
Am Fam Physician. 2014;89(4):283-284
Author disclosure: No relevant financial affiliations.
A 26-year-old man presented with weakness on the right side of his face that occurred abruptly when he awoke that morning. He also had excess lacrimation in his right eye. About three days before onset of the facial weakness, he experienced mild right otalgia that resolved the same day. He did not have fever, visual changes, numbness, or hearing loss, but his sense of taste was altered. He had no significant medical history.
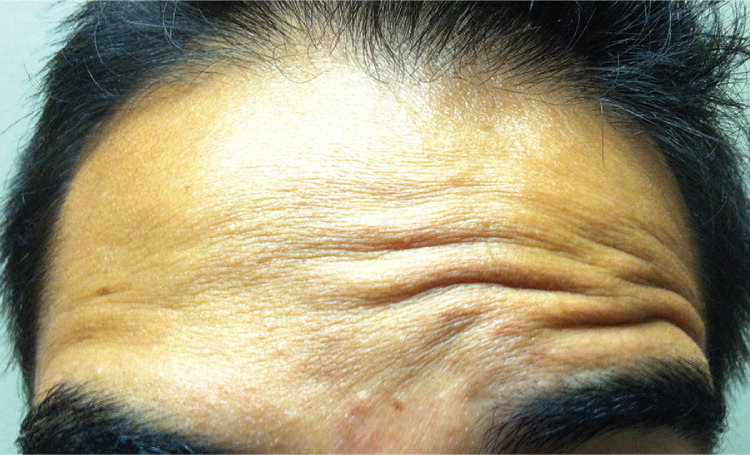
Physical examination revealed profound weakness of the muscles of facial expression on the right side (Figure 1). He was unable to activate the right brow depressors (Figure 2) or smile symmetrically (Figure 3). Other neurologic findings were normal. Magnetic resonance imaging of the head, with special focus on the right internal auditory canal, revealed no pathologic findings.


Question
Discussion
The correct answer is A: Bell palsy. Clinical characteristics of Bell palsy are caused by cranial nerve VII dysfunction and include sudden onset of unilateral paralysis, eyebrow droop, inability to close the eye, disappearance of the nasolabial fold, and mouth drawn to the unaffected side. It may be associated with loss of taste on the anterior two-thirds of the tongue, or with altered secretion of the lacrimal and salivary glands. The forehead muscles are typically involved in patients with Bell palsy, whereas they are usually spared in patients with upper motor neuron lesions, as seen with transient ischemic attacks or cerebral stroke.
The onset of Bell palsy is often acute, and the course is progressive. Symptoms can peak up to three weeks after onset of facial nerve dysfunction, and may linger up to six months. Without treatment, symptoms usually resolve within three to four weeks. An estimated 75% of all facial paralyses are of unknown etiology.1 The role of herpes simplex virus in Bell palsy is controversial.2
Chronic inflammatory demyelinating polyneuropathy affects peripheral nerves and nerve roots,3 and leads to symmetric motor involvement that is more pronounced than sensory. Weakness is present in proximal and distal muscles, although cranial nerve involvement is possible. On physical examination, the patient may have a decrease in vibratory sensation, proprioception, pain/temperature sensation, and reflexes.
Melkersson-Rosenthal syndrome, or cheilitis granulomatosa, is rare. Symptoms begin in adolescence, with recurrent facial palsy, facial edema, and lingua plicata.4 Facial palsy often occurs after facial swelling, but may appear months before. Facial palsy is intermittent; however, it may become permanent and can be unilateral, bilateral, partial, or complete. This condition can affect cranial nerves other than cranial nerve VII and is associated with tuberculoid granulomas in edematous tissue.
Most salivary gland tumors occur in the parotid gland. Parotid gland tumors may cause facial paralysis. Partial or complete facial nerve paralysis occurs in up to 23% of patients with malignant parotid lesions at presentation and is associated with a worse prognosis.5 A palpable parotid gland mass or swelling, or a unilateral facial palsy that does not improve, should raise suspicion for parotid gland tumor.
Transient ischemic attacks are episodes of focal neurologic or retinal dysfunction provoked by impaired blood supply to a specific vascular territory of the central nervous system without acute infarction. Symptoms may last from minutes to hours and are characterized by reversibility of the neurologic deficit. Therefore, it is important to recognize transient ischemic attack as a warning of impending stroke.6 There are a wide array of clinical presentations because any vascular territories of the central nervous system may be affected. Distribution of symptoms is often not localized. Pure motor hemiparesis can occur and is characterized by weakness involving the face, arm, and/or leg of one side of the body in the absence of sensory deficits or cortical signs.
| Condition | Characteristics |
|---|---|
| Bell palsy | Sudden onset of unilateral paralysis; eyebrow droop, inability to close the eye, disappearance of the nasolabial fold, mouth drawn to the unaffected side; may be associated with loss of taste on the anterior two-thirds of the tongue, or with altered secretion of the lacrimal and salivary glands |
| Chronic inflammatory demyelinating polyneuropathy | Symmetric motor involvement is more pronounced than sensory; proximal and distal weakness; decrease in vibratory sensation, proprioception, pain/temperature sensation, and reflexes is possible |
| Melkersson-Rosenthal syndrome | Facial edema and fissured tongue beginning in adolescence, with recurrent episodes of facial palsy; associated with tuberculoid granulomas in edematous tissue |
| Parotid gland tumor | Palpable parotid gland mass or swelling, or a unilateral facial palsy that does not improve |
| Transient ischemic attack | Transient episode of neurologic dysfunction lasting a few minutes to several hours; symptoms may be recurrent and are always reversible; wide range of areas are affected; presentations vary and can include dizziness, diplopia, dysarthria, hemianopia, numbness, focal hearing loss, and sometimes overwhelming stupor or coma |
