
Am Fam Physician. 2014;89(7):569-573
Patient information: A handout on this topic is available at https://familydoctor.org/familydoctor/en/diseases-conditions/intertrigo.html.
Author disclosure: No relevant financial affiliations.
Intertrigo is a superficial inflammatory dermatitis occurring on two closely opposed skin surfaces as a result of moisture, friction, and lack of ventilation. Bodily secretions, including perspiration, urine, and feces, often exacerbate skin inflammation. Physical examination of skin folds reveals regions of erythema with peripheral scaling. Excessive friction and inflammation can cause skin breakdown and create an entry point for secondary fungal and bacterial infections, such as Candida, group A beta-hemolytic streptococcus, and Corynebacterium minutissimum. Candidal intertrigo is commonly diagnosed clinically, based on the characteristic appearance of satellite lesions. Diagnosis may be confirmed using a potassium hydroxide preparation. Resistant cases require oral fluconazole therapy. Bacterial superinfections may be identified with bacterial culture or Wood lamp examination. Fungal lesions are treated with topical nystatin, clotrimazole, ketoconazole, oxiconazole, or econazole. Secondary streptococcal infections are treated with topical mupirocin or oral penicillin. Corynebacterium infections are treated with oral erythromycin.
Intertrigo is caused by cutaneous inflammation of opposing skin surfaces. It is more common in hot and humid environments and during the summer. Skin folds, including inframammary (Figure 1), intergluteal, axillary, and interdigital (Figure 2) areas, may be involved.1 Intertrigo is more common in young and older persons secondary to a weakened immune system, incontinence, and immobility, although it can occur at any age.2–4
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Intertrigo associated with Candida should be managed with topical antifungals applied twice daily until the rash resolves. | C | 14 |
| Fluconazole (Diflucan), 100 to 200 mg daily for seven days, is used for intertrigo complicated by a resistant fungal infection. Patients who are obese may require an increased dosage. | C | 14 |
| Skin barrier protectants, such as zinc oxide ointment and petrolatum, as part of a structured skin care routine that also includes gentle cleansing and moisturizing may reduce recurrent intertrigo infections. | C | 20, 21 |


Etiology and Predisposing Factors
Intertrigo most often occurs in patients with obesity (body mass index more than 30 kg per m2), diabetes mellitus, or human immunodeficiency virus infection, and in those who are bedridden. It also occurs in patients with large skin folds and those who wear diapers or other items that trap moisture against the skin. There is a linear increase in the severity of obesity and the presence of intertrigo.5 Patients who are obese sweat more profusely because of their thick layers of subcutaneous brown fat, generating more heat than persons with normal body mass.6 This increases thermal, frictional, and moisture components of the skin.5
As the stratum corneum becomes macerated because of hyperhydration, the friction intensifies and further weakens and damages the epidermal tissue. The condition can progress to severe inflammation and skin breakdown. This erosion of the epidermal barrier may create an entry point for micro-organisms that cause secondary infections.7
Clinical Manifestations
Intertrigo is often a chronic disorder that begins insidiously with the onset of pruritus, stinging, and a burning sensation in skin folds. Physical examination of the skin folds usually reveals regions of erythema with peripheral scaling. Intertrigo associated with a fungal superinfection may produce satellite papules and pustules. Candidal intertrigo (Figure 3) is often associated with a foul-smelling odor. In the presence of a bacterial superinfection, plaques and abscesses may form.8

Interdigital intertrigo (Figure 2) may be mild and asymptomatic, but also may lead to intense erythema and desquamation. The affected skin may have a foul odor and may be macerated and ulcerated with copious or purulent discharge. Patients with interdigital intertrigo and comorbidities such as obesity or diabetes are at greater risk of cellulitis.3 Interdigital intertrigo can progress to a severe bacterial infection with pain, mobility problems, erysipelas, cellulitis, abscess formation, fasciitis, and osteomyelitis causing pain so severe that the patient is unable to ambulate.3 Web space infections are typically caused by gram-positive cocci such as Staphylococcus and Streptococcus and may cause ulceration, fever, and chills.9 Foot care and patient education are key in preventing interdigital infections in patients with diabetes.10
Diagnosis
Intertrigo may be difficult to distinguish from other skin disorders, but the patient history will help in the diagnosis (Table 1).8 The history should include previous treatments, especially topical steroids and antibacterial soaps or ointments. Some steroids may cause atrophy and maceration, and some soaps and ointments may exacerbate skin inflammation. A visual inspection of the skin will help identify lesions in other areas.8
| Disease | Characteristics |
|---|---|
| Infectious diseases | |
| Candidiasis (moniliasis) | Superficial erythematous infection, commonly affecting moist, cutaneous areas of the skin; satellite pustules |
| Dermatophytosis (tinea corporis, tinea versicolor) | Pruritic infections of nonviable keratinized tissues, such as nails and hair; contains a leading scale |
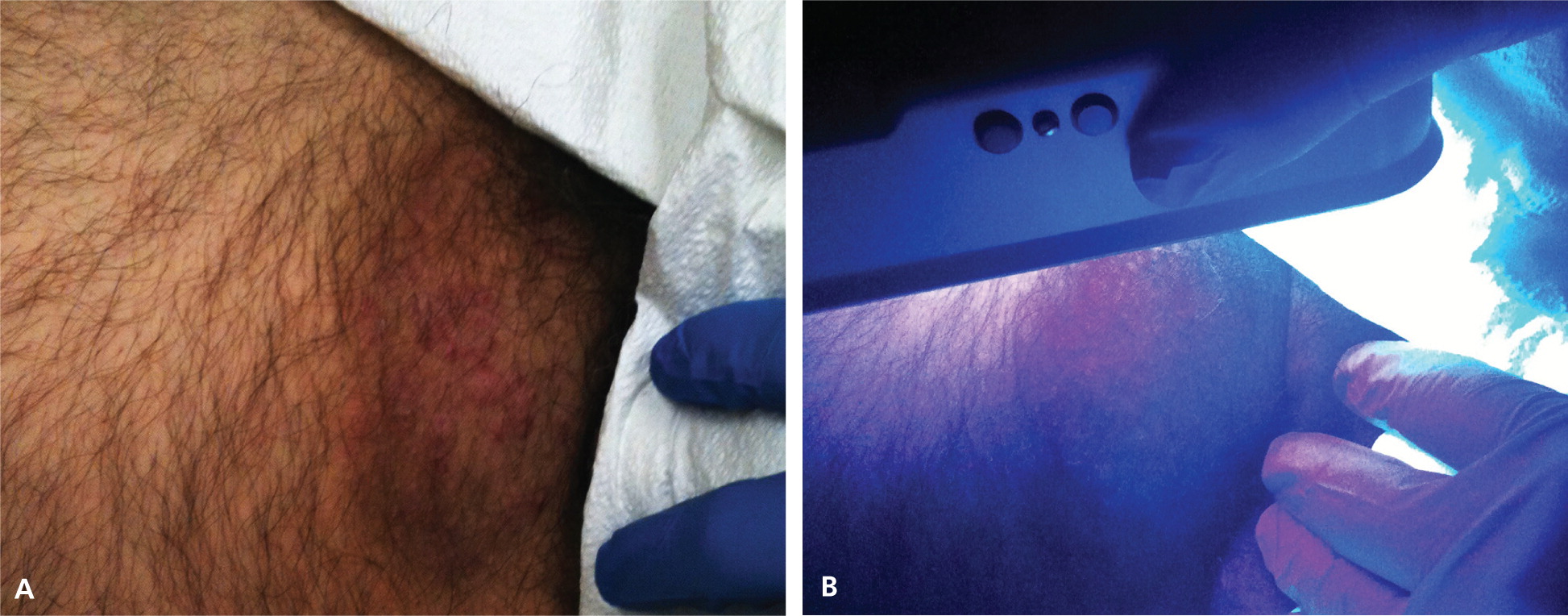
| Erythrasma | Small, red-brown macules that may coalesce into larger patches with sharp borders; may be asymptomatic or pruritic; fluoresces coral-red on Wood lamp examination |
| Pyoderma | Aggressive infection with boggy, blue-red bullae that progress to deep ulcers with hemorrhagic bases |
| Scabies | Infection with intense pruritus and minimal cutaneous manifestations, including intertriginous burrows and papules; the head is spared in all age groups except infants |
| Seborrheic dermatitis | Yellow, greasy, scaly plaques with overlying erythema; most often affects the face, postauricular region, and chest |
| Noninfectious inflammatory diseases | |
| Atopic dermatitis | Red or brownish patches with intense pruritus; personal and/or family history of seasonal allergies and asthma is common |
| Pemphigus vulgaris | Serious, often fatal, autoimmune disease; flaccid bullae, Nikolsky sign (i.e., disruption of the epidermal layer with lateral pressure, leading to ulceration) |
| Psoriasis | Chronic scaling papules and plaques; often affects extensor surfaces of the elbows and knees; associated with silvery scale |
| Noninflammatory diseases | |
| Acanthosis nigricans | Hyperpigmentation with velvety, thickened skin, predominantly on posterior neck and body folds |
| Hidradenitis suppurativa | Chronic condition of apocrine gland–bearing skin in the axillae or anogenital region; deep abscesses and old scars |
| Intertrigo | Pruritic regions of erythema and peripheral scaling between skin folds |
| Lichen sclerosus | Well-demarcated, hypopigmented, atrophic plaques on the genitalia, trunk, and axillae |
| Neoplasms | |
| Bowen disease | Solitary, enlarging, erythematous, well-defined plaque |
| Paget disease | Erythematous plaques with scaling, crusting, and/or exudation; affects the breast, axillae, or anogenital region; may represent a neoplastic process |
| Superficial basal cell carcinoma | Most common skin cancer; pink or flesh-colored papule often containing a telangiectatic vessel |
The diagnosis of secondary fungal infections is commonly made clinically, based on the characteristic appearance and distribution of satellite papules and pustules.11 The diagnosis may, however, be confirmed with a potassium hydroxide preparation positive for pseudohyphae and spores. Additionally, a potassium hydroxide preparation, Wood lamp examination, or culture of skin scrapings can diagnose conditions such as Candida or dermatophyte infections. The presence of hyphae on potassium hydroxide examination confirms dermatophytic lesions, including tinea versicolor and tinea corporis, and the presence of pseudohyphae confirms Candida infection. A video showing a potassium hydroxide examination of a fungal infection is available at http://www.youtube.com/watch?v=ugeMsyEDJaw. The Wood lamp examination fluoresces green with Pseudomonas infection and coral-red with erythrasma (Figure 4), a bacterial infection caused by Corynebacterium minutissimum.3
Treatment
| Condition | Treatments | |
|---|---|---|
| Intertrigo | Topical: zinc oxide ointment, petrolatum, talcum powder, aluminum sulfate, calcium acetate solution | |
| Intertrigo complicated by secondary bacterial infections | ||
| Erythrasma | Topical: erythromycin, clindamycin, Whitfield ointment, chlorhexidine | |
| Oral: erythromycin | ||
| Group A beta-hemolytic streptococcus | Topical: mupirocin (Bactroban), erythromycin, low-potency steroids | |
| Oral: penicillin, cephalexin (Keflex), ceftriaxone (Rocephin), cefazolin, clindamycin | ||
| Intertrigo complicated by secondary fungal infections | ||
| Candida | Topical: nystatin, clotrimazole, ketoconazole, oxiconazole (Oxistat), econazole | |
| Oral: fluconazole (Diflucan; used for resistant cases) | ||
| Dermatophytes | Topical: clotrimazole, ketoconazole, oxiconazole, econazole | |
BARRIER AGENTS
In uncomplicated intertrigo, numerous agents and mechanisms can be used to keep the skin folds dry, clean, and cool. Applying barrier protectants reduces skin breakdown and alleviates pruritus and pain. Skin protectants include zinc oxide ointment and petrolatum.12 Separating skin surfaces with absorbent products, such as gauze, cotton, and products with water vapor–permeable sheets, may also help reduce friction.
DRYING AGENTS
Aluminum sulfate, calcium acetate solution, and antiseptic drying agents (e.g., talcum powder) may be used.11,13 Powder drying agents should not be applied at the same time as antifungal creams or ointments because this will create a tacky paste. If both are used, they should be applied two to three hours apart. If symptoms do not improve after treatment, potassium hydroxide preparation, and bacterial culture and sensitivity testing should be performed.
SECONDARY FUNGAL INFECTIONS
Intertrigo complicated by fungal infection should be managed with topical antifungals. Nystatin is effective only for candidal intertrigo. Clotrimazole, ketoconazole, oxiconazole (Oxistat), or econazole may be used for both Candida and dermatophyte infections. Topical treatments are applied twice daily until the rash resolves. Fluconazole (Diflucan), 100 to 200 mg daily for seven days, is used for resistant fungal infections, although patients who are obese may require an increased dosage. Oral azoles may potentiate the effects of hypoglycemic agents, leading to low blood glucose levels, and patients with diabetes should be instructed to monitor their blood glucose levels with concomitant use of these medications.14
SECONDARY BACTERIAL INFECTIONS
The moist, damaged skin associated with intertrigo provides an opportunistic environment for bacterial microorganisms; therefore, secondary cutaneous infections are common. Staphylococcus aureus infection may occur independently or with group A beta-hemolytic streptococcal infection.15 Pseudomonas aeruginosa, Proteus mirabilis, or Proteus vulgaris also may be present independently or simultaneously.
The optimal treatment for patients with intertrigo and group A beta-hemolytic streptococcal infections includes single or multiple regimens of topical therapies (e.g., mupirocin [Bactroban], erythromycin); oral antibiotics (e.g., penicillin, first-generation cephalosporins); and low-potency topical steroids (e.g., hydrocortisone 1% cream).3,15 Low-potency topical steroids can also be useful to treat intertrigo associated with seborrheic or atopic dermatitis.16
Cutaneous erythrasma is best managed with erythromycin (topical, applied twice daily until rash resolves, or oral, 250 mg four times daily for two weeks).3,17,18 Oral erythromycin is more effective than a topical regimen, but it can cause adverse reactions, such as nausea, vomiting, abdominal pain, and diarrhea.3,17,18 Topical clindamycin, Whit-field ointment, and antibiotic soaps may also be beneficial.17
Preventing Recurrent Infections
Keeping the area affected by intertrigo dry and exposed to air can help prevent recurrences. Weight loss should be encouraged if obesity is a predisposing factor. Some patients with large, pendulous breasts may benefit from reduction mammoplasty.19
Data Sources: In conducting our literature search, we used Cochrane, UpToDate, PubMed, and Google Scholar. We used the keywords intertrigo, fungal infections, and secondary skin infections. Search dates: July 2012 and January 2014.
