
Am Fam Physician. 2013;88(8):533-534
Author disclosure: No relevant financial affiliations.
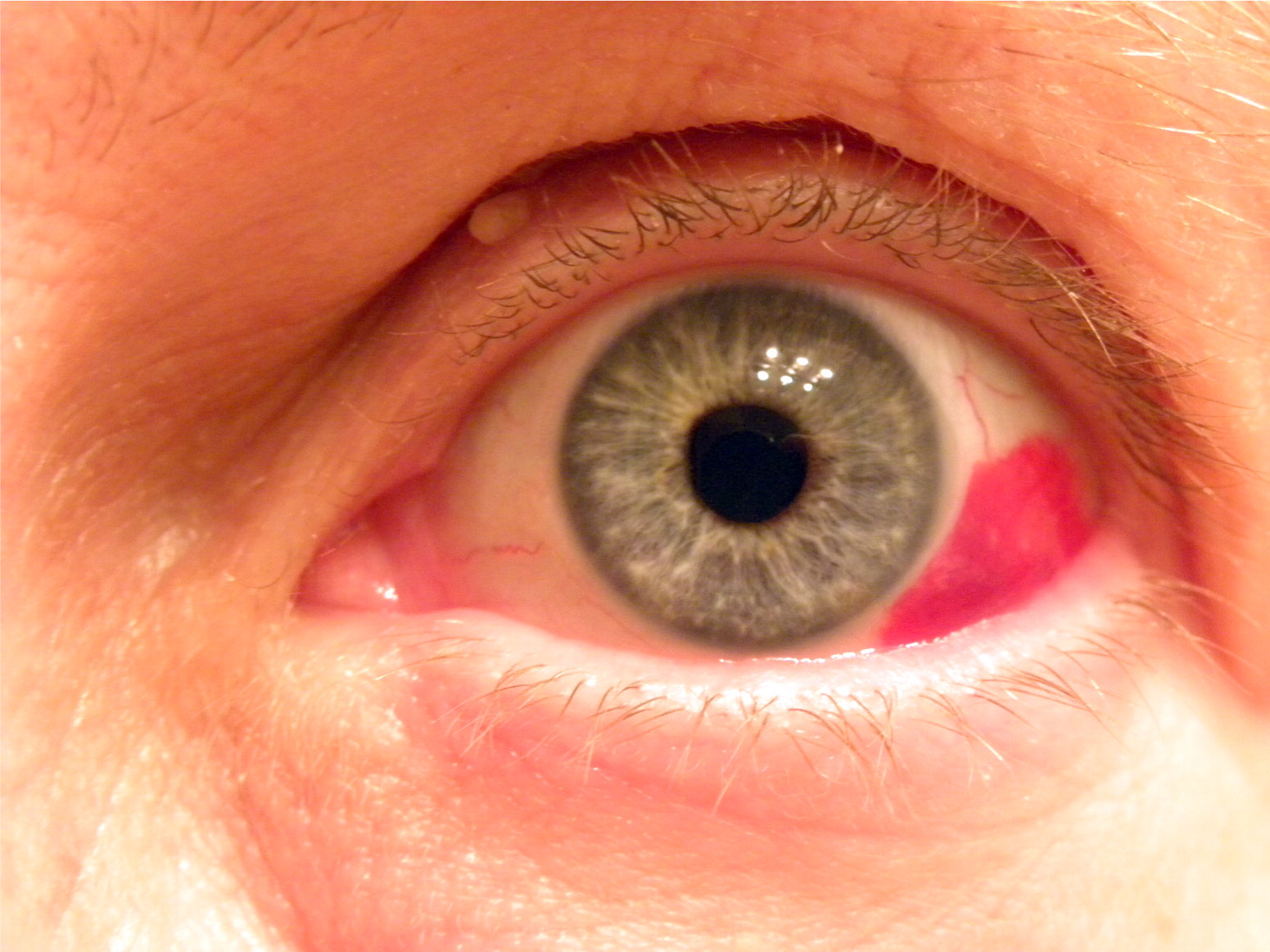
A 55-year-old woman presented with acute onset of redness in her left eye (see accompanying figure), which she noted upon awakening in the morning. She had no pain, ocular discharge, photophobia, blurry vision, or history of blunt trauma. On examination, she was normotensive. Her pupils were equal and reactive, and her corrected vision was 20/20.
Question
Discussion
The answer is D: subconjunctival hemorrhage. Subconjunctival hemorrhage is a common cause of red eye that is characterized by blood under the conjunctiva, usually localized to one sector of the eye.1 In severe cases, the entire sclera may be obstructed by blood. Patients with a subconjunctival hemorrhage are otherwise asymptomatic with no pain or vision changes. However, the patch of redness is sharply demarcated and often startles patients.
Most subconjunctival hemorrhages occur spontaneously or after minor, unnoticeable trauma, such as coughing, sneezing, or straining. If there is a history of trauma, a ruptured globe should be ruled out. Hypertension is the chief risk factor for a subconjunctival hemorrhage in older patients.2 Anticoagulant medications and bleeding disorders may also contribute to the condition.
Most subconjunctival hemorrhages resolve without treatment in approximately two weeks. Elevated blood pressure or suspicion of a bleeding disorder should prompt further evaluation.
Acute angle-closure glaucoma is characterized by diffuse conjunctival redness that is most pronounced adjacent to the limbus.3 Intraocular pressure is elevated. There is no discharge, but the pupil is mid-dilated and reacts poorly to light. Moderate to severe ocular pain may be accompanied by headache and blurry or decreased vision, and patients may report seeing halos around lights. The condition is usually unilateral. Abdominal pain, nausea, and vomiting may be present. All patients require urgent ophthalmologic referral.
Episcleritis is an inflammatory condition characterized by dilated episcleral vessels, giving the appearance of a red eye. Redness is usually localized, but can be diffuse. Vision is not affected, but patients often have a dull ache or tenderness over the injected area. The condition responds to oral nonsteroidal anti-inflammatory drugs or topical corticosteroids, and usually does not progress to scleritis. Nearly one-half of cases have bilateral involvement.4 Recurrent cases should prompt assessment for autoimmune disease.
A hyphema is caused by bleeding into the anterior chamber, leading to a layering of red blood cells in the eye that are visible without an ophthalmoscope or slit lamp. Patients often have a history of blunt trauma to the orbit. Hyphemas may cause decreased visual acuity, photophobia, and eye pain, but no discharge. Patients with a hyphema require assessment for other ocular injury, including penetrating eye trauma, and immediate ophthalmologic referral.
Viral conjunctivitis is one of the most common causes of red eye seen in primary care. It often accompanies an upper respiratory tract infection and is contagious. On physical examination, there is diffuse redness of the eye with a watery discharge, and pupils are reactive. Occasionally, patients describe a gritty sensation, but vision should be normal.
| Diagnosis | Characteristics |
|---|---|
| Acute angle-closure glaucoma | Diffuse conjunctival redness, especially adjacent to the limbus; ocular pain may be accompanied by headache and blurry or decreased vision; abdominal pain, nausea, and vomiting may be present; usually unilateral, pupil mid-dilated and nonreactive |
| Episcleritis | Localized or diffuse redness, dull ache, tender on palpation; normal vision; responds to corticosteroids or oral nonsteroidal anti-inflammatory drugs |
| Hyphema | Layering of blood in the anterior chamber; possible decreased visual acuity, photophobia, eye pain |
| Subconjunctival hemorrhage | Sharply demarcated area of bright redness; painless; normal vision; resolves spontaneously |
| Viral conjunctivitis | Diffuse redness, watery discharge; often associated with a viral upper respiratory tract infection |
