Am Fam Physician. 2014;89(8):649-657
Author disclosure: No relevant financial affiliations.
The elbow is a complex joint designed to withstand a wide range of dynamic exertional forces. The location and quality of elbow pain can generally localize the injury to one of the four anatomic regions: anterior, medial, lateral, or posterior. The history should include questions about the onset of pain, what the patient was doing when the pain started, and the type and frequency of athletic and occupational activities. Lateral and medial epicondylitis are two of the more common diagnoses and often occur as a result of occupational activities. Patients have pain and tenderness over the affected tendinous insertion that are accentuated with specific movements. If lateral and medial epicondylitis treatments are unsuccessful, ulnar neuropathy and radial tunnel syndrome should be considered. Ulnar collateral ligament injuries occur in athletes participating in sports that involve overhead throwing. Biceps tendinopathy is a relatively common source of pain in the anterior elbow; history often includes repeated elbow flexion with forearm supination and pronation. Olecranon bursitis is a common cause of posterior elbow pain and swelling. It can be septic or aseptic, and is diagnosed based on history, physical examination, and bursal fluid analysis if necessary. Plain radiography is the initial choice for the evaluation of acute injuries and is best for showing bony injuries, soft tissue swelling, and joint effusions. Magnetic resonance imaging is the preferred imaging modality for chronic elbow pain. Musculoskeletal ultrasonography allows for an inexpensive dynamic evaluation of commonly injured structures.
Determining the underlying etiology of elbow pain can be difficult because of the complex anatomy of this joint and the broad differential diagnosis. As with other musculoskeletal problems, the keys to diagnosing elbow pain are a history to include mechanism of injury or exacerbating movements, and a focused physical examination. The patient's occupation and recreational activities can be important clues to diagnosis. Table 1 provides the differential diagnosis of elbow pain by anatomic location.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| If an ulnar collateral ligament injury is suspected, the medial joint space of the symptomatic elbow should be compared with the asymptomatic side for the amount of opening, the subjective quality of the end point while a valgus force is applied across the joint, and pain. | C | 7, 8, 12 |
| In patients with signs of compressive ulnar neuropathy at the cubital tunnel, a physical examination of the upper extremities and cervical spine is essential to rule out other compressive neuropathies. | C | 14, 20, 21 |
| To avoid introducing infection, aspiration of olecranon bursitis should be performed only when the diagnosis is uncertain or to relieve symptoms in refractory cases. | C | 24 |
| Magnetic resonance imaging is the preferred imaging modality for chronic elbow pain. | C | 37, 38 |
| Anterior |
| Anterior capsule strain |
| Biceps tendinopathy |
| Gout |
| Intra-articular loose body |
| Osteoarthritis |
| Pronator syndrome |
| Rheumatoid arthritis |
| Lateral |
| Lateral epicondylitis |
| Osteochondral defect |
| Plica |
| Posterolateral rotatory instability |
| Radial tunnel syndrome/posterior interosseous nerve syndrome |
| Medial |
| Cubital tunnel syndrome |
| Medial epicondylitis |
| Ulnar collateral ligament injury |
| Valgus extension overload syndrome |
| Posterior |
| Olecranon bursitis |
| Olecranon stress fracture |
| Osteoarthritis |
| Posterior impingement |
| Triceps tendinopathy |
Anatomy
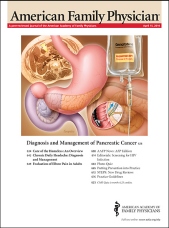
The elbow is primarily a hinged joint, but possesses the unique ability to rotate the distal arm in pronation and supination (Figure 11 ). These unique motions, along with a wide range of dynamic exertional forces, predispose the elbow and its structures to significant injuries, particularly with repetitive motions. Understanding the anatomy and the physical forces of movement will aid in diagnosis.2
Anterior Elbow Pain
BICEPS TENDINOPATHY
The biceps tendon is a relatively common source of pain in the anterior elbow. Although distal biceps tendon ruptures are rare, comprising 3% of all tendon ruptures, distal biceps tendinopathy is more common.3 This condition presents with an insidious course of anterior elbow pain, especially with resisted flexion and resisted supination of the forearm. Patients with biceps tendinopathy may present with vague anterior elbow pain. History often includes repeated elbow flexion with forearm supination or pronation, such as in dumbbell curls. On physical examination, with the elbow flexed to 90 degrees, passive supination and pronation of the forearm should reveal a normal piston-like movement of the biceps muscle belly. Absence of this motion indicates a complete tear. Resisted supination typically recreates pain deep in the antecubital fossa. The hook test, which involves the examiner hooking the biceps tendon with his or her fingertip, will confirm an intact tendon and may assist in localizing the pain generator (Figure 2). Magnetic resonance imaging (MRI) or musculoskeletal ultrasonography can be used to demonstrate continuity and changes in caliber of the tendon.4

OTHER CAUSES
Uncommon etiologies of anterior elbow pain include intra-articular processes such as osteoarthritis, rheumatoid arthritis, and gout.
Medial Elbow Pain
MEDIAL EPICONDYLITIS (GOLFER'S ELBOW)
Medial epicondylitis is much less common than lateral epicondylitis and typically occurs in athletes or workers who participate in activities that involve repetitive valgus stress and flexion at the elbow, as well as repetitive wrist flexion and pronation. It is a tendinopathy of the common flexor tendon, usually the flexor carpi radialis and the pronator teres.1,5
Patients typically report the insidious onset of pain at the medial elbow with or without accompanying grip-strength weakness. The point of maximal tenderness is usually at the insertion of the flexor-pronator mass, 5 to 10 mm distal and anterior to the medial epicondyle. Pain during resisted pronation is the most sensitive physical examination finding. The pain can also usually be recreated with resisted wrist flexion.6
ULNAR COLLATERAL LIGAMENT INJURY
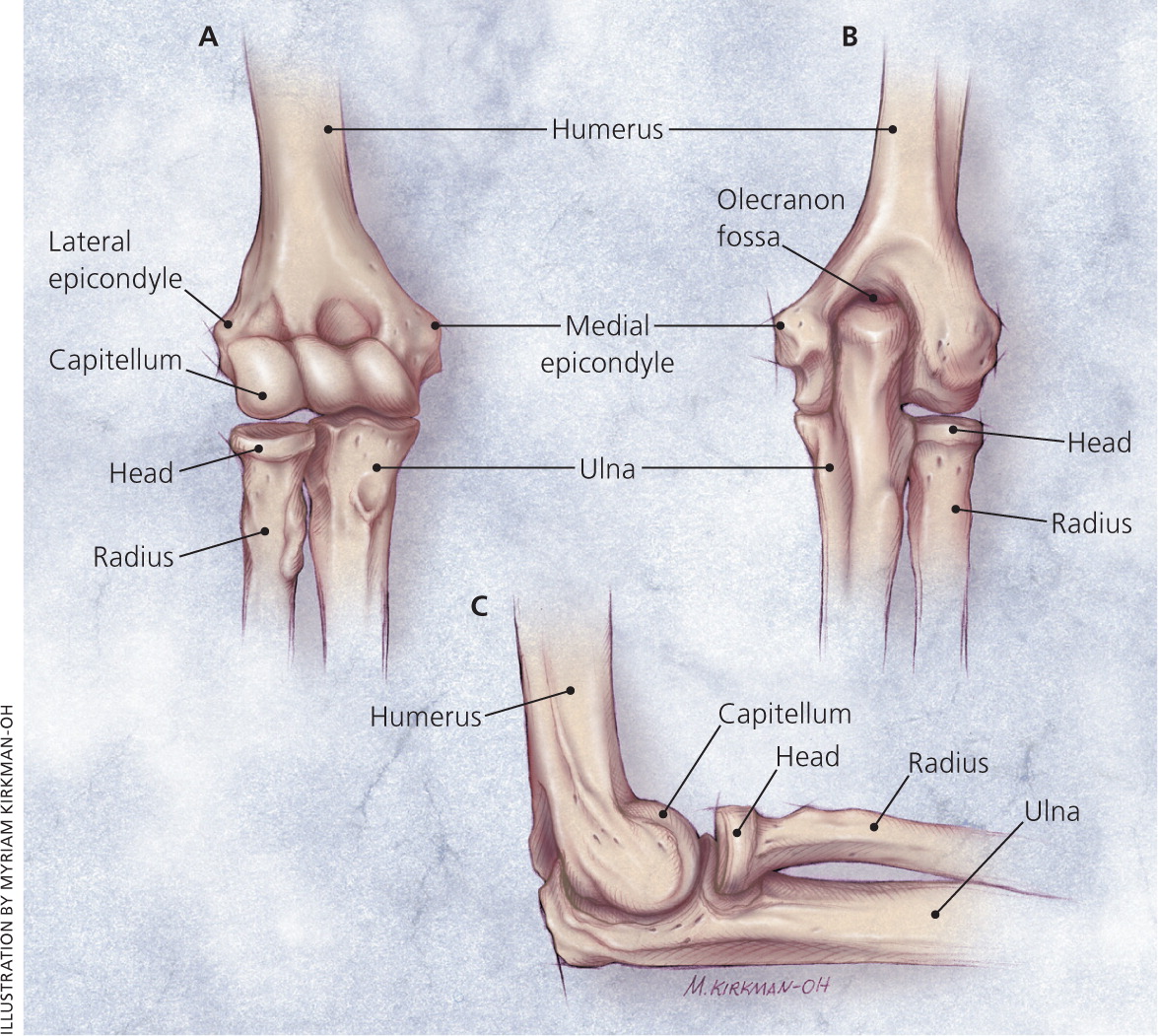
The anterior bundle of the ulnar collateral ligament (UCL) is the primary restraint to valgus stress during overhead throwing (Figure 3). UCL injuries commonly occur in athletes participating in sports that involve overhead throwing, such as baseball, javelin, and volleyball.7-9 Injury to the UCL results in significant valgus elbow instability and may predispose an athlete to secondary injuries.8,10
The history should include questions about the onset of pain, what the patient was doing when the pain started, sports played, and the frequency of participation. Patients with an acute UCL injury usually report the sensation of a pop followed by the immediate onset of pain and bruising around the medial elbow. Tenderness over the UCL has a sensitivity of 81% to 94%, but a specificity of only 22% for UCL tears.11
The most important examination for a possible UCL injury is assessment of the medial joint space laxity or instability against valgus forces. The medial joint space of the symptomatic elbow should be compared with the asymptomatic side for the amount of opening, the subjective quality of the end point while a valgus force is applied across the joint, and pain. A normal joint space will open less than 3 mm, with a firm end point.7,8,12
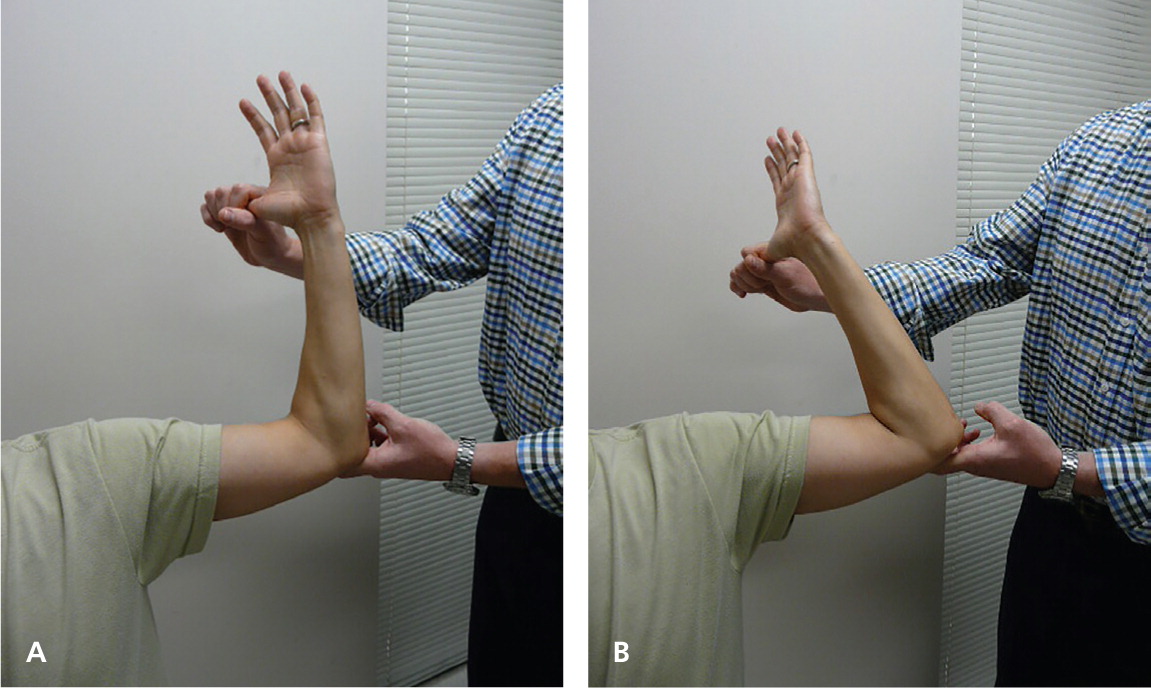
The moving valgus stress test (Figure 4) has a 100% sensitivity and a 75% specificity for diagnosing UCL injuries (Table 23,7,8,11,13–17 ). This test is performed with the shoulder in 90 degrees of abduction and external rotation. While maintaining constant valgus torque on the elbow, the elbow is quickly flexed and extended. A positive result is defined as pain between 70 and 120 degrees of flexion.11 A video of the moving valgus stress test is available at http://www.youtube.com/watch?v=plk7G2s8V30.
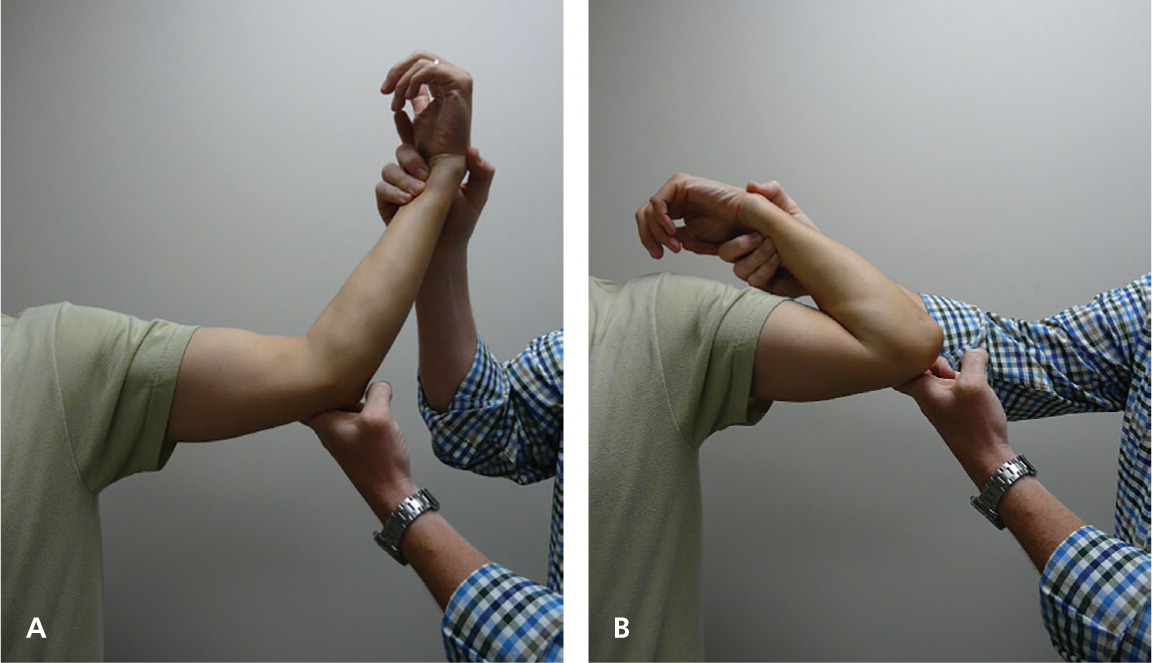
The milking maneuver (Figure 5) can provide additional information on the possible presence of a UCL injury. This maneuver is performed with the forearm supinated, shoulder abducted, and elbow flexed beyond 90 degrees. The examiner then pulls the patient's thumb posteriorly, creating a valgus force (Table 23,7,8,11,13–17 ). Patients with a UCL injury will have pain, instability, and apprehension.11
| Test | How performed | Positive findings | Suggested diagnosis |
|---|---|---|---|
| Elbow abduction stress test | Valgus stress applied against an elbow held in 20 to 30 degrees of flexion | Absence of a firm end point and movement of the articular surfaces of the medial epicondyle and ulna | Ulnar collateral ligament injury |
| Hook test | Shoulder abducted to 90 degrees with the elbow in 90 degrees of flexion | Finger does not hook onto the biceps tendon | Distal biceps tendon rupture |
| Examiner's finger attempts to hook behind the distal biceps tendon | |||
| Middle finger test | With an outstretched arm, the patient attempts to extend the middle finger against resistance | Weakness or inability to resist force | Posterior interosseous nerve compression syndrome |
| Pain isolated at the lateral epicondyle | Lateral epicondylitis | ||
| Milking maneuver | Forearm supinated, shoulder abducted, and elbow flexed beyond 90 degrees | Apprehension, instability, and medial joint pain | Ulnar collateral ligament injury |
| Valgus stress is placed on the elbow by pulling on the thumb | |||
| Modified milking maneuver | Shoulder adducted and externally rotated | Apprehension, instability, and medial joint pain | Ulnar collateral ligament injury |
| Moving valgus stress test | Shoulder abducted and externally rotated | Pain between 70 and 120 degrees | Ulnar collateral ligament injury |
| While maintaining a constant valgus force, the elbow is quickly flexed and extended through a complete range of motion | |||
| Tinel test | Gentle tapping over the course of a superficial nerve | Tingling, paresthesias over the distal course of the nerve | Cubital tunnel syndrome, radial tunnel syndrome |
CUBITAL TUNNEL SYNDROME
Cubital tunnel syndrome is a compressive or traction neuropathy of the ulnar nerve as it passes through the cubital tunnel of the medial elbow (Figure 3). After carpal tunnel syndrome, it is the second most common compressive neuropathy of the upper extremities.18 Approximately 60% of patients with medial epicondylitis have a concomitant compressive ulnar neuropathy.19
Patients will have medial elbow pain with repetitive activity. The pain is usually associated with numbness and tingling in the ulnar border of the forearm and hand, and in the ring and little fingers. If the condition exists for an extended period of time, weakness of the intrinsic muscles of the hand may develop.19 Patients may also have nighttime pain from sleeping with the elbow fully flexed. A physical examination of the upper extremities and cervical spine is essential to rule out other compressive neuropathies.14,20,21
A positive Tinel sign at the cubital tunnel has a specificity of 48% to 100% and a sensitivity of 44% to 75% for a compressive neuropathy12,21 (Table 23,7,8,11,13–17 ). Physical examination should focus on muscles innervated by the ulnar nerve distal to the cubital tunnel: the flexor carpi ulnaris, the flexor digitorum palmaris, the hypothenar eminence, and the intrinsic muscles of the hand. Wartenberg sign (the inability to adduct the little finger), a clawhand deformity, and flexion of the proximal interphalangeal joint and the distal interphalangeal joint of the ring and small fingers may also be present (Table 23,7,8,11,13–17 ). The ulnar nerve should be palpated in the cubital tunnel during flexion and extension to detect any subluxation or dislocation of the nerve.19
Lateral Elbow Pain
LATERAL EPICONDYLITIS (TENNIS ELBOW)
This overuse tendinopathy occurs in approximately 1% to 3% of the population annually, and although it is commonly called tennis elbow, only 5% to 10% of tennis players develop the condition. Most patients are in their 30s and 40s and develop lateral epicondylitis as a result of occupational rather than recreational activities.14 The lateral elbow is affected four to 10 times more often than the medial side.22
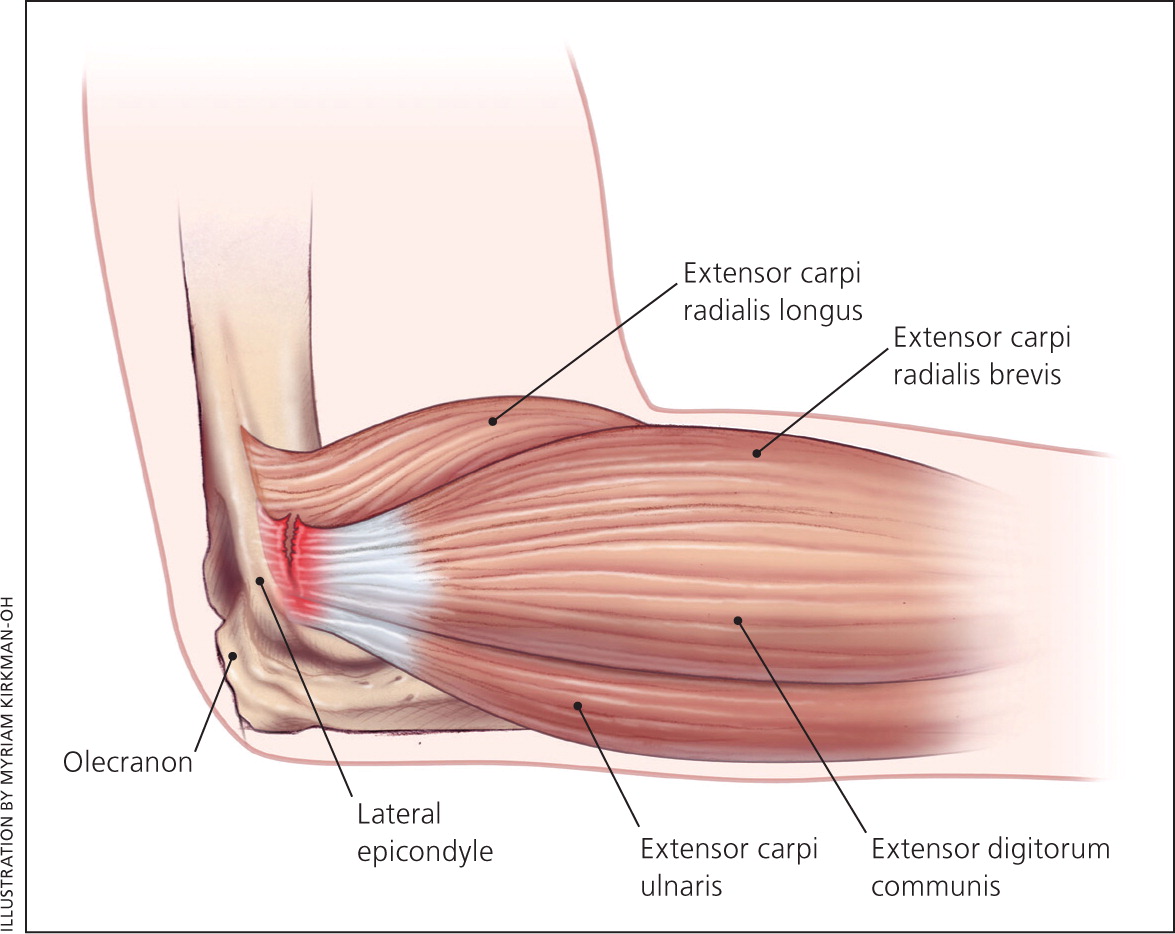
The lateral epicondyle of humerus serves as the common extensor origin for the active supinators of the forearm, including the extensor carpi radialis brevis (Figure 6). Physical examination reveals maximal tenderness approximately 1 cm distal to the epicondyle at the origin of the extensor carpi radialis brevis. Pain and decreased strength with resisted gripping and with wrist supination and extension are often present.22
RADIAL TUNNEL SYNDROME AND POSTERIOR INTEROSSEOUS NERVE SYNDROME
There is some controversy about whether radial tunnel syndrome and posterior interosseous nerve syndrome are two separate entities or a continuum of the same condition. A small percentage of patients who present with lateral elbow pain and are thought to have lateral epicondylitis on initial presentation actually have an entrapment neuropathy of the radial nerve.15,23
For both syndromes, patients typically present with a history of repetitive forearm supination and pronation (e.g., carpenters, mechanics) and have insidious, poorly localized pain in the forearm. Physical examination typically reveals a positive Tinel sign at the radial tunnel. The point of maximal tenderness usually resides over the anterior radial head. The presence of weakness with resisted supination of the forearm and extension of the middle finger (middle finger test; Figure 7) is common with posterior interosseous nerve syndrome 20 (Table 23,7,8,11,13–17 ). In contrast, radial tunnel syndrome typically presents as a pure pain syndrome without any objective clinical muscular weakness.15,19,23

OSTEOCHONDRAL DEFECT (OSTEOCHONDRITIS DISSECANS)
The articular surface most commonly injured within the elbow is the radial aspect of the joint, which can present as lateral elbow pain. Athletes in overhead throwing sports or sports that require repetitive valgus stress or compressive forces on the elbow (e.g., gymnastics) are prone to these types of injuries. Occasionally, separation of the osteochondral fragment may occur, resulting in a loose body. Symptoms may include locking, catching, or inability to fully extend the elbow.16
Posterior Elbow Pain
OLECRANON BURSITIS
Olecranon bursitis is the most common superficial bursitis and is a common cause of posterior elbow pain and swelling.24 Olecranon bursitis can be septic or aseptic. Patients with septic olecranon bursitis present with pain, swelling, warmth, and erythema over the olecranon; roughly one-half will have a fever. Diagnosis is confirmed by bursal fluid analysis.25 By contrast, patients with aseptic olecranon bursitis may present with a history of minor trauma to the elbow and a boggy, nontender mass over the olecranon without redness, warmth, limited range of motion, or other signs of infection.26 Because aspiration of bursae can be associated with complications such as introducing infection, this should be performed only when the diagnosis is uncertain or to relieve symptoms in refractory cases.24
TRICEPS TENDINOPATHY
Tendinopathy at the triceps insertion occasionally occurs in weight lifters or industrial workers in whom repetitive elbow extension against resistance is required. Diagnosis is fairly straightforward in the setting of a suggestive history. On physical examination, the patient reports pain at the posterior elbow with resisted extension, and tenderness at the triceps insertion.27
POSTERIOR IMPINGEMENT
Valgus extension overload syndrome is a condition that presents in younger athletes who are subjected to repetitive valgus stresses while in hyperextension (i.e., javelin throwers). This stress causes impingement of the olecranon tip in the olecranon fossa, which may cause osteophyte formation and a fixed flexion deformity over time. A similar condition exists in older persons with osteoarthritis. On physical examination, the patient will have posterior elbow pain when forced into full elbow extension.27
| Diagnosis | Clinical presentation | Diagnostic approach | Treatment | |
|---|---|---|---|---|
| Anterior | ||||
| Biceps tendinopathy4,28 | Vague anterior elbow pain; history of repeated elbow flexion with forearm supination and pronation | Resisted supination recreates pain deep in the antecubital fossa | Relative rest, ice, short course of NSAIDs, physical therapy | |
| Lateral | ||||
| Lateral epicondylitis (tennis elbow)14,29–32 | Much more common than medial epicondylitis; insidious onset of pain because of increase in occupational or recreational activities; tenderness to palpation over the common extensor tendon | Pain and decreased strength with resisted gripping and with wrist supination and extension; pain at the lateral elbow with isolated resisted extension of the middle finger | Relative rest and watchful waiting, ice, bracing, short course of NSAIDs | |
| Stretching and strengthening with or without formal physical therapy | ||||
| Bracing (consider wrist extension brace instead of commonly used counterforce traction brace) | ||||
| Injections of corticosteroids, autologous blood, or platelet-rich plasma; prolotherapy; dry needling | ||||
| Topical nitroglycerin | ||||
| Surgery for recalcitrant cases | ||||
| Posterior interosseous nerve syndrome15 | Painless loss of the ability to extend the middle finger against resistance | Positive result on the middle finger test (the inability to actively extend the middle finger against resistance) | Cessation of inciting activity | |
| Splinting to maintain forearm supination and wrist extension | ||||
| Physical therapy focusing on ergonomics, stretching, and then strengthening | ||||
| Surgery may be considered for refractory cases | ||||
| Radial tunnel syndrome15 | Pain in the lateral aspect of the forearm in the absence of any motor symptoms | Pain only, with no motor findings | Same treatment as for posterior interosseous nerve syndrome | |
| Medial | ||||
| Cubital tunnel syndrome33 | Insidious onset of pain and paresthesias down the medial aspect of the forearm into the ring and little fingers | Positive Tinel sign at the cubital tunnel; may feel the ulnar nerve subluxate over the medial epicondyle with flexion and extension | Conservative treatment: cessation of inciting activity, night splint to keep arm in extension, physical therapy with nerve gliding exercises | |
| Surgery for recalcitrant cases that fail to respond to four to six months of treatment | ||||
| Medial epicondylitis (golfer's elbow)17,29 | Insidious onset of pain because of increase in occupational or recreational activities; tenderness to palpation of flexor-pronator mass | Pain with resisted wrist flexion and pronation | Relative rest, ice, bracing, short course of NSAIDs (topical or oral) | |
| Stretching and strengthening with or without formal physical therapy | ||||
| Injections with corticosteroids (may be more effective than NSAIDs in the short term), autologous blood, or platelet-rich plasma; dry needling | ||||
| Topical nitroglycerin | ||||
| Surgery for recalcitrant cases | ||||
| Ulnar collateral ligament injury17 | Sensation of a pop over the medial elbow | Positive result on moving valgus stress test or milking maneuver; lack of end point with valgus stress | Rest, ice, sling, short course of NSAIDs | |
| Grade 1 and 2 partial tears should be treated with relative rest and prolonged guided rehabilitation | ||||
| Surgery should be considered early on for elite level/professional athletes | ||||
| Posterior | ||||
| Olecranon bursitis | ||||
| Aseptic24,26,34–36 | History of minor trauma to the elbow; boggy, nontender mass over the olecranon | Bursal fluid analysis; absence of redness, warmth, limited range of motion, or other signs of infection | Ice, compressive dressings, avoidance of aggravating activity | |
| For failed conservative treatment, aspiration of the bursa followed by two weeks of compressive dressing | ||||
| Surgical bursectomy may be required for refractory cases persisting longer than three months | ||||
| Intrabursal corticosteroid injection may be considered but can be complicated by infection and skin atrophy | ||||
| Septic25 | Pain, swelling, warmth, and erythema over the olecranon; approximately 50% of patients have fever | Bursal fluid analysis | Aspiration, mechanical rest, systemic oral or intravenous antibiotics directed by bursal fluid culture | |
| Posterior impingement27 | Pain at the posterior elbow, especially at full extension | Posterior elbow pain when forced into full elbow extension; radiography to evaluate for osteophyte formation | Avoidance of offending movements | |
| If conservative treatment fails, arthroscopic osteotomy of osteophytes on the posterior elbow is effective | ||||
| Triceps tendinopathy27,28 | Pain at the posterior elbow, especially with extensor use (pushing motions) | Pain at the posterior elbow with resisted extension; tenderness at the triceps insertion | Relative rest, ice, short course of NSAIDs, refer for physical therapy | |
| Surgery is rarely indicated | ||||
Imaging
Plain radiography is the initial choice for the evaluation of acute injuries and is best for showing bony injuries, soft tissue swelling, and joint effusions. Plain radiography also has a role in the evaluation of chronic conditions such as enthesopathy, bone spurs, and osteochondral diseases.18 At a minimum, anteroposterior and lateral plain radiography should be performed at the initial visit.37
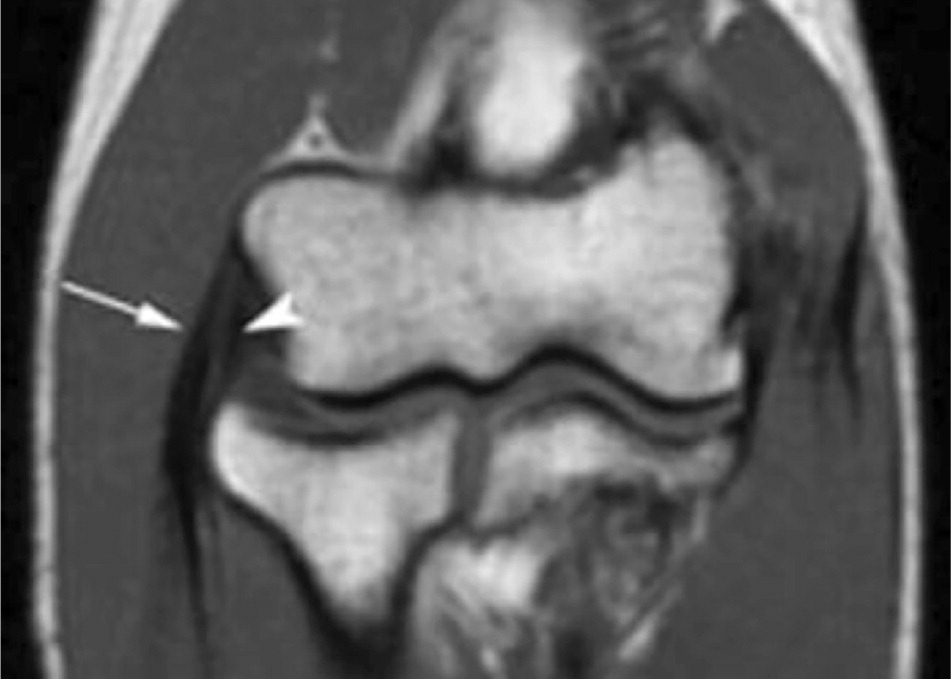
Most conditions that cause chronic elbow pathology are clinical diagnoses; imaging may be used to confirm the diagnosis before further intervention or referral. MRI is the preferred imaging modality for chronic elbow pain.37,38 MRI can identify pathologic conditions such as bone marrow edema, tendinopathy, nerve entrapments, and joint effusions. Magnetic resonance arthrography may be performed in patients without an effusion to identify ligament tears, osteochondral defects, or loose bodies18,37 (Figure 839 ).
Compared with MRI, computed tomography has a limited role in the evaluation of chronic elbow pain. It may be superior to MRI in detecting soft tissue calcification, such as myositis ossificans or intra-articular bodies.
Musculoskeletal ultrasonography is more operator-dependent than MRI but allows for an inexpensive dynamic evaluation of commonly injured structures. Ultrasonography is less expensive than MRI and, in skilled hands, has a sensitivity of 64% to 82% for the diagnosis of medial and lateral elbow tendinopathy, compared with a sensitivity of 90% to 100% with MRI.38
Electrodiagnostic studies, such as nerve conduction studies and electromyography, are helpful in confirming the diagnosis of a peripheral compressive neuropathy and ruling out conditions such as plexopathies and cervical radiculopathies. Because it takes time for the compressive or traction neuropathy to result in a positive electrodiagnostic study, false-negative results can occur if the testing is performed before symptoms have been present for six to eight weeks.12,18
Data Sources: A PubMed search was completed in Clinical Queries using the key terms elbow pain, epicondylitis, bursitis, radial tunnel, cubital tunnel, and impingement. The search included meta-analyses, randomized clinical trials, clinical trials, and reviews. Also searched were the Agency for Healthcare Research and Quality evidence reports, the Cochrane database, Essential Evidence Plus, the Institute for Clinical Systems Improvement, and the National Guideline Clearinghouse database. Search dates: January 15, 2012; June 27, 2012; and December 5, 2013.