
Am Fam Physician. 2014;90(10):717-724
Patient information: See related handout on car safety during pregnancy, written by the authors of this article.
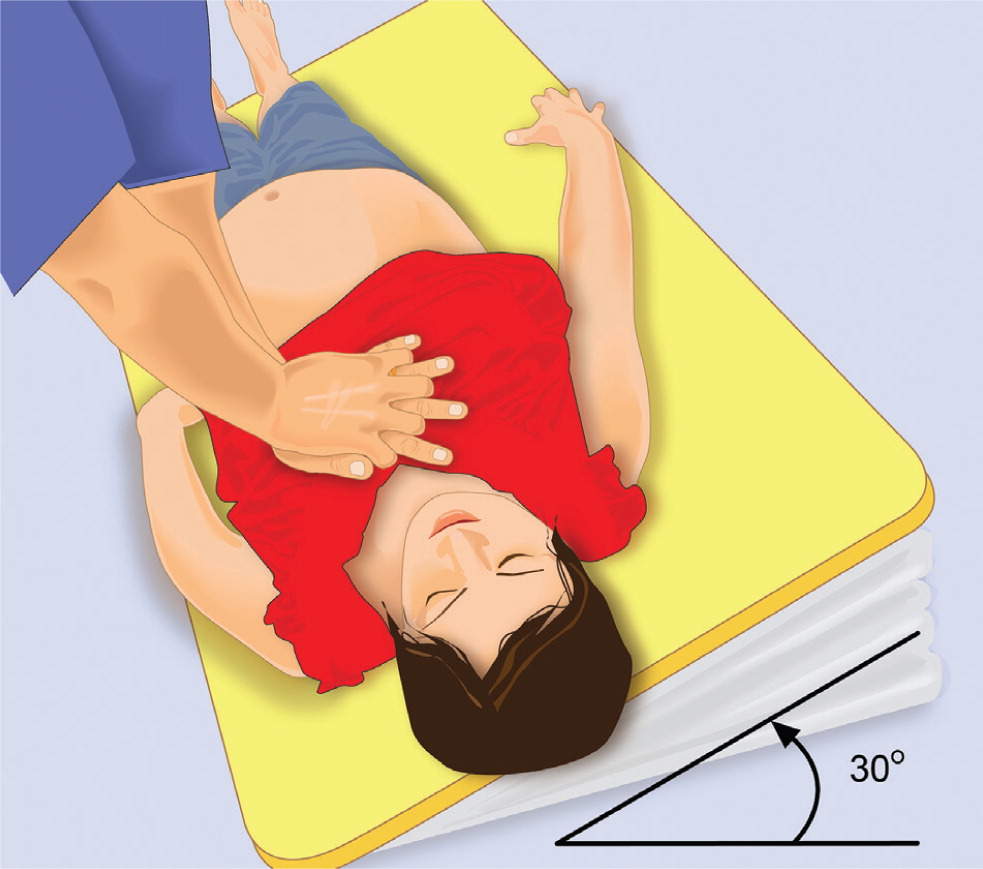
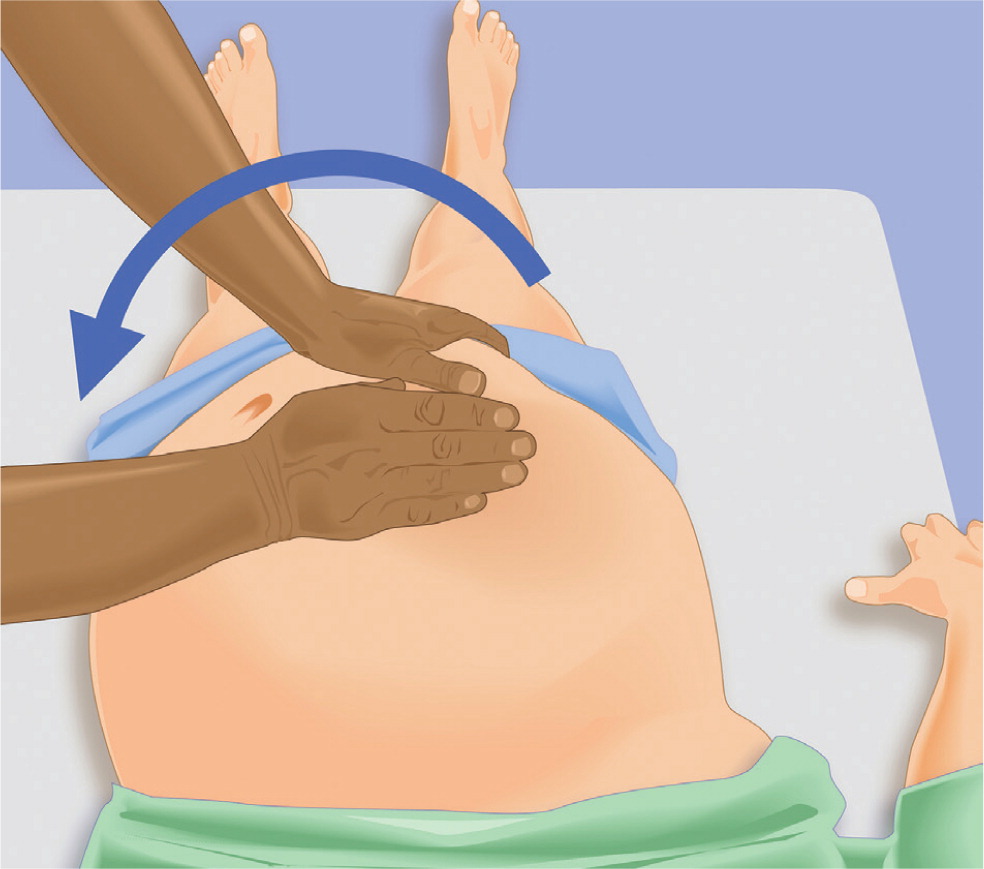
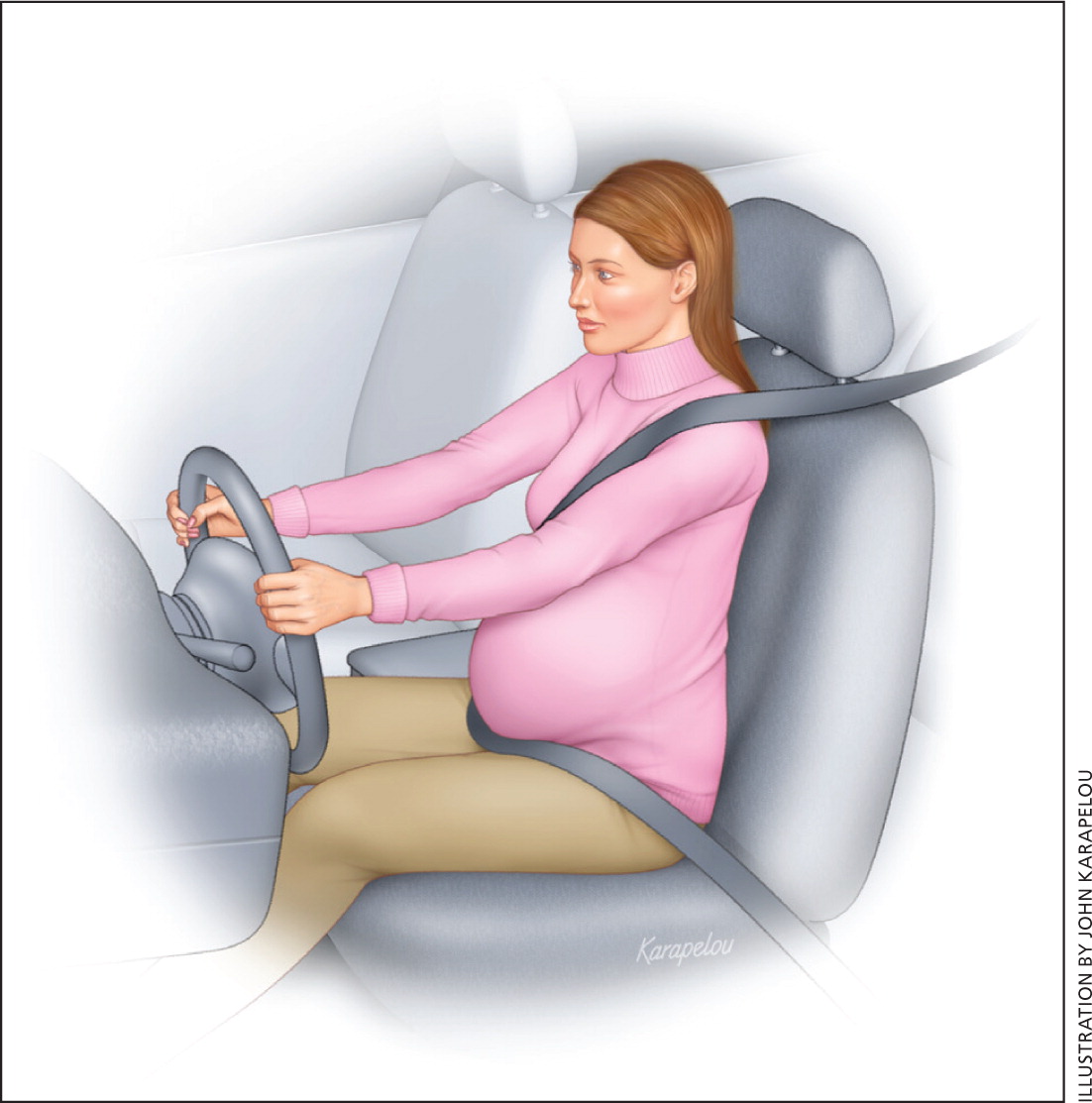
Trauma complicates one in 12 pregnancies, and is the leading nonobstetric cause of death among pregnant women. The most common traumatic injuries are motor vehicle crashes, assaults, falls, and intimate partner violence. Nine out of 10 traumatic injuries during pregnancy are classified as minor, yet 60% to 70% of fetal losses after trauma are a result of minor injuries. In minor trauma, four to 24 hours of tocodynamometric monitoring is recommended. Ultrasonography has low sensitivity, but high specificity, for placental abruption. The Kleihauer-Betke test should be performed after major trauma to determine the degree of fetomaternal hemorrhage, regardless of Rh status. To improve the effectiveness of cardiopulmonary resuscitation, clinicians should perform left lateral uterine displacement by tilting the whole maternal body 25 to 30 degrees. Unique aspects of advanced cardiac life support include early intubation, removal of all uterine and fetal monitors, and performance of perimortem cesarean delivery. Proper seat belt use reduces the risk of maternal and fetal injuries in motor vehicle crashes. The lap belt should be placed as low as possible under the protuberant portion of the abdomen and the shoulder belt positioned off to the side of the uterus, between the breasts and over the midportion of the clavicle. All women of childbearing age should be routinely screened for intimate partner violence.
Family physicians, regardless of their involvement in intrapartum care, often evaluate pregnant women after minor accidents, falls, or motor vehicle crashes. Trauma complicates one in 12 pregnancies, and is the leading nonobstetric cause of death among pregnant women.1–3 Traumatic injuries to pregnant women are unintentional (motor vehicle crashes [48%], falls [25%], poisonings, and burns) or intentional (assaults/intimate partner violence [IPV; 17%], suicide [3.3%], homicide, and gunshot wounds [4%]).2,4 Injuries are classified as minor or major trauma. By convention, minor trauma does not involve the abdomen, rapid compression, deceleration, or shearing forces, and the patient does not report pain, vaginal bleeding, loss of fluid, or decreased fetal movement.5 Nine out of 10 traumatic injuries during pregnancy are classified as minor. However, of fetal losses associated with trauma, 60% to 70% follow minor injuries.4
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Pregnant women at greater than 20 weeks' gestation who have experienced trauma should be monitored for a minimum of four hours by tocodynamometry. | C | 8, 12 |
| The Kleihauer-Betke test should be performed in all pregnant women who sustain major trauma. | C | 8, 12 |
| Perimortem cesarean delivery after cardiac arrest may improve neonatal and maternal outcomes, and is not harmful. | C | 16, 19, 20, 22 |
| Pregnant women who are occupants in motor vehicles should wear lap and shoulder seat belts, and should not turn off air bags. | C | 28, 29 |
| All women of childbearing age should be screened for intimate partner violence. | B | 31, 33 |
Anatomic and physiologic changes of pregnancy influence the assessment, management, and prevention of trauma.3,6 Physiologic changes include a 30% to 50% increase in blood volume and a 40% to 50% increase in respiratory rate.7 Anatomic changes include elevated diaphragm, delayed gastric emptying, and progressive uterine growth. During the first trimester, the thick-walled uterus is well protected from trauma by the pelvic girdle. In the second trimester, relatively abundant amniotic fluid volume protects the fetus. By the third trimester, however, the now thin-walled and prominent uterus is exposed to blunt and penetrating abdominal trauma. The placenta is an inelastic organ attached to an elastic organ (the uterus). Placental abruption may occur when trauma involving acceleration and deceleration deforms the uterus and shears the placenta off its implantation site.
Assessment
The most common pregnancy-related traumas are minor incidents, including motor vehicle crashes and mild blunt abdominal trauma. These situations require clinical judgment about the extent of maternal and fetal assessment. However, because insignificant trauma can result in fetal injury or demise, fetal monitoring recommendations for pregnant women with minor trauma are similar to those for women with major trauma.8–10 In patients who have experienced IPV, an assessment for depression and suicidality should accompany assessment for immediate safety.11
In major trauma, the primary assessment should focus on airway, breathing, and circulation. Once the primary assessment has been completed, a secondary assessment should include obstetric and nonobstetric injuries and fetal well-being.
A placental abruption may become apparent shortly after the injury. Fetal monitoring in women who experience trauma at greater than 20 weeks' gestation should be initiated as soon as the patient is stabilized. The patient should be monitored by tocodynamometry for a minimum of four hours.8,12 Eight or more contractions per hour were present in the first four hours of monitoring in 100% of patients with an ultimate diagnosis of placental abruption.8,9 If at least six contractions per hour are detected during the four-hour initial period, or the mechanism of injury presents a high degree of fetal risk,13 then 24 hours of monitoring is indicated.3,12 Before viability (23 to 24 weeks' gestation), the fetal heart should be monitored via intermittent Doppler auscultation, and after viability, continuous fetal monitoring should be performed.
Ultrasonography has poor sensitivity (24%) for detection of placental abruption. However, it is very specific (96%), resulting in a positive predictive value of 88% if abruption is seen and a negative predictive value of 53% if abruption is not seen.14
The Kleihauer-Betke test allows identification of fetal blood cells. It should be performed in pregnant women who sustain major trauma to detect fetomaternal transfusion, regardless of Rh status, to determine the degree of fetomaternal hemorrhage.8 Although the Kleihauer-Betke test screens for the degree of trauma in all patients, the result is used only to dictate Rh immune globulin therapy in Rh-negative patients.
Management
MINOR TRAUMA
Management of minor trauma is limited to care of lacerations or fractures, discussion of appropriate analgesics, counseling about the signs and symptoms of abruption, and ensuring appropriate follow-up. Tetanus toxoid should be administered if tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis (Tdap) vaccine has not already been administered during the current pregnancy. Appropriate referrals should be made to community-based advocacy groups for persons who have experienced IPV, and a plan should be made to ensure the safety of the patient and other vulnerable persons living in the household.11
MAJOR TRAUMA
When feasible, patients who have experienced major trauma should be transported to a hospital that has the resources to perform a timely trauma evaluation.3 Because placental abruption has been reported to occur up to 24 hours following trauma, monitoring via tocodynamometry should be continued for a minimum of 24 hours if at least six uterine contractions have occurred or if there are nonreassuring fetal heart rate patterns, vaginal bleeding, significant uterine tenderness, serious maternal injury, or a positive Kleihauer-Betke test result.3,13 If none of these findings are present, the patient may be discharged home with precautions.3 Table 1 provides evaluation and discharge criteria for blunt trauma in pregnancy.9,12
| Evaluation |
| Primary maternal and fetal survey |
| Laboratory: blood type, Rh factor test, hematocrit measurement, Kleihauer-Betke test, coagulation studies |
| Consider obstetric ultrasonography |
| If greater than 20 weeks' gestation, monitor for contractions |
| If fewer than three contractions per hour, monitor for four hours, then discharge |
| If three to seven contractions per hour, monitor for 24 hours, then discharge |
| Discharge criteria |
| Resolution of contractions |
| Reassuring fetal heart tracing |
| Intact membranes |
| No vaginal bleeding |
| No uterine tenderness |
| All Rh-negative patients should receive Rh immune globulin therapy unless the injury is remote from the uterus (e.g., isolated distal extremity)12 |
Between 24 and 34 weeks' gestation, if delivery appears imminent, 12 mg of betamethasone should be administered intramuscularly to promote fetal lung maturity, and repeated in 24 hours. All pregnant Rh-negative patients should receive Rh immune globulin therapy unless the injury is remote from the uterus (e.g., isolated distal extremity).12
CARDIOPULMONARY RESUSCITATION
Because of maternal physiologic changes, left lateral uterine displacement is required during cardiopulmonary resuscitation. This is performed by tilting the whole maternal body 25 to 30 degrees (Figure 215 ), or by manual uterine displacement (Figure 315 ). Manual uterine displacement may allow for more effective chest compressions because it avoids the need to facilitate a total body tilt.16 All standard medications and defibrillation regimens may be used in advanced cardiac life support (ACLS).17 Unique aspects of ACLS include early intubation, removal of all uterine and fetal monitors, and performance of a perimortem cesarean delivery.18 Modifications of resuscitative efforts in pregnancy are listed in eTable A.
| Action | Rationale |
|---|---|
| Basic life support | |
| Perform manual uterine displacement, or 25- to 30-degree left lateral tilt | Decreased aortocaval compression |
| Increase chest wall compression force | Decreased chest wall compliance with breast hypertrophy and diaphragmatic elevation |
| Use cricoid pressure, if assistance is available | Decreased gastric aspiration |
| Perform compressions higher on the sternum (slightly above center of sternum) | Elevated diaphragm and contents |
| Remove fetal and uterine monitors before defibrillation | Loss of adequate cardiac shock dose; produces skin burns at monitor sites |
| Heimlich maneuver; use chest thrust if unable to encircle the gravid abdomen | Enlarged uterus displaces diaphragm |
| Advanced cardiac life support | |
| Start intravenous therapy above diaphragm | Aortocaval compression |
| Early tracheal intubation; use short laryngoscope handle and smaller endotracheal tube | Difficult ventilation with pharyngeal edema, breast hypertrophy, diaphragmatic elevation |
| Consider other etiologies (e.g., magnesium toxicity) | Magnesium used as tocolytic therapy |
| Consider left wide paddle, adhesive pad, or breast displacement | Dextrorotation of the heart; breast hypertrophy |
| Verify endotracheal tube with carbon dioxide detector | Esophageal detector more likely not to reinflate after compression |
| Alter ventilation volumes and rates | Tailor ventilator support to oxygenation and ventilation |
| Perform emergency hysterotomy after four minutes | Decreased aortocaval and venous compression |
| Continue all maternal resuscitative efforts (cardiopulmonary resuscitation, positioning, defibrillation, and drugs) during and after cesarean delivery | Decreased aortocaval and venous compression |
PERIMORTEM CESAREAN DELIVERY
Perimortem cesarean delivery may save the life of the fetus when performed after 23 to 24 weeks' gestation.19,20 Delivery increases venous return and cardiac output by 25% to 30%, may lead to a clear survival benefit for the mother, and has not been shown to be harmful.16,19–22 The American Heart Association recommends considering perimortem cesarean delivery if ACLS has not returned spontaneous circulation within four to five minutes of cardiac arrest.18 Table 2 and eTable B describe considerations based on gestational age and issues related to perimortem cesarean delivery.
| Gestational age less than 20 weeks: emergency hysterotomy is not indicated for a single fetus, but it may be indicated for more than one fetus. |
| Gestational age 20 to 23 weeks: emergency hysterotomy is indicated to enable successful resuscitation but not for survival of the delivered fetus. |
| Gestational age greater than 23 weeks: emergency hysterotomy is indicated to save the life of both the mother and fetus. |
| Emergency hysterotomy should not be delayed while attempting to listen for fetal heart tones or to perform an ultrasonography to document gestational age. A uterine fundus measurement of 3 to 4 cm above the umbilicus correlates with a 23- to 24-week singleton gestation, and is a quick, easy assessment of gestational age that can be made in the field. Omission of an emergency hysterotomy, or delay in performing the procedure, may lead to the unnecessary loss of two lives, although the decision is multidimensional. |
| Personnel with the appropriate skills and equipment should provide this service, in or out of the hospital. |
| Factors to consider | Discussion | |
|---|---|---|
| Cardiac arrest | ||
|
| |
| Mother-infant factors | ||
|
| |
| Setting and personnel | ||
|
| |
| Differential diagnosis | ||
|
| |
Prevention
MOTOR VEHICLE CRASHES
Seat belt use actually decreases during pregnancy, because women fear that the seat belt will hurt the fetus. In blunt trauma, the most common cause of fetal death is maternal death.9 Incorrect seat belt use increases the risk of intrauterine injury and fetal death.25 When women were properly restrained, adverse fetal outcomes occurred in 29% of motor vehicle crashes. In women who were improperly restrained, adverse fetal outcomes occurred in 50% of motor vehicle crashes.26 Proper seat belt use should be a major prenatal counseling issue. The lap belt should be placed as low as possible under the protuberant portion of the abdomen and the shoulder belt positioned off to the side of the uterus, between the breasts and over the midportion of the clavicle (Figure 4). Placement of the lap belt over the dome of the uterus significantly increases pressure transmission to the uterus and has been associated with significant uterine and fetal injury. There should not be excessive slack in either belt, and both the lap and shoulder restraints should be applied as snugly as comfort will allow.
Air bag deployment reduces injury to pregnant women and does not increase the risk of adverse pregnancy outcomes.27 The American College of Obstetricians and Gynecologists (ACOG)28 and the National Highway Traffic Safety Administration29 state that pregnant women who are occupants in motor vehicles should wear lap and shoulder seat belts and should not turn off air bags.
INTIMATE PARTNER VIOLENCE
Direct assault on the abdomen may occur in the setting of IPV. As a result, ACOG and the American Academy of Pediatrics recommend universal screening for IPV during pregnancy.30,31 Likewise, the American Academy of Family Physicians states that all family physicians should be alert for physical and behavioral signs and symptoms associated with abuse or neglect.32 The U.S. Preventive Services Task Force recommends that all women of childbearing age be screened for IPV.33 A review of this topic was previously published in the May 15, 2011, issue of American Family Physician (https://www.aafp.org/afp/2011/0515/p1165.html).
A patient who presents with a vague or inconsistent history of trauma should raise suspicion for battering.12 Battering may escalate in pregnancy. The abdomen is the most common target for blows, kicks, and other assaults. Table 3 lists other historical elements and signs that may indicate IPV.12,30 Identified patients should be appropriately counseled and referred.30
| Diminished self-image, depression, or suicide attempts |
| Frequent emergency department or physician's office visits |
| Injuries inconsistent with the stated history |
| Partner insists on being present for interview and examination, and monopolizes discussion |
| Progressive isolation from support systems |
| Reproductive coercion |
| Self-abuse |
| Self-blame for injuries |
| Symptoms suggestive of substance abuse |
| Unwanted touching or fondling |
Data Sources: Drawing on the literature search completed in October 2013 for the American Academy of Family Physicians' Advanced Life Support in Obstetrics Chapter K: Maternal Resuscitation, we searched the Cochrane Database of Systematic Reviews, the National Guideline Clearinghouse, and PubMed utilizing the key words trauma, motor vehicle crashes, pregnancy, abruption, and perimortem cesarean delivery, both individually and in combination. Search date: August 14, 2014.
The opinions and assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the U.S. Army, Navy, or Air Force Medical Departments or the U.S. Army, Navy, Air Force, or Public Health Service.
This article is one in a series on “Advanced Life Support in Obstetrics (ALSO),” initially established by Mark Deutchman, MD, Denver, Colo. The series is now coordinated by Larry Leeman, MD, MPH, ALSO Managing Editor, Albuquerque, N.M.
