Am Fam Physician. 2014;89(12):956-962
Author disclosure: No relevant financial affiliations.
When choosing an infiltrative anesthetic agent, the type of procedure, the length of time required for anesthesia, and the pharmacodynamics of each medication are important considerations. Distraction techniques and buffering with sodium bicarbonate can be used to decrease the pain associated with injection. Local cutaneous infiltration is the most commonly used anesthetic technique and involves direct injection into the area requiring anesthesia. Field blocks provide anesthesia by circumferentially blocking innervation to the area. Nerve blocks target the innervation to a specific area and are useful on the face and digits. Using easily identifiable landmarks, blockade of the supraorbital, supratrochlear, infraorbital, and mental nerves can provide site-specific anesthesia. Dorsal and palmar or plantar digital nerve blocks can be performed at a variety of locations on the hands and feet.
Infiltrative anesthesia is often administered in the office setting. The physician's ability to execute a variety of techniques ensures adequate pain relief while minimizing risk to the patient, leading to optimal outcomes. The standard procedure for infiltrative anesthesia is summarized in Table 1.1–3
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Lidocaine (Xylocaine) buffered with sodium bicarbonate decreases the pain associated with injection; this effect is enhanced when the solution is warmed to room temperature. | B | 28–31 |
| The intraoral approach to infraorbital or mental nerve blocks reduces patient discomfort. | C | 1, 2, 36–38 |
| Review anatomy and choose an anesthetic technique | |
| Consider contraindications | |
| Absolute contraindications: patient refusal, infection at injection site, allergy to local anesthetic, nonsterile conditions | |
| Relative contraindications: coagulopathy, preexisting neuropathy of the target nerve | |
| Discuss the procedure with the patient, including what he or she can expect and the possible complications; obtain signed informed consent as needed | |
| Evaluate the surrounding area and areas distal to the injection site for signs of neurovascular compromise | |
| Choose and label the appropriate anesthetic agent based on the technique and clinical situation; warm and buffer solutions as indicated | |
| Cleanse the injection site (for intact skin, alcohol wipes are as effective as chlorhexidine [Peridex] or povidone/ iodine) | |
| Rapidly insert the needle (27- to 30-gauge) through the skin into the subcutaneous layer, using distraction techniques as necessary; consider aspiration before injection | |
| Slowly and steadily inject small volumes of anesthetic while withdrawing the needle | |
| Test the area for adequate anesthesia | |
There are two classes of infiltrative anesthetics, amides and esters, which create a reversible blockade of sodium channels within the nerve fibers.4–6 When choosing an anesthetic agent, it is important to consider the type of procedure, the length of time required for anesthesia, and the pharmacodynamics of each medication. Table 2 is an overview of commonly used infiltrative anesthetic agents.4,6–9 True allergies to local anesthetics are rare, especially with amide preparations.10–12 However, evidence suggests there is cross reactivity between agents within the same class.13–15 In patients with a possible allergy, skin testing should be considered when immunoglobulin E–mediated reactions cannot be ruled out using the history.10,12
| Agent | Concentration | Onset* | Duration* | Maximum dose | |
|---|---|---|---|---|---|
| mg per kg | mL | ||||
| Amides | |||||
| Lidocaine (Xylocaine) | 0.5%, 1%, or 2%† | Rapid: < 2 minutes | 30 to 60 minutes | 4 (up to 300 mg per dose) | 0.5%: 60 1%: 30 2%: 15 |
| Lidocaine with epinephrine‡ | 1% or 2% | Rapid: < 2 minutes§ | 1 to 4 hours | 7 (up to 500 mg per dose) | 1%: 50 2%: 25 |
| Bupivacaine (Marcaine) | 0.25% or 0.5% | Slow: 5 minutes | 2 to 4 hours | 2 (up to 175 mg per dose) | 0.25%: 70 0.5%: 35 |
| Esters | |||||
| Procaine (Novocain) | 1% or 2% | Moderate: 2 to 5 minutes | 15 to 60 minutes | 7 (up to 600 mg per dose) | 1%: 60 2%: 30 |
| Tetracaine (Pontocaine) | 0.5% | Slow: 5 to 10 minutes | 2 to 3 hours | 1.4 (up to 120 mg per dose) | 24 |
Anesthetic Agents
Lidocaine (Xylocaine), an amide, is the most commonly used infiltrative anesthetic and is available in several concentrations.10 For most procedures, a 0.5% or 1% solution is appropriate. Higher concentrations of lidocaine do not improve onset or duration of action and may increase the risk of toxicity.1,10 Adding epinephrine (concentration of 1:100,000 or 1:200,000) prolongs the duration of anesthesia, increases the maximum dose, and may aid hemostasis.1,7,16–18 Contrary to longstanding belief, the use of lidocaine with epinephrine on the nose, ears, digits, and penis appears to be safe.19–21 However, many physicians still choose to avoid epinephrine use in these areas. Epinephrine should not be used in patients with peripheral artery disease.
Bupivacaine (Marcaine) is a widely used amide. It has a prolonged duration of action, but this also increases the risk of toxicity (4:1 risk of toxicity compared with lidocaine) and can cause a dose-dependent widening of the QRS interval, leading to ventricular fibrillation.22,23 Bupivacaine is contraindicated in pregnant women because of the increased bio-availability from decreased venous return.6,24–26 Procaine (Novocain) and tetracaine (Pontocaine) are most often used for dental, topical, spinal, and epidural anesthesia.
Pain Control
Using the smallest needle possible (27- to 30-gauge) and gently pinching or vibrating the skin adjacent to the injection site reduces the pain of injection.1,2,27 Injecting the anesthetic slowly and steadily while withdrawing the needle also minimizes pain. Injection into the subcutaneous tissue is less painful and provides equally effective anesthesia.1,2,27
Buffering lidocaine, especially solutions containing epinephrine, reduces the pain of the injection and increases patient satisfaction.28–30 Buffering is performed using sodium bicarbonate at a lidocaine-to-bicarbonate ratio of 9:1. There is a synergistic effect of pain reduction when buffering is coupled with warming the solution to room temperature.31 Bupivacaine may also be warmed and buffered to reduce pain; however, the solution has a tendency to precipitate with the rise in pH.32–34
Techniques
LOCAL CUTANEOUS INFILTRATION
Injection directly into the area needing anesthesia is adequate for minor lacerations or skin biopsies and is the most commonly used anesthetic technique. Limitations include tissue distortion, inadequate anesthesia to surrounding areas, and risk of toxicity with large amounts of anesthetic.
FIELD BLOCK
A field block should be considered for heavily contaminated wounds, for skin abscesses, and when tissue distortion should be avoided (e.g., across the vermilion border). This technique circumferentially blocks innervation to the area.2 Often, a square- or diamond-shaped field is used (Figure 1). Advantages of this technique include a longer duration of anesthesia and flexibility to accommodate the clinical situation. Limitations include an increased risk of toxicity when large amounts of anesthetic are needed and lack of effectiveness in areas with complex innervation, such as the nose.
NERVE BLOCK
A nerve block is achieved by targeting a specific nerve that supplies sensation to the desired location. It is useful on the face and digits.
Supraorbital and Supratrochlear Nerves. The forehead is innervated by the supraorbital and supratrochlear nerves, which branch off the ophthalmic portion (V1) of the trigeminal nerve. The supraorbital nerve arises from the supraorbital foramen, which can be palpated along the orbital ridge approximately 2.5 cm from the midline of the face and is in line with the pupil on forward gaze. The supratrochlear nerve is located approximately 1 cm medial to the supraorbital notch along the orbital ridge. These nerves can be blocked individually at the landmark areas, or both nerves can be blocked by infiltrating 2 to 4 mL of anesthetic along the superior border of the eyebrow.35 Complications of a forehead block include eyelid swelling, hematoma, and periorbital ecchymosis.1
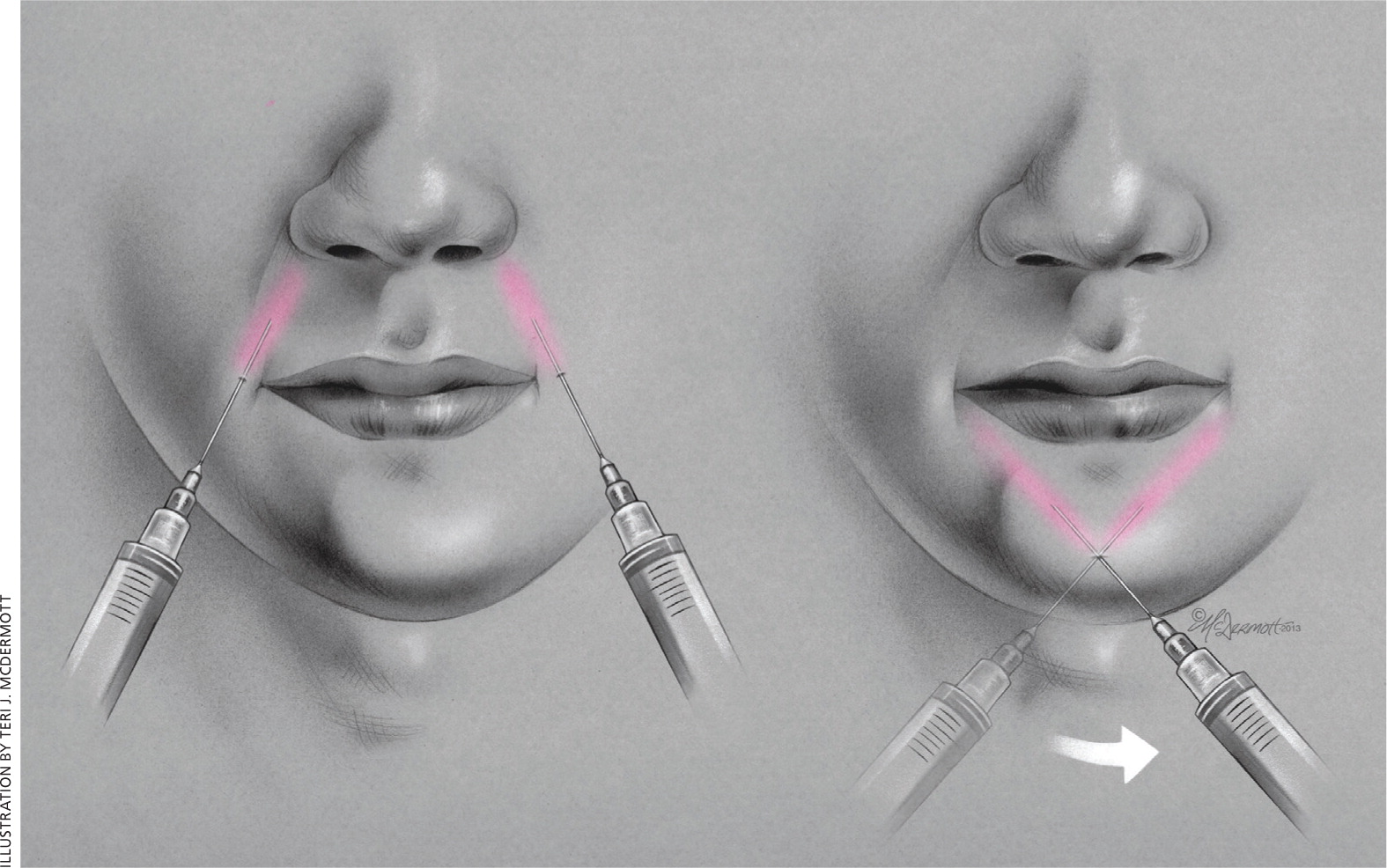
Infraorbital Nerve. The infraorbital nerve branches off of the maxillary portion (V2) of the trigeminal nerve and provides sensation from the lower eyelid to the upper lip. It penetrates the maxilla through the infraorbital foramen located just inferior to the infra-orbital ridge, also in line with the pupil on forward gaze.
There are two approaches to an infraorbital nerve block (Figure 2). The extraoral approach is performed by placing one finger on the infraorbital ridge just above the infraorbital foramen while inserting the needle superolaterally 1 cm inferior to the foramen. Aspiration is recommended to avoid the facial artery and vein.
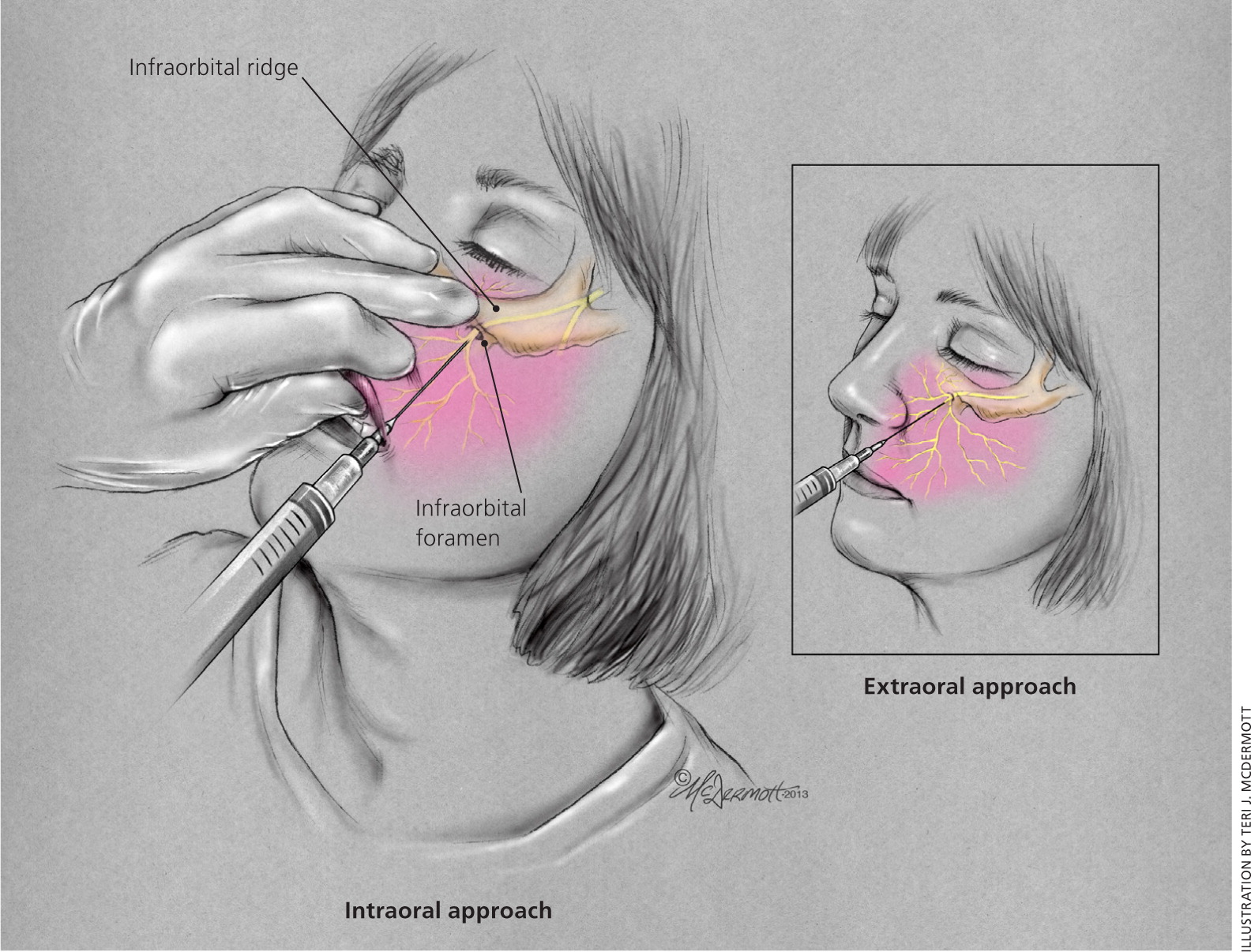
With the intraoral approach, the middle finger is placed on the inferior border of the infraorbital ridge to guide needle placement. The patient's upper lip is then grasped with the index finger and thumb, allowing for retraction of the lip and cheek. The needle is directed parallel to the long axis of the second premolar and advanced through the mucosa toward the infraorbital foramen. Aspiration should occur before injecting 1 to 3 mL of anesthetic, taking care not to advance beyond the bony orbit (approximately 2.5 cm) or into the foramen itself to avoid globe trauma or nerve damage. The intraoral technique doubles the duration of anesthesia and allows for the use of topical anesthetic on the mucosa to decrease the pain of injection.36,37
Mental Nerve. Anesthesia of the lower lip and chin can be accomplished by blocking the mental nerve. The mental nerve originates from the mandibular portion (V3) of the trigeminal nerve and emerges out of the mental foramen, which is located 1 cm inferior and slightly anterior to the second premolar. The mental nerve penetrates the mandible at a location in line with the pupil on forward gaze. The mental nerve can be reached extraorally or intraorally. Like the infraorbital nerve block, the intraoral approach can be combined with topical anesthesia.38
With the extraoral approach, the mental foramen is located by palpating along the mandible externally. The needle is inserted perpendicular to the bone and advanced to the periosteum. It is retracted 2 to 3 mm, and 2 to 4 mL of anesthetic is injected near, but not directly into, the mental foramen (Figure 3).
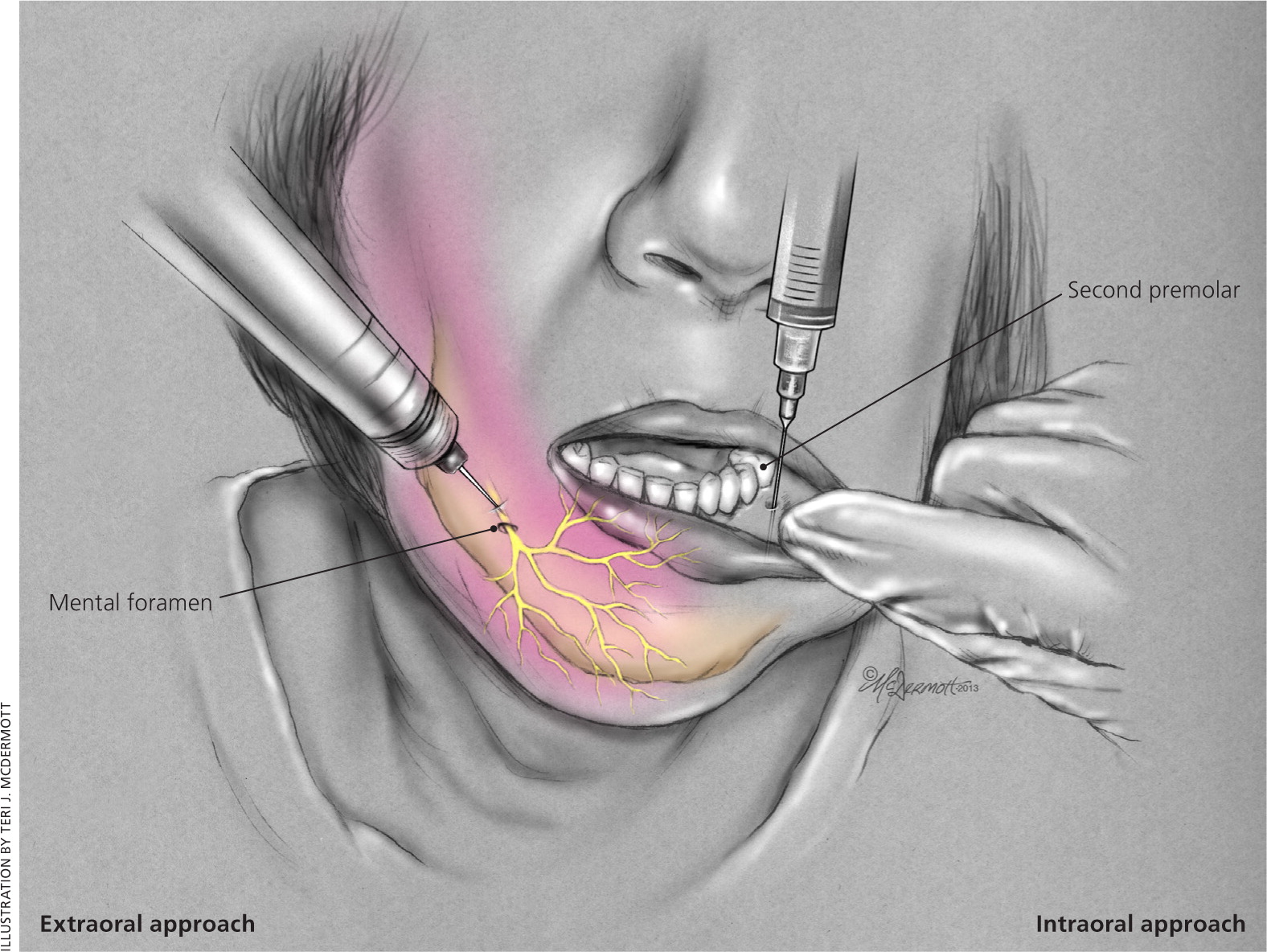
The intraoral technique is performed by pulling back the lower lip with the thumb and index finger while placing the needle at the mucosal junction of the lower lip and gum inferior to the second premolar. Then, 1 to 2 mL of anesthetic is injected near the foramen. When the operative field is near the midline, a bilateral mental nerve block should be performed to provide adequate anesthesia.
Digital Nerves. Indications for a digital nerve block include laceration repair involving the digits, reduction of fractures or dislocations, drainage of infections, and removal of nails. Although local anesthesia may be equally effective for laceration repair,39 local infiltration can be challenging because of the confined tissue space.1 The phalanges are supplied by the dorsal digital nerves at approximately the 2- and 10-o'clock positions, and by the palmar digital nerves at approximately the 4- and 8-o'clock positions. Because of the sensory distribution of these nerves (Figure 4), only the two palmar digital nerves need to be blocked in procedures involving the middle three fingers, whereas all four nerves should be blocked in procedures involving the thumb or little finger.40 The nerves can be blocked in several locations, but the most reproducible location is the web space just distal to the metacarpal or metatarsal heads.
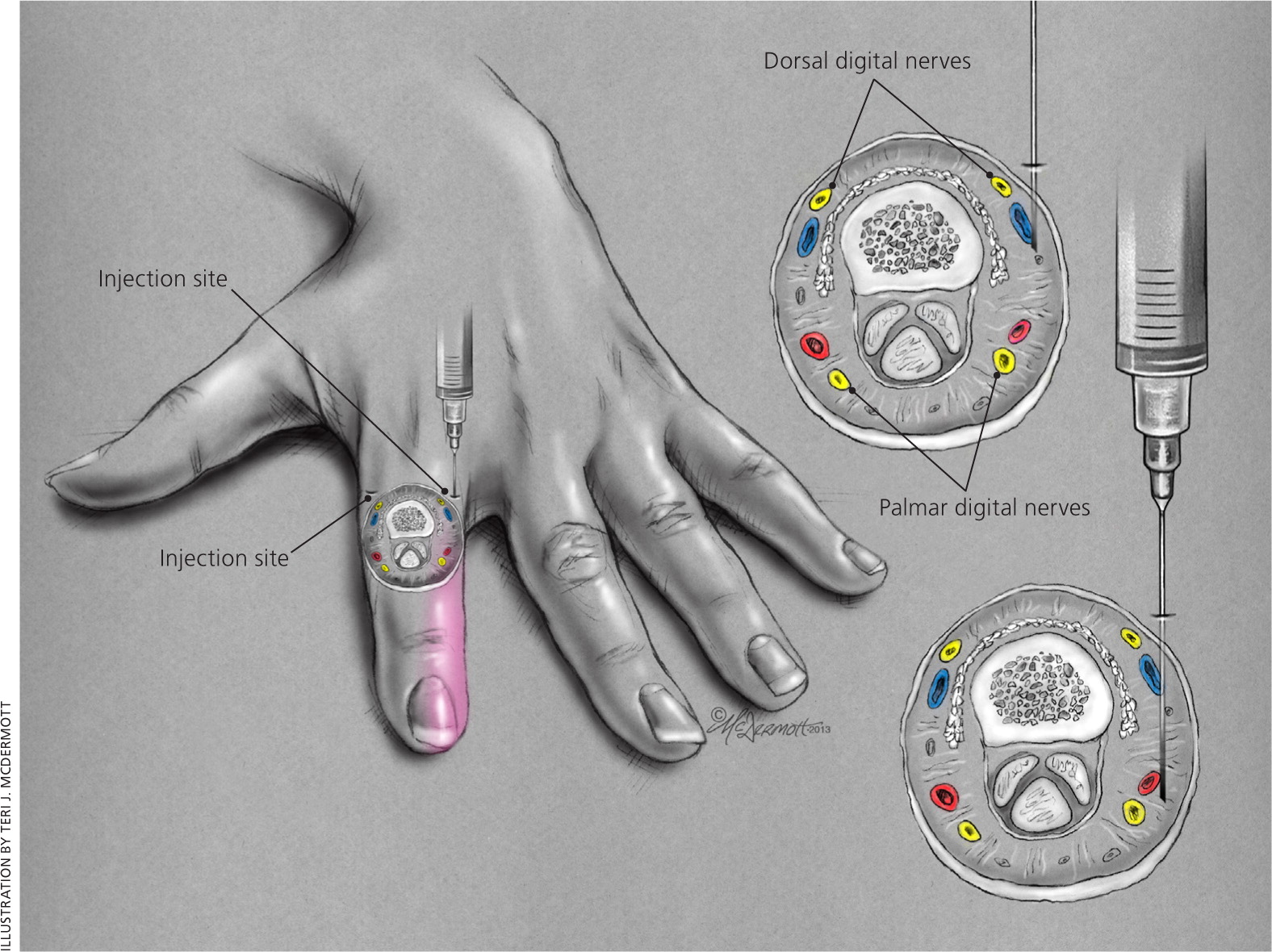
When blocking all four nerves supplying the phalanx, a dorsal approach at the level of the web space and just lateral to the proximal phalanx (Figure 4) is preferred.1 After the dermis is penetrated, 0.5 to 1 mL of lidocaine 1% is injected subcutaneously. The needle is then passed lateral to the phalanx until it begins to tent the palmar/ plantar surface. Without puncturing the palmar/ plantar skin, another 0.5 to 1 mL of anesthetic is injected. The procedure is repeated on the opposite side of the phalanx.1 Although this technique is preferred, other approaches may be used.1
When blocking the palmar digital nerves in the middle three fingers, a single site can be used, but may be more painful because it requires an injection into the palmar surface. The needle is inserted from a distal to proximal direction at a 45-degree angle to the skin directly over the metacarpal head. The needle is advanced until it makes contact with the bone. During advancement, a small amount of anesthetic can be injected. Upon contact with the bone, the needle is withdrawn slightly, then angled 4 mm medially followed by 4 mm laterally, with 0.5 mL of anesthetic injected in both locations.1
Data Sources: PubMed searches were completed using the key terms regional anesthesia, infiltrative anesthesia, local anesthetic agents, lidocaine buffering, lidocaine with epinephrine, forehead block, supraorbital nerve block, infraorbital nerve block, mental block, digital block, digital nerve block, anesthesia for phalanges, aspiration prior to injection, bupivacaine toxicity, and bupivacaine pregnancy. The search included randomized controlled trials, clinical trials, and systematic reviews. Also searched were Agency for Healthcare Research and Quality evidence reports, Clinical Evidence, the Cochrane database, Essential Evidence Plus, the Institute for Clinical Systems Improvement, the National Guideline Clearinghouse database, and DynaMed. Search dates: October and December 2011 and January 2014.