Am Fam Physician. 2014;90(4):229-235
Patient information: See related handout on impetigo, written by the authors of this article.
Author disclosure: No relevant financial affiliations.
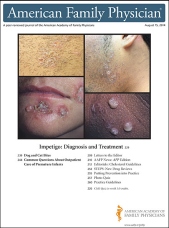
Impetigo is the most common bacterial skin infection in children two to five years of age. There are two principal types: nonbullous (70% of cases) and bullous (30% of cases). Nonbullous impetigo, or impetigo contagiosa, is caused by Staphylococcus aureus or Streptococcus pyogenes, and is characterized by honey-colored crusts on the face and extremities. Impetigo primarily affects the skin or secondarily infects insect bites, eczema, or herpetic lesions. Bullous impetigo, which is caused exclusively by S. aureus, results in large, flaccid bullae and is more likely to affect intertriginous areas. Both types usually resolve within two to three weeks without scarring, and complications are rare, with the most serious being poststreptococcal glomerulonephritis. Treatment includes topical antibiotics such as mupirocin, retapamulin, and fusidic acid. Oral antibiotic therapy can be used for impetigo with large bullae or when topical therapy is impractical. Amoxicillin/clavulanate, dicloxacillin, cephalexin, clindamycin, doxycycline, minocycline, trimethoprim/sulfamethoxazole, and macrolides are options, but penicillin is not. Natural therapies such as tea tree oil; olive, garlic, and coconut oils; and Manuka honey have been anecdotally successful, but lack sufficient evidence to recommend or dismiss them as treatment options. Treatments under development include minocycline foam and Ozenoxacin, a topical quinolone. Topical disinfectants are inferior to antibiotics and should not be used. Empiric treatment considerations have changed with the increasing prevalence of antibiotic-resistant bacteria, with methicillin-resistant S. aureus, macrolide-resistant streptococcus, and mupirocin-resistant streptococcus all documented. Fusidic acid, mupirocin, and retapamulin cover methicillin-susceptible S. aureus and streptococcal infections. Clindamycin proves helpful in suspected methicillin-resistant S. aureus infections. Trimethoprim/sulfamethoxazole covers methicillin-resistant S. aureus infection, but is inadequate for streptococcal infection.
Impetigo is a common bacterial skin infection caused by Staphylococcus aureus, group A beta-hemolytic Streptococcus pyogenes, a combination of the two, or less commonly, anaerobic bacteria.1,2 In the United States, more than 11 million skin and soft tissue infections are caused by S. aureus annually.3 Impetigo is the most common skin infection in children two to five years of age, but persons of any age can be affected.4 One-third of skin and soft tissue infections in returning travelers are attributable to impetigo, usually secondary to infected mosquito bites.5
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Topical antibiotics are more effective than placebo and preferable to oral antibiotics for limited impetigo. | A | 8, 11 |
| Oral penicillin should not be used for impetigo because it is less effective than other antibiotics. | B | 8, 12 |
| Oral erythromycin and macrolides should not be used to treat impetigo because of emerging drug resistance. | B | 8, 12 |
| There is insufficient evidence to recommend topical disinfectants for the treatment of impetigo. | B | 8 |
| There is insufficient evidence to recommend (or dismiss) popular herbal treatments for impetigo. | C | 24 |
Many bacteria inhabit healthy skin; some types, such as S. pyogenes and S. aureus, intermittently colonize the nasal, axillary, pharyngeal, or perineal areas.2,6 These bacteria can lead to infection of susceptible skin.6 Other factors that predispose to impetigo are skin trauma; hot, humid climates; poor hygiene; day care settings; crowding; malnutrition; and diabetes mellitus or other medical comorbidities.2,6 Autoinoculation via fingers, towels, or clothing often leads to the formation of satellite lesions in adjacent areas.6 The highly contagious nature of impetigo also allows spread from patients to close contacts. Although impetigo is considered a self-limited infection, antibiotic treatment is often initiated for a quicker cure and to prevent the spread to others.2 This can help decrease the number of school and work days lost.6 Hygienic practices such as cleaning minor injuries with soap and water, handwashing, regular bathing, and avoiding contact with infected children can help prevent infection.7
Clinical Presentation
There are two presentations of impetigo: nonbullous (also known as impetigo contagiosa) and bullous.
NONBULLOUS
Nonbullous impetigo is the most common presentation, comprising 70% of cases. Nonbullous impetigo can be further classified as primary or the more prevalent secondary (common) form.4,8 Primary impetigo is a direct bacterial invasion of intact healthy skin.4,8 Secondary (common) impetigo is a bacterial infection of disrupted skin caused by trauma, eczema, insect bites, scabies, or herpetic outbreaks and other diseases.6 Diabetes or other underlying systemic conditions also increase susceptibility.6 Impetigo starts as maculopapular lesions that transition into thin-walled vesicles that rapidly rupture, leaving superficial, sometimes pruritic or painful erosions covered by the classic honey-colored crusts4,8 (Figure 1). The course of infection can last two to three weeks if untreated.8 Once the crust dries, the remaining area heals without scarring. The exposed skin of the face (e.g., nares, perioral region) and the extremities are the most commonly affected sites.1 Regional lymphadenitis may occur, but systemic symptoms are unlikely.1,8 Nonbullous impetigo is usually caused by S. aureus, but S. pyogenes can also be involved, especially in warmer, more humid climates.

BULLOUS
Bullous impetigo is caused only by S. aureus1,4,9 and is characterized by large, fragile, flaccid bullae that can rupture and ooze yellow fluid (Figure 24 ). It usually resolves within two to three weeks without scarring.8 The pathognomonic collarette of scales on its periphery develops after the bullae rupture, leaving a thin, brown crust on the remaining erosions1 (Figure 3). These larger bullae form because of exfoliative toxins produced by S. aureus strains that cause loss of cell adhesion in the superficial epidermis.9 Bullous impetigo is typically found on the trunk, axilla, and extremities, and in intertriginous (diaper) areas.2 It is the most common cause of ulcerative rash on the buttocks of infants.1 Systemic symptoms are uncommon but can include fever, diarrhea, and weakness.4


Diagnosis
The diagnosis of nonbullous and bullous impetigo is nearly always clinical. Differential diagnosis includes many other blistering and rash disorders (Table 1).1,4,10 Skin swabs cannot differentiate between bacterial infection and colonization.11 In patients in whom first-line therapy fails, culture of the pus or bullous fluid, not the intact skin, may be helpful for pathogen identification and antimicrobial susceptibilities.12 Although serologic testing for streptococcal antibodies is helpful in the diagnosis of acute poststreptococcal glomerulonephritis, it does not aid in the diagnosis of impetigo.13
| Bullous |
| Bullous erythema multiforme |
| Bullous fixed drug eruption |
| Bullous lupus erythematosus |
| Bullous pemphigoid reactions |
| Bullous scabies |
| Contact dermatitis |
| Dermatitis herpetiformis |
| Insect bites |
| Linear immunoglobulin A bullous dermatosis |
| Necrotizing fasciitis |
| Pemphigus vulgaris |
| Stevens-Johnson syndrome |
| Thermal burns |
| Transient neonatal pustular melanosis |
| Nonbullous |
| Atopic dermatitis |
| Bockhart impetigo*10 |
| Childhood discoid lupus erythematosus |
| Contact dermatitis |
| Cutaneous candidiasis |
| Dermatophytosis (tinea corporis or capitis) |
| Herpes simplex virus |
| Pediculosis (lice) |
| Scabies |
| Sweet syndrome (acute febrile neutrophilic dermatosis) |
| Varicella zoster virus |
Complications
Impetigo is usually a self-limited condition, and although rare, complications can occur. These include cellulitis (nonbullous form), septicemia, osteomyelitis, septic arthritis, lymphangitis, lymphadenitis, guttate psoriasis, staphylococcal scalded skin syndrome, and acute poststreptococcal glomerulonephritis, with poststreptococcal glomerulonephritis being the most serious.14 The number of possible causes, incidence, and clinical severity of acute poststreptococcal glomerulonephritis have decreased, because the causative organism of impetigo has shifted from S. pyogenes to S. aureus.13 Most cases of poststreptococcal glomerulonephritis in the United States are associated with pharyngitis. The strains of S. pyogenes implicated in impetigo are thought to have minimal nephritogenic potential.13 There are no data to indicate that antibiotic treatment of impetigo has any effect on preventing the development of acute poststreptococcal glomerulonephritis, which can occur in up to 5% of patients with nonbullous impetigo.1,11,15,16 Rheumatic fever does not appear to be a complication of impetigo.16
Treatment
Treatment options for impetigo include topical antibiotics, systemic antibiotics, and topical disinfectants.8 Quality evidence-based research for the most effective treatment of impetigo is lacking.11 In 2012, an updated Cochrane review on impetigo interventions evaluated 68 randomized controlled trials, including 26 on oral treatments and 24 on topical treatments. There was no clear evidence as to which intervention is most effective.8 Topical antibiotics are more effective than placebo and preferable to oral antibiotics for limited impetigo.8,11 Systemic antibiotics are often reserved for more generalized or severe infections in which topical therapy is not practical. Clinicians sometimes may choose both topical and systemic therapy.8 The ideal treatment should be effective, be inexpensive, have limited adverse effects, and should not promote bacterial resistance.2,4,8
TOPICAL ANTIBIOTICS
Topical antibiotics (Table 26,8,11,14,17–19 ) have the advantage of being applied only where needed, minimizing antibiotic resistance and avoiding gastrointestinal and other systemic adverse effects.4,8 The length of time of topical treatment varies based on product, but in clinical trials, a seven-day course was more effective than placebo for resolution of impetigo.8,11 Local allergic reactions, skin sensitization, and difficulty with application to areas such as eyelids, mouth, and back are potential disadvantages of topical treatments. Three topical antibiotic preparations recommended for impetigo are mupirocin 2% cream or ointment (Bactroban), retapamulin 1% ointment (Altabax), and fusidic acid (not available in United States). Empiric treatment considerations have changed with the increasing prevalence of antibiotic-resistant bacteria. Methicillin-resistant S. aureus (MRSA), macrolide-resistant streptococcus, and mupirocin-resistant streptococcus are now documented.6,14
| Medication | Instructions | Cost* |
|---|---|---|
| Fusidic acid 2% ointment†17 |
|
|
| Mupirocin 2% cream (Bactroban)‡8,18 |
|
|
| Mupirocin 2% ointment‡11 |
|
|
| Retapamulin 1% ointment (Altabax)§19 |
|
|
Retapamulin is a novel pleuromutilin antibacterial and the first new topical antibacterial in nearly 20 years.14 Pleuromutilins, derived from the fungus Clitopilus passeckerianus, have antibacterial activity against gram-positive bacterial organisms.20 Retapamulin acts on three key aspects of bacterial protein synthesis, making it far less likely to induce resistant strains. In 2007, the U.S. Food and Drug Administration approved retapamulin 1% ointment for the treatment of impetigo due to S. aureus (methicillin-susceptible isolates only) or S. pyogenes in adults and children at least nine months of age. Retapamulin is not approved for intranasal staphylococcal carrier treatment or treatment of MRSA-related skin infections.6,19 Pricing of the two topical treatment options available in the United States varies depending on preparation. Mupirocin is available as a less expensive generic version and as a brand. All available mupirocin products are less expensive than the newer brand-only retapamulin ointment (Table 26,8,11,14,17–19 ).
ORAL ANTIBIOTICS
Oral antibiotic therapy can be used for impetigo with large bullae or when topical therapy is impractical (Table 3).12,15 Treatment for seven days is usually sufficient, but this can be extended if the clinical response is inadequate and antibacterial susceptibility has been confirmed. There is no clear evidence-based preference among the different classes of oral antibiotics. Comparison studies also show no significant difference in cure rates between topical and oral antibiotics.8 In the past, erythromycin and penicillin were standard treatments, but because of emerging drug resistance, they are no longer routinely used.12 Resistance rates vary regionally, so health care professionals should check local resistance patterns to select the appropriate antibiotic.8 One study that lacked statistical power showed oral penicillin V potassium was no more effective than placebo.4,11 In other studies, penicillin V potassium was inferior to erythromycin and cloxacillin (no longer available in the United States), whereas topical mupirocin was slightly superior to oral erythromycin. No macrolide was found to be better than another, but all were found superior to penicillin V potassium; however, because of increasing macrolide resistance, they are no longer a preferred option. Amoxicillin/clavulanate (Augmentin) was superior to amoxicillin alone because of its coverage of β-lactamase–producing organisms. Although cephalosporins may be used, there is no evidence that one generation is better than another.8
| Drug | Adult seven-day dose | Cost (for a typical course of treatment)* | Children seven-day dose | Cost* |
|---|---|---|---|---|
| Amoxicillin/clavulanate (Augmentin)† | 875/125 mg every 12 hours | $19 ($193) |
| 1 bottle, 400/57 mg per 5 mL (100-mL oral suspension): $30 ($125) |
| Cephalexin (Keflex) | 250 mg every six hours or 500 mg every 12 hours | $5 ($90) |
| 1 bottle, 250 mg per 5 mL (100-mL oral suspension): $14 (NA) |
| Clindamycin‡ | 300 to 600 mg every six to eight hours | $18 ($200) |
| 1 bottle, 75 mg per 5 mL (100-mL oral solution): $47 (pricing varies by region) |
| Dicloxacillin | 250 mg every six hours | $14 (NA) |
| See adult pricing: no liquid formulation available |
| Doxycycline§ | 50 to 100 mg every 12 hours | $15 ($95) |
| 1 bottle, 25 mg per 5 mL (60-mL oral suspension): $20 (pricing varies by region) |
| Minocycline (Minocin)§ | 100 mg every 12 hours | $36 ($185) |
| See adult pricing: no liquid formulation available |
| Trimethoprim/sulfamethoxazole§ | 160/800 mg every 12 hours | $4 (NA) |
| 1 bottle, 40/200 mg per 5 mL (100-mL oral suspension): $4 (pricing varies by region) |
The incidence of MRSA-related skin and soft tissue infections was increasing, but more recent studies show it may be declining.21 No studies have specifically identified a problem with MRSA-related impetigo in adults or children, but cultures may still be useful in some settings.6,12 If MRSA infection is suspected, initial treatment with trimethoprim/sulfamethoxazole, clindamycin, or a tetracycline (doxycycline or minocycline [Minocin]) is recommended pending culture results.6 Although trimethoprim/sulfamethoxazole is effective for S. aureus infection, including most MRSA infections, its use for impetigo is limited by inadequate coverage of streptococcal bacteria. Oral clindamycin penetrates skin and skin structures and should be considered if MRSA infection is suspected. Because of an increasing risk of pseudomembranous colitis, clindamycin should be reserved for patients allergic to penicillin, or for infections that fail to respond to other treatments. Tetracyclines can be used for susceptible MRSA infections, but should be avoided in children younger than eight years.12 Oral fluoroquinolones are not preferred because of low staphylococcal activity and their potential association with tendinopathy and arthropathies.12
TOPICAL DISINFECTANTS
There are some studies on the benefits of nonantibiotic treatments, such as disinfectant soaps, but they lack statistical power.11 Disinfectants appear to be less effective than topical antibiotics and are not recommended.8 Studies comparing hexachlorophene (not available in the United States) with bacitracin and hydrogen peroxide with topical fusidic acid found the topical antibiotic to be more effective.8,22,23
NATURAL THERAPIES
The evidence is insufficient to recommend or dismiss popular herbal treatments for impetigo.24 Natural remedies such as tea tree oil; tea effusions; olive, garlic, and coconut oils; and Manuka honey have been anecdotally successful. The fact that impetigo is self-limited means that many “cures” could appear to be helpful without being superior to placebo. In one study, tea leaf ointment and oral cephalexin (Keflex) were similarly effective, with a cure rate of 81% vs. 79%.25 Tea tree oil (derived from Melaleuca alternifolia) appeared to be equivalent to mupirocin 2% for topical decolonization of MRSA.26
Future Treatments
Future treatments for impetigo might include minocycline foam (Foamix), which has successfully completed phase II trials, and Ozenoxacin, a topical quinolone that has successfully completed phase III clinical trials.27,28 Few controlled clinical trials have had their results published and most are methodologically weak. This area seems to merit further study through rigorous clinical trials.
Data Sources: A PubMed search was conducted for impetigo-related topics, including clinical reviews, randomized controlled trials, and meta-analyses. Search terms included impetigo; impetigo and treatment; retapamulin; fusidic acid; impetigo and MRSA; natural and herbal treatments for impetigo; minocycline foam (Foamix); Ozenoxacin; antibiotic resistance and impetigo; and topical and systemic treatments for impetigo. Relevant publications from the Cochrane Database of Systematic Reviews, Essential Evidence, UpToDate, Epocrates, and the Centers for Disease Control and Prevention website were also reviewed. Search dates: April to December 2012, and May 2014.