Am Fam Physician. 2014;90(2):119-120
Author disclosure: No relevant financial affiliations.
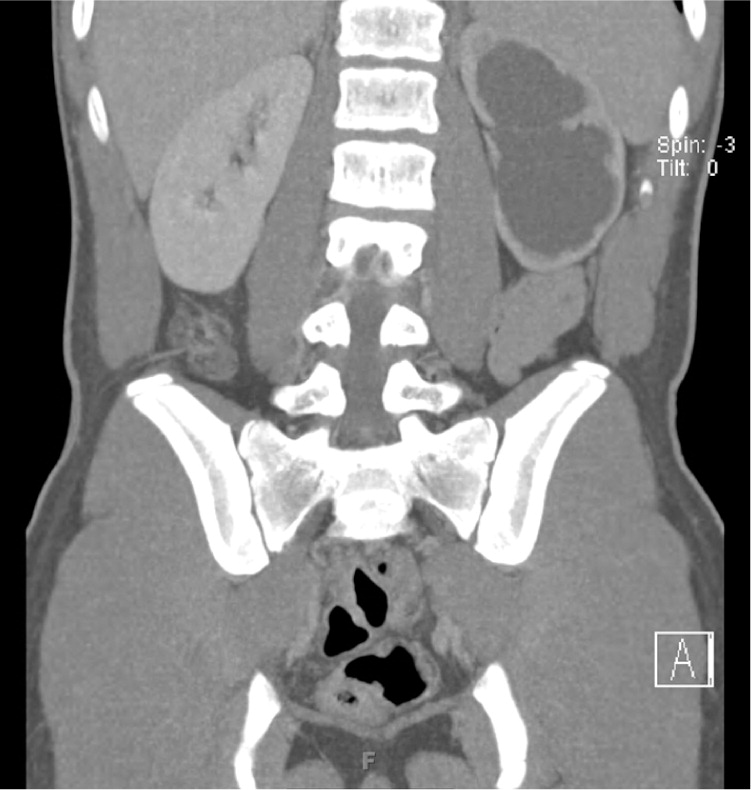
A 16-year-old boy presented to the emergency department approximately 30 minutes after he was injured during a football game. He was hit in the left flank by a helmet during a tackle. He felt short of breath and had sharp, stabbing pain on deep inspiration. He was able to speak in full sentences. He was healthy and was not taking any medications or supplements.
Physical examination revealed a heart rate of 82 beats per minute, respiratory rate of 20 breaths per minute, and a blood pressure of 130/74 mm Hg. His left flank was tender to palpation, but there was no ecchymosis or palpable abdominal mass. Urinalysis and serum creatinine findings were normal. Computed tomography was performed (Figures 1 and 2).

Question
Discussion
The answer is A: incidental finding of congenital ureteropelvic junction obstruction. The patient had a left flank contusion, and computed tomography showed isolated severe hydronephrosis with disproportionate dilatation of the renal pelvis and parenchymal thinning. Ureteropelvic junction obstruction is the most common cause of congenital hydronephrosis.1 Because this condition is often asymptomatic, late, incidental diagnosis is common. The condition causes increased kidney pressure, which results in blunting of the renal calyces and hydronephrosis. The obstruction is most often caused by intrinsic stenosis in the proximal ureter, and less commonly by extrinsic compression from a mass or aberrant renal vessel. Ureteropelvic junction obstruction is a risk factor for kidney rupture; therefore, this patient was advised to avoid contact sports until further evaluation.2
Ureterovesical junction obstruction is the second most common cause of congenital hydronephrosis.1 Obstruction occurs at the junction of the distal ureter and bladder. Imaging findings include megaureter and hydronephrosis. Secondary causes include extrinsic tumors, retroperitoneal fibrosis, and neurogenic bladder.3
Renal cell carcinoma is the most common kidney tumor in persons older than 15 years. Imaging shows a heterogeneous mass extending from normal kidney tissue. The classic presentation is the triad of flank pain, gross hematuria, and renal mass, but all three findings are present in only 19% of patients.4 Although this is a common cancer in adults, it accounts for only 2% of malignant kidney tumors in children.5
Renal papillary necrosis most often presents with hematuria. It can be painless, or pain can occur because of urinary obstruction from the sloughed cells. Analgesic nephropathy, sickle cell disease, sickle cell trait, and diabetes mellitus are risk factors.6 Computed tomography findings may include small, lobulated kidneys; blunting and clubbing of the renal calyces at the papillary tips; calcification of necrotic papillae; and sloughed papillae observed as triangular filling defects within the collecting system.
Traumatic rupture of the kidney from blunt trauma is common in high-energy collisions. Radiographic findings include evidence of tissue injury, subcapsular hematoma, contrast extravasation, and perinephric or retroperitoneal fluid collection.7 Relative to trauma to the urinary tract, renal contusion and laceration are the most common injuries reported.
| Diagnosis | Symptoms | Preferred imaging modality | Radiographic findings |
|---|---|---|---|
| Congenital ureteropelvic junction obstruction | Asymptomatic or intermittent flank pain | Ultrasonography | Hydronephrosis with tapering of dilated renal pelvis at the level of the proximal ureter |
| Congenital ureterovesical junction obstruction | Asymptomatic or intermittent flank pain | Ultrasonography | Hydronephrosis, megaureter |
| Renal cell carcinoma | Triad of flank pain, gross hematuria, and renal mass is the classic presentation | Unenhanced CT followed by three-phase CT | Enhancing renal mass |
| Renal papillary necrosis | Painful or painless hematuria | Computed tomographic urography | Small, lobulated kidneys; blunting and clubbing of renal calyces; filling defects from sloughing and calcification of papillae and contrast pooling into the site of sloughed papillae |
| Traumatic kidney rupture | Hematuria, flank pain, possible hemodynamic instability | Three-phase CT | Tissue injury, subcapsular hematoma, contrast extravasation, perinephric or retroperitoneal fluid collection |