evaluate for intraocular foreign bodies or orbital wall fractures.
TREATMENT
Superficial conjunctival lacerations smaller than 1 cm that occur with no other ocular findings can be managed in the primary care setting with topical antibiotics. However, if a globe injury is diagnosed or suspected, pressure should not be placed on the eye, and the patient should be instructed to limit coughing or straining to prevent extrusion of the intraocular contents. Antiemetics are often administered to prevent the Valsalva maneuver and any further pressure on the globe. A metal shield should be placed over the eye, and the patient should be referred immediately to an ophthalmologist.16,17 Initial medical treatment consists of prophylactic systemic antibiotics with coverage against organisms associated with posttraumatic endophthalmitis, such as Staphylococcus aureus, Staphylococcus epidermidis, and Streptococcus species. The fluoroquinolones levofloxacin (Levaquin; 500 mg orally every 12 hours) and moxifloxacin (Avelox; 400 mg orally every 12 hours) have excellent vitreous penetration, and should be administered to patients with globe injuries.18,19 Alternatively, intravenous administration of vancomycin (1 g every 12 hours) or ceftazidime (Fortaz; 1 g every eight hours) may reduce the risk of posttraumatic endophthalmitis.20 A tetanus booster should also be administered, if necessary.
PROGNOSIS
Visual recovery from an open globe injury depends on several factors. Good initial visual acuity and smaller wound size (10 mm or less) are associated with a better prognosis. Conversely, poor outcomes are associated with posterior wound location; posttraumatic endophthalmitis; and afferent pupillary defect, a sign of severe damage to the retina or optic nerve that results in pupil dilation when a bright light is switched from the unaffected to the affected eye.18,21 Follow-up after a globe injury is necessary to monitor for sympathetic ophthalmia (i.e., intraocular inflammation of the unaffected eye). Although rare, this condition can lead to profound vision loss.
Chemical Injury
ILLUSTRATIVE CASE
A 20-year-old woman presents with pain, burning, tearing, and decreased vision in her right eye. Earlier that day, she poured a cleaning solution into the sink and instantly felt the liquid splash onto her face and eye. Her visual acuity on presentation is 20/400, and penlight examination shows swollen upper and lower eyelids, conjunctival injection, and an opaque cornea.
BACKGROUND
Chemical eye injuries occur after exposure of the ocular surface to an acid or alkali in the form of a liquid, powder, or gas. The severity of injury depends on the pH concentration of the chemical and the duration of contact with the ocular surface.22 Chemical burns damage the conjunctival and corneal epithelium and may cause ischemic damage to the conjunctival and scleral vessels, potentially affecting the entire anterior segment of the eye.
DIAGNOSIS
Patients with a chemical eye injury typically present with eye pain, redness, tearing, sensitivity to light, and decreased vision. To assess the severity of the injury, the physician should attempt to identify the type of chemical involved and how much of it came in contact with the eye.
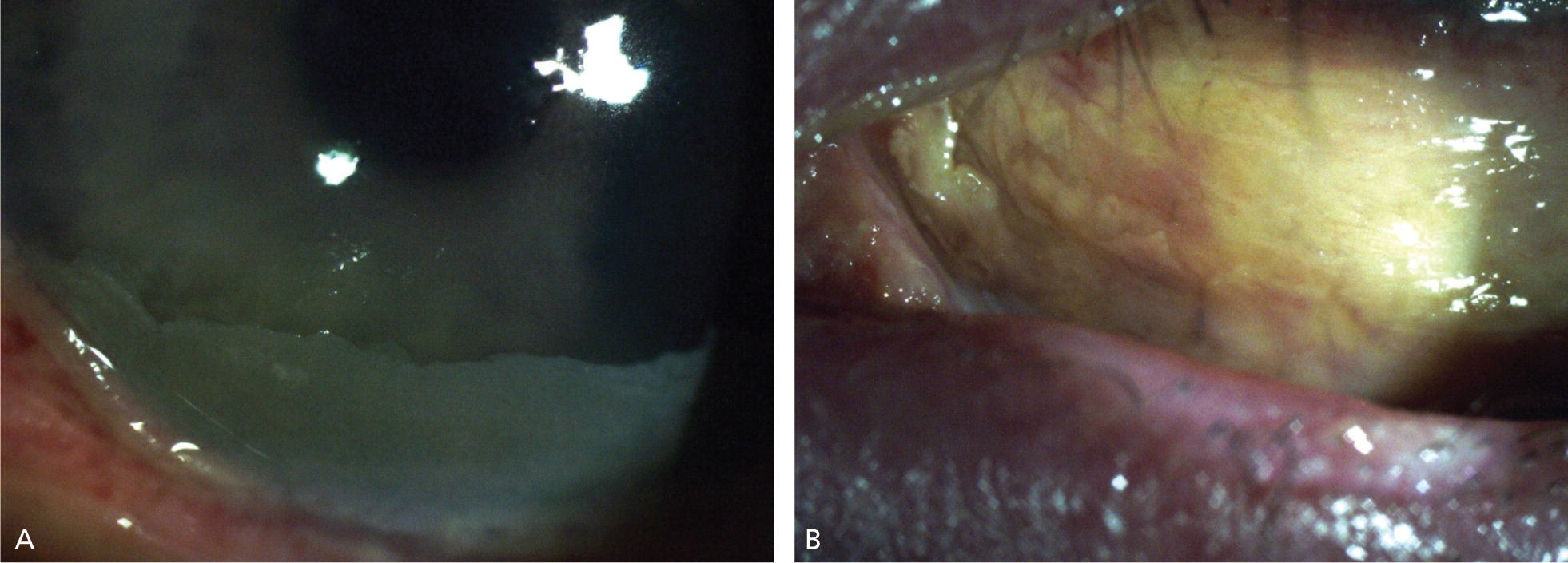
Examination of the external and anterior segment of the eye may reveal swelling and burns to the eyelids; a cloudy cornea; corneal epithelial defect; conjunctival injection; or a white eye, which indicates conjunctival ischemia (Figure 2). Initial testing of the ocular surface should be performed by placing a strip of litmus paper in the conjunctival fornix. The Roper-Hall classification system is used to describe the extent of injury; it is based on the degree of ischemia to the limbus (i.e., the junction between the cornea and sclera) and the degree of corneal haze (Table 2).25
| Grade | Corneal findings | Limbal ischemia | Prognosis |
|---|---|---|---|
| I | Mild epithelial damage | None | Good |
| II | Stromal haze with visible iris details | Less than one-third of limbus | Good |
| III | Stromal haze that obscures iris details | One-third to one-half of limbus | Guarded |
| IV | Opaque, no view of the iris | More than one-half of limbus | Poor |
TREATMENT
A chemical burn to the eye is an ocular emergency. Treatment should be initiated immediately because of the potential for permanent damage and vision loss. Initial treatment involves administering topical anesthetics to the eye, followed by copious irrigation with lactated Ringer's solution, normal saline, or water if other irrigation solutions are not available.22 The eye should be irrigated with at least 2 L of fluid using a lens irrigation system or intravenous tubing. The pH of the ocular surface should be remeasured five minutes after initial irrigation, and a wet cotton swab should be used to sweep the upper and lower fornices to remove any retained crystallized chemical particles. Further irrigation is necessary if the ocular surface has not been neutralized (pH of 7.0 to 7.5).
Once the ocular surface has been neutralized, the patient should be referred immediately to an ophthalmologist. Subsequent care depends on the extent of the injury. For mild burns (grades I and II), treatment with antibiotic eye drops and preservative-free artificial tears may suffice to promote corneal and conjunctival epithelial healing.26 Severe burns (grades III and IV) require topical antibiotics and artificial tears, as well as topical steroid, ascorbate, and citrate drops to reduce inflammation and promote epithelialization.26
PROGNOSIS
The prognosis depends on how quickly the eye is irrigated after a chemical injury; immediate irrigation results in less damage to the ocular surface and better visual outcomes.27 The prognosis also depends on the grade of the initial injury. In a retrospective study of patients with alkali burns, visual acuity was 20/40 or better in 100% of patients with grade I or II injuries, compared with 86% and 60% of patients with grade III or IV injuries, respectively.26 Long-term complications may occur, and follow-up is necessary to monitor for elevated intraocular pressure, corneal opacities, and eyelid abnormalities.
Data Sources: The Cochrane Database of Systematic Reviews, Agency for Healthcare Research and Quality, and U.S. Preventive Services Task Force were searched on September 6 and 9, 2011, using the keywords retinal detachment, mechanical globe injury, posttraumatic endophthalmitis, and ocular burn. A PubMed search was performed on September 13 and 16, 2011, using the same keywords.
