
Am Fam Physician. 2014;89(7):537-541
Patient information: See related handout on shoulder pain, written by the authors of this article.
Author disclosure: No relevant financial affiliations.
The overhead athlete is at unique risk for injury because of the mechanics associated with rapid shoulder elevation, abduction, and external rotation. Angulation of the humeral head against the posterosuperior glenoid can cause rotator cuff tendon and labral impingement. The throwing or striking motion of baseball, softball, water polo, tennis, racquetball, and volleyball may result in scapular dyskinesis, partial articular-sided supraspinatus avulsions, and posterosuperior labral tears. The SICK scapula syndrome (scapular malposition, inferior medial border prominence, coracoid pain and malposition, and dyskinesis of scapular movement) is thought to increase the risk of injury in the overhead athlete. Special physical examination maneuvers and magnetic resonance imaging may be helpful in diagnosing intra-articular pathology. Rehabilitation of injuries associated with internal impingement of the shoulder should include three basic components: strengthening, stretching, and sport-specific exercises. Arthroscopic surgery may be considered if symptoms do not improve after three months of conservative management.
Shoulder pain in the overhead athlete may result from fractures, nerve-related pathology, overuse, or articular, muscular, or tendon injuries. In sports such as baseball, softball, water polo, tennis, racquetball, and volleyball, the overhead throwing motion requires coordination from the feet to the hand in a single kinetic chain.1 This kinetic chain requires a coordinated delivery of muscle power to generate and transmit energy to throw or strike a ball. A break in this coordinated effort (even in the trunk or legs) can result in altered mechanics that may injure the shoulder2 via internal impingement and associated partial articular-sided supraspinatus avulsions and posterosuperior labral tears3 (Table 1). Athletes who routinely assume the overhead arm position (i.e., maximal external rotation of the humerus with shoulder abduction and elevation) are vulnerable to internal impingement from microinstability of the glenohumeral joint, overuse, or fatigue of the shoulder girdle muscles.4,5
| Clinical recommendations | Evidence rating | References |
|---|---|---|
| Scapular motion and position should be evaluated in overhead athletes with shoulder pain, and physical therapy should be initiated if dyskinesis is present. | C | 6–10 |
| Physical examination maneuvers and magnetic resonance arthrography accurately identify intra-articular shoulder injuries, but their diagnostic effectiveness is limited for partial-thickness rotator cuff tears. | C | 18, 20 |
| The Jobe relocation and O'Brien tests are the most reliable for identifying labral pathology. | C | 22 |
| The primary treatment for internal impingement of the shoulder is rehabilitation and physiotherapy consisting of stretching, strengthening, and sport-specific exercises. | C | 9, 21 |
| Condition | Mechanism | Presentation | Diagnosis | Treatment |
|---|---|---|---|---|
| Labral tear (posterosuperior) | Internal impingement of the shoulder | Pain during cocking phase of throwing or ball striking | Abnormal results on O'Brien test or other preferred test for superior labrum anteroposterior tears | Physical therapy and activity modification; may require surgery |
| PASTA injury (partial articular-sided supraspinatus tendon avulsion) | Internal impingement of the shoulder | Pain during cocking phase of throwing or ball striking | Abnormal results on empty-can test | Physical therapy and activity modification; may require surgery |
| SICK scapula syndrome (scapular malposition, inferior medial border prominence, coracoid pain and malposition, dyskinesis of scapular movement) | Aberrant muscle function around the scapula | Coracoid pain and pain with throwing | Abnormal positioning and dyskinesis of scapula | Physical therapy and activity modification |
SICK Scapula Syndrome
Scapular interaction with the thorax allows a wide range of mechanical motion.6 Normal scapular motion relies on a group of muscles known as scapular stabilizers, which are prone to imbalance and injury.7–9 The SICK scapula syndrome (defined by a posture of scapular malposition, inferior medial border prominence, coracoid pain and malposition, and dyskinesis of scapular movement) is thought to increase the risk of injury in the overhead athlete.7,9,10
The cocking or windup phase of throwing occurs when the arm moves in the opposite direction to the final direction of ball velocity. The glenohumeral joint normally abducts and rotates externally, and the scapula tilts posteriorly and rotates upward and externally, thus keeping the arm in the same plane as the scapula.6,9 The SICK scapula does the opposite: it tilts anteriorly and rotates downward and internally. These abnormal motions of the scapula increase the angulation of the humerus on the glenoid and decrease subacromial space, leading to pain and impingement, the precursors to rotator cuff and labral pathology.9 Repetitive positioning in this manner can result in shortening of the posterior capsule and can constrain glenohumeral internal rotation, worsening the SICK scapula.
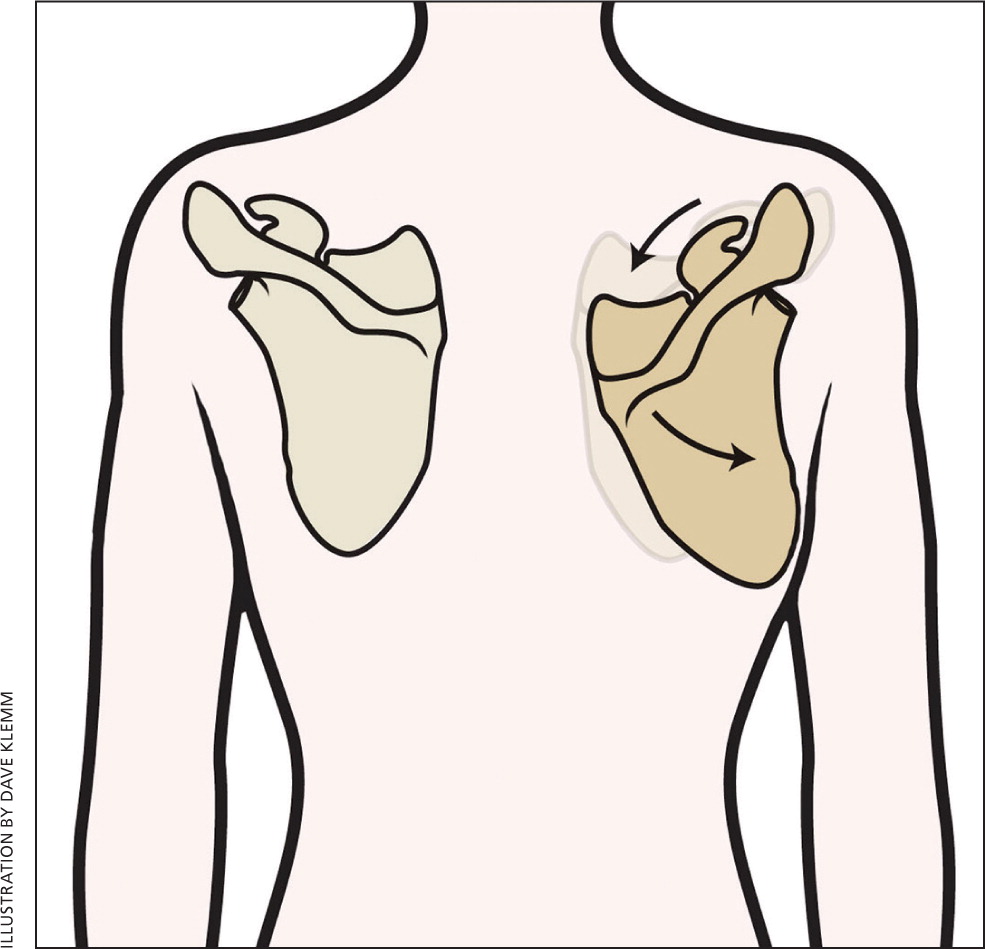
Clinical evaluation of the overhead athlete with shoulder pain should include passive examination of the scapula as well as observation during active range of motion.8,9 On passive physical examination, a SICK scapula will appear lower, with a prominent infperior medial border and tender coracoid7,9 (Figure 1). These characteristic changes result from weakness of the scapular stabilizers (serratus anterior, infraspinatus, deltoid, and lower and middle trapezius) and concomitant tension of opposing scapular stabilizers (levator scapulae, upper trapezius, and pectoralis).7,9 The coracoid will be tender to palpation, and patients will have pain with active flexion. On repeat examination during active range of motion, symptoms should resolve if the examiner stabilizes the upper scapula and assists with upward rotation.11
PASTA Injuries
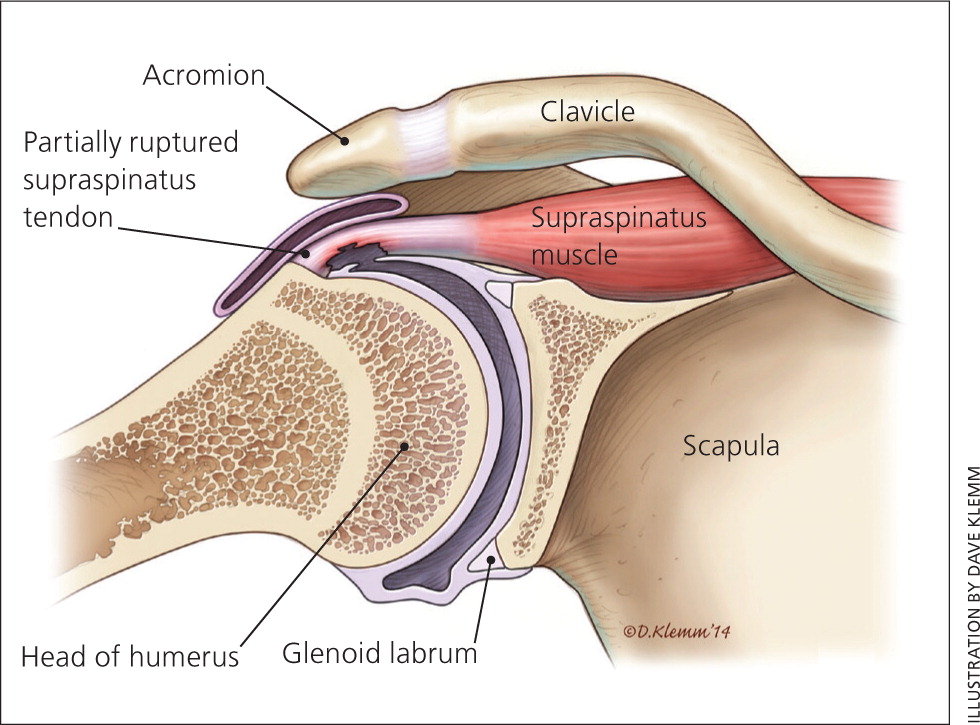
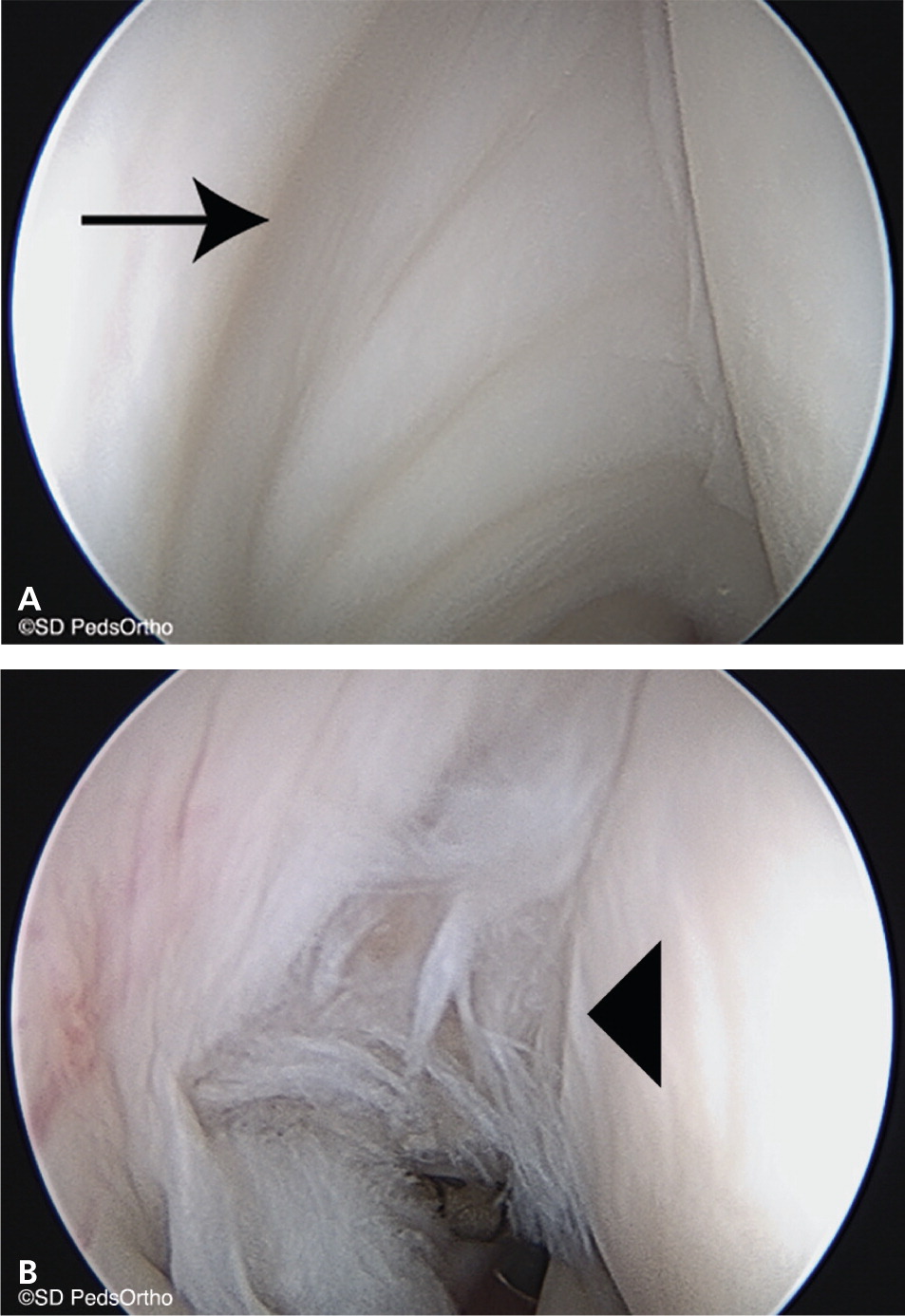
Rotator cuff tendon tears are rare in adolescents and young adults.12–14 However, partial articular-sided supraspinatus tendon avulsion (PASTA) injuries increasingly affect adolescents.12,15 As the humerus maximally externally rotates against the scapula in abduction, the fibers of the supraspinatus (and occasionally the infraspinatus) can become entrapped (Figure 2); repetition of this motion may result in a PASTA injury.16 Excessive external rotation in the cocking phase of overhead throwing may also contribute to avulsion of the articular side of the tendon. A grade 1 partial tear is less than 3 mm avulsed, grade 2 is 3 to 6 mm, and grade 3 is larger than 6 mm or more than 50% avulsed.17
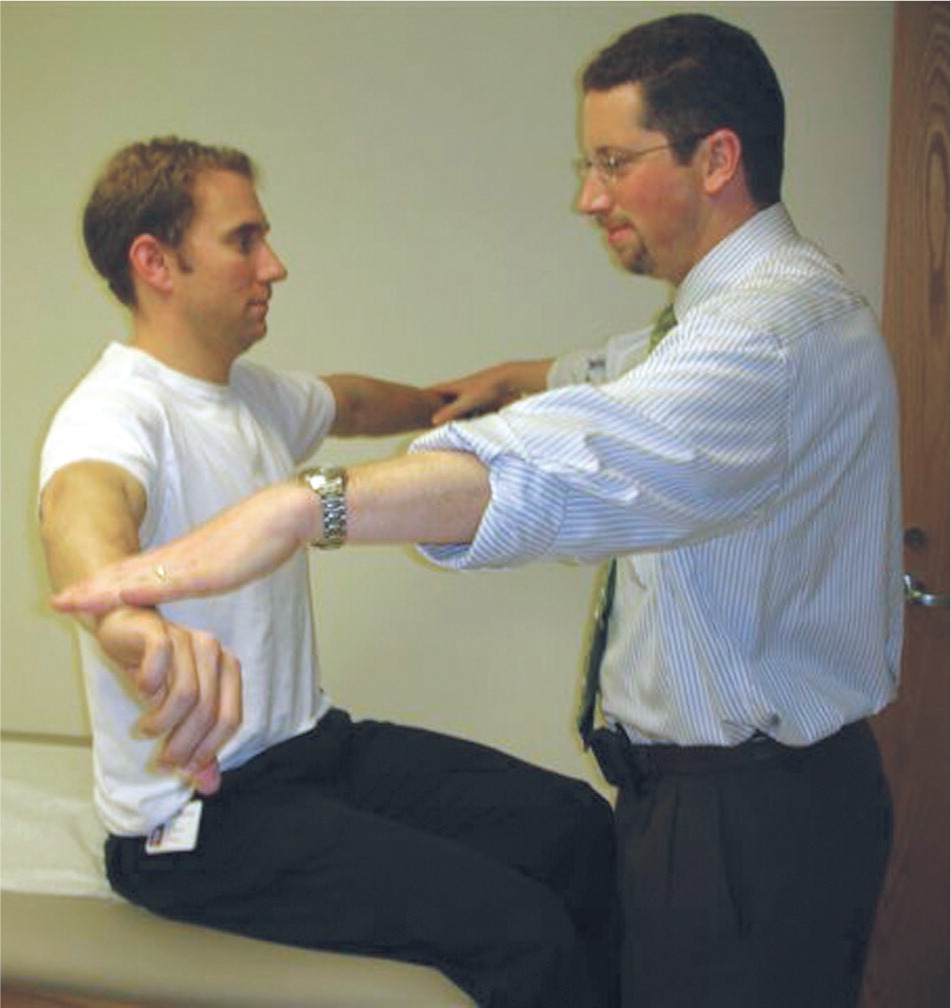
Diagnosing a partial tear of the rotator cuff tendon can be difficult. A systematic review demonstrated that physical examination maneuvers and magnetic resonance imaging were relatively accurate in diagnosing full rotator cuff tears, but were less sensitive and specific for partial tendon injuries.18 Specific tests that should be performed include the empty can test (Figure 3), as well as comparative testing of the rotator cuff musculature (Figures 4 and 5).19 The sensitivity and specificity of the empty can test are 70% and 58%, respectively, for a partial rotator cuff tear and 98% and 58% for a complete tear.20


Magnetic resonance arthrography is more accurate than magnetic resonance imaging (MRI) alone in identifying PASTA injuries.18 The sensitivity and specificity of magnetic resonance arthrography are 95% and 93%, respectively, for full-thickness rotator cuff tears, and 62% and 92% for partial-thickness tears.18
Labral Pathology
Superior labrum anteroposterior (SLAP) tears are the most common labral pathology in overhead athletes.21 Isolated tears of the posterosuperior labrum are less understood. However, it is thought that fraying or frank tears may occur in this region via internal impingement.22 The sensitivity and specificity of physical examination and MRI for labral tears are similar to those for PASTA injuries.22,23
Examination maneuvers that test labral integrity include the Jobe relocation test (supine patient with arm in maximal external rotation plus abduction, with posterior pressure applied to relieve apprehension), the O'Brien test (arm held horizontally 60 degrees out of scapular plane while actively resisting with thumb down, then up with resolution of pain), the anterior apprehension test (similar to Jobe relocation, but without maximal external rotation; anterior pressure causes apprehension), palpation of the bicipital groove, the crank test (pain elicited with supine circumduction of the humerus on the glenoid), Speed test (resisted forward elevation of humerus), and Yergason test (resisted forearm supination). The Jobe relocation and O'Brien tests are the most useful for identifying labral pathology (Table 220,22–24 ). None of the tests identify a SLAP tear specifically.23,24
| Condition | Test | Sensitivity (%) | Specificity (%) | Positive predictive value (%) | Negative predictive value (%) | Likelihood ratio |
|---|---|---|---|---|---|---|
| Labral pathology | Crank | 12.5 to 91 | 56 to 100 | 11 to 100 | 29.2 to 93 | 0.72 to 13.00 |
| O'Brien | 32 to 100 | 11.1 to 98.5 | 10 to 94.6 | 14.3 to 100 | 0.37 to 2.33 | |
| Speed | 6 to 100 | 11 to 98 | 8 to 46 | 53 to 96 | 0.33 to 3.33 | |
| Yergason | 12 to 13 | 87 to 100 | 44 to 100 | 53 to 71.1 | 0.92 to 3.00 | |
| Rotator cuff pathology | Cross-body | 17 to 25 | 79 to 81 | 10 to 45 | 62 to 89 | 0.78 to 1.25 |
| Empty can | 41 to 89 | 50 to 98 | 9 to 68 | 71 to 88 | 1.4 to 45.00 | |
| Hawkins | 69 to 88 | 43 to 48 | 17 to 45 | 71 to 92 | 1.33 to 1.54 | |
| Lift-off | 17 to 92 | 60 to 98 | NA | NA | 0.43 to 31.00 | |
| Speed | 33 to 40 | 70 to 75 | 14 to 50 | 67 to 89 | 1.10 to 1.62 |
Magnetic resonance arthrography has a sensitivity of 95% and specificity of 100% for anterior labral tears in adults; however, it is considerably less accurate for diagnosing superior and posterior tears (sensitivities of 60% and 50%, respectively).25 A study in children found that although MRI was more sensitive than physical examination in detecting anterior labral pathology, it was only 70% accurate in identifying tears that extended beyond the anteroinferior quadrant.26
Treatment
The primary treatment for internal impingement of the shoulder is nonsurgical management.9 Rehabilitation of the shoulder should include three basic components: strengthening, stretching, and sport-specific exercise. Strengthening should include the rotator cuff muscles as well as the core muscle groups (everything in the kinetic chain). Stretching should correct the internal rotation deficit, and should include the cross-arm stretch and sleeper stretch.27 If SICK scapula syndrome is present, stretching of the pectoralis minor is important.9 This is done by placing a towel or foam roller in line with the spine, lying supine on the roller, and, with assistance, pressing the shoulders posteriorly.
The time needed to restore function through physical therapy is variable and often dependent on the motivation of the patient; the type of injury may be less important in predicting response to treatment. A minimum of six weeks is usually necessary to gauge success, but three months is not uncommon.
Surgery for a partial rotator cuff tear is typically performed via arthroscopy (Figure 6). Grade 1 and 2 injuries that involve less than 50% thickness of the cuff tendon are usually debrided back to stable edges, whereas grade 3 tears should be repaired.28 There are many techniques for repair, with 86% to 89% of patients returning to their previous level of play.29 Debridement should be performed if fraying of the labrum is present. Surgical repairs of SLAP tears21 and PASTA injuries have similar outcomes.30
Data Sources: A literature search was performed using PubMed and Essential Evidence Plus. Keywords included adolescent, childhood, overhead athlete, shoulder pain, rotator cuff injury, scapular dyskinesis, and internal impingement. The search was limited to the English language. Search dates: February 2012 and December 2013.
