
Am Fam Physician. 2015;91(7):452-459
See related content: Evaluation of Acute Abdominal Pain in Adults.
Author disclosure: No relevant financial affiliations.
Acute abdominal pain is a common presentation in the outpatient setting and can represent conditions ranging from benign to life-threatening. If the patient history, physical examination, and laboratory testing do not identify an underlying cause of pain and if serious pathology remains a clinical concern, diagnostic imaging is indicated. The American College of Radiology has developed clinical guidelines, the Appropriateness Criteria, based on the location of abdominal pain to help physicians choose the most appropriate imaging study. Ultrasonography is the initial imaging test of choice for patients presenting with right upper quadrant pain. Computed tomography (CT) is recommended for evaluating right or left lower quadrant pain. Conventional radiography has limited diagnostic value in the assessment of most patients with abdominal pain. The widespread use of CT raises concerns about patient exposure to ionizing radiation. Strategies to reduce exposure are currently being studied, such as using ultrasonography as an initial study for suspected appendicitis before obtaining CT and using low-dose CT rather than standard-dose CT. Magnetic resonance imaging is another emerging technique for the evaluation of abdominal pain that avoids ionizing radiation.
Abdominal pain is a common presentation in the ambulatory setting, accounting for 1.5% of all office-based visits and 8% of all emergency department visits in the United States in 2010.1 Acute abdominal pain has many potential underlying causes, ranging from benign, self-limited conditions to life-threatening surgical emergencies. Although the patient history, physical examination, and laboratory test results can narrow the differential diagnosis, imaging is often required for definitive diagnosis and treatment.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Ultrasonography is the initial imaging study of choice for evaluating patients with acute right upper quadrant pain. | C | 6 |
| Computed tomography is the initial imaging study of choice for evaluating patients with acute right lower quadrant or left lower quadrant pain. | C | 5, 8 |
| Conventional radiography has limited diagnostic value in the assessment of patients with acute abdominal pain. | C | 21 |
| Beta human chorionic gonadotropin testing should be considered before performing diagnostic imaging in all women of reproductive age presenting with acute abdominal pain. | C | 9 |
The differential diagnosis for abdominal pain is broad, encompassing gastrointestinal, gynecologic, urologic, vascular, and musculoskeletal conditions. An approach to narrowing the differential diagnosis based on history, physical examination, and laboratory testing, in addition to imaging, is outlined in our previous article on this topic.2 If a likely diagnosis is apparent based on the clinical presentation, imaging may or may not be indicated (Table 13–12 ).
| Likely clinical diagnosis | Imaging recommendation | Comments |
|---|---|---|
| Abscess | CT of abdomen and pelvis with contrast media3 | — |
| Acute pancreatitis | Ultrasonography of abdomen4 | Consider CT if ultrasonography is nondiagnostic, presentation is atypical, or patient is critically ill |
| Appendicitis | CT of abdomen and pelvis with contrast media5 | — |
| Cholecystitis | Ultrasonography of abdomen6 | Cholescintigraphy or CT may be considered if ultrasonography is equivocal |
| Crohn disease | CT enterography7 | Choice of examination depends on institutional preferences and resources |
| Diverticulitis | CT of abdomen and pelvis with contrast media8 | Patients with typical symptoms and no suspected complications may not require imaging |
| Ectopic pregnancy | Ultrasonography of pelvis (transvaginal and transabdominal)9 | — |
| Gastroenteritis | Imaging not typically indicated | — |
| Herpes zoster infection | Imaging not typically indicated | — |
| Intrauterine pregnancy | Ultrasonography of pelvis (transvaginal and transabdominal)9 | — |
| Irritable bowel syndrome | Imaging not typically indicated | — |
| Mesenteric ischemia | CT angiography of abdomen with contrast media10 | Conventional angiography is invasive but may be considered to diagnose and treat with a single procedure |
| Muscle strain | Imaging not typically indicated | — |
| Nephrolithiasis | CT of abdomen and pelvis without contrast media11 | Ultrasonography may be considered if CT is unavailable; ultrasonography may help detect obstruction but has poor sensitivity for visualizing stones |
| Ovarian torsion | Ultrasonography of pelvis (transvaginal and transabdominal)9 | — |
| Pelvic inflammatory disease | Imaging not typically indicated | — |
| Small bowel obstruction | CT of abdomen and pelvis with contrast media12 | Conventional radiography may be appropriate for initial evaluation |
| Urinary tract infection | Imaging not typically indicated | — |
The location of pain is often a helpful starting point. The American College of Radiology (ACR) has developed evidence-based guidelines, the ACR Appropriateness Criteria, to help physicians make the most appropriate imaging decisions for specific clinical conditions. The ACR Appropriateness Criteria for abdominal imaging are based primarily on the location of pain. For most locations, the ACR provides several clinical variants (e.g., presence or absence of fever, leukocytosis, pregnancy) and outlines the appropriate imaging for each scenario. This article includes one clinical variant for each pain location; tables for all clinical variants are available at https://acsearch.acr.org/list.
Right Upper Quadrant Pain
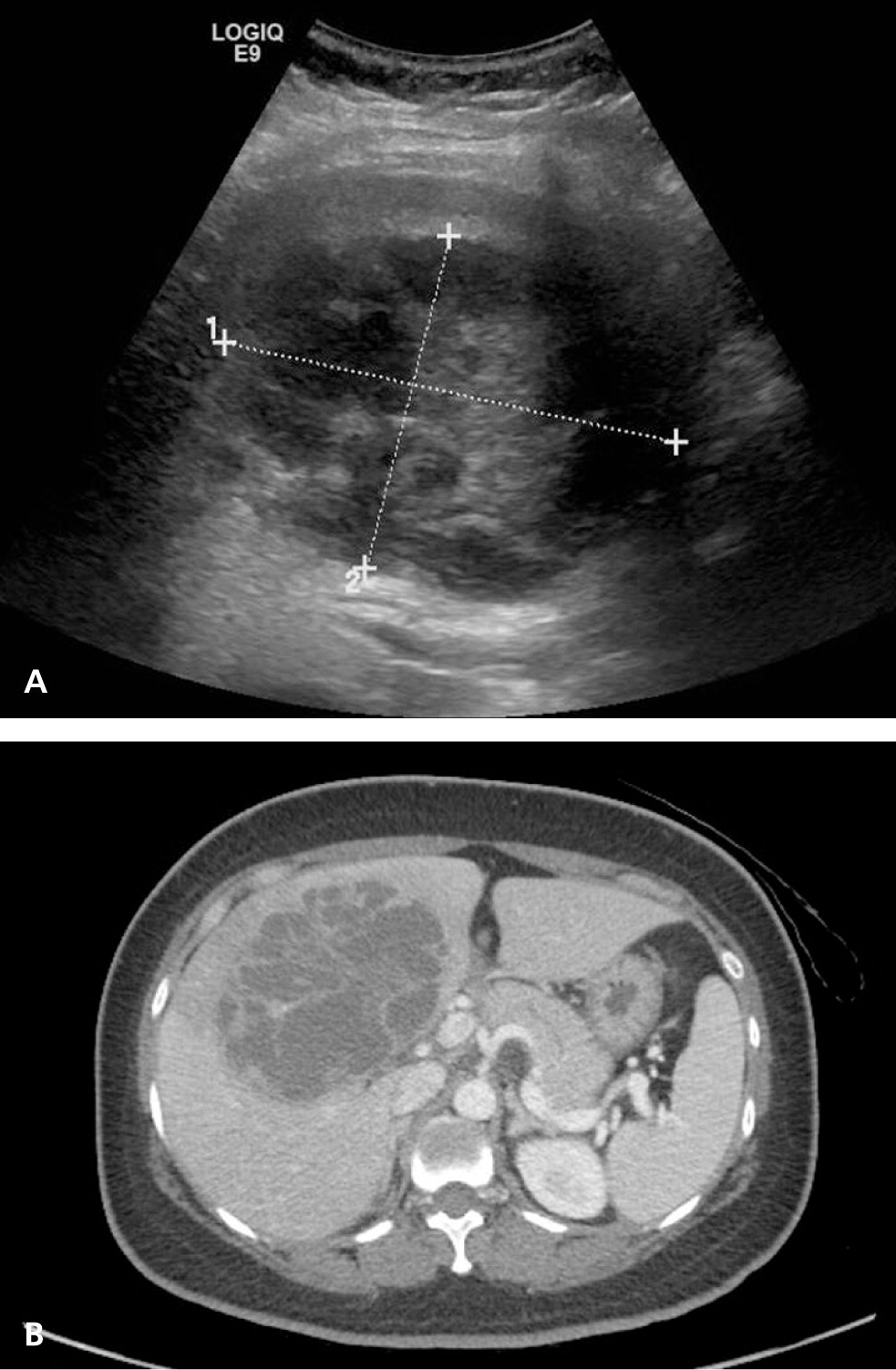
Acute cholecystitis is a primary diagnostic consideration in patients presenting with new-onset right upper quadrant pain. History, physical examination, and laboratory testing are often insufficient for diagnosing acute cholecystitis without further workup.13 The ACR Appropriateness Criteria recommend ultrasonography as the initial imaging test for patients presenting with right upper quadrant pain (Table 2).6 Although a meta-analysis of 57 studies from 1978 to 2010 showed that cholescintigraphy has better sensitivity and specificity (96% and 90%, respectively) than ultrasonography (81% and 83%, respectively) for detecting acute cholecystitis,14 ultrasonography is more readily available, can identify other potential causes of pain (Figure 1A), and does not expose the patient to ionizing radiation.
| Radiologic procedure | Rating | Comments | Relative radiation level |
|---|---|---|---|
| Ultrasonography of abdomen | 9 | — | 0 |
| MRI of abdomen without and with contrast media | 6 | See statement regarding contrast media under anticipated exceptions* | 0 |
| Cholescintigraphy | 6 | Based on ultrasound findings, this generally should follow ultrasonography of the right upper quadrant | ☢☢ |
| CT of abdomen with contrast media | 6 | — | ☢☢☢ |
| MRI of abdomen without contrast media | 4 | — | 0 |
| CT of abdomen without contrast media | 4 | — | ☢☢☢ |
| CT of abdomen without and with contrast media | 3 | — | ☢☢☢☢ |
Computed tomography (CT) has not been widely studied for the evaluation of right upper quadrant pain.14 It may be considered in patients with inconclusive ultrasonography or cholescintigraphy results or to help guide surgical planning6 (Figure 1B). Several small studies of magnetic resonance imaging (MRI) suggest that it may be useful for evaluating acute cholecystitis, with a sensitivity (85%) and specificity (81%) similar to that of ultrasonography.14 MRI can be used in patients with equivocal ultrasonography findings or to visualize hepatic and biliary abnormalities that cannot be characterized on ultrasonography.6
Right Lower Quadrant Pain
Acute appendicitis is the most common cause of right lower quadrant pain requiring surgery5 and is the focus of imaging considerations in this location. The ACR Appropriateness Criteria recommend CT as the initial imaging test of choice for patients presenting with right lower quadrant pain (Table 3).5 A meta-analysis of six studies from 1994 to 2005 found that CT has better sensitivity and specificity (91% and 90%, respectively) than ultrasonography (78% and 83%, respectively) for detecting acute appendicitis15 (Figure 2). CT also provides more consistent results than ultrasonography,5 because ultrasonography is a highly operator-dependent technique that varies based on the skill and experience level of the technologist and radiologist. Routine use of CT for evaluation of appendicitis has reduced the negative-finding appendectomy rate from 24% to 3%,16 and it has been shown to decrease overall costs by $447 per patient by preventing unnecessary appendectomies and hospital admissions.17
| Radiologic procedure | Rating | Comments | Relative radiation level |
|---|---|---|---|
| CT of abdomen and pelvis with contrast media | 8 | Oral or rectal contrast media may not be needed depending on institutional preference | ☢☢☢☢ |
| CT of abdomen and pelvis without contrast media | 7 | Use of oral or rectal contrast media depends on institutional preference | ☢☢☢☢ |
| Ultrasonography of abdomen | 6 | Perform this procedure with graded compression | 0 |
| Ultrasonography of pelvis | 5 | This procedure is appropriate in women with pelvic pain | 0 |
| MRI of abdomen and pelvis without and with contrast media | 5 | See statement regarding contrast media under anticipated exceptions (Table 2) | 0 |
| Radiography of abdomen | 4 | This procedure may be useful when there is concern for perforation and free air | ☢☢ |
| CT of abdomen and pelvis without and with contrast media | 4 | Oral or rectal contrast media may not be needed depending on institutional preference | ☢☢☢☢ |
| MRI of abdomen and pelvis without contrast media | 4 | — | 0 |
| Radiography with contrast enema | 2 | — | ☢☢☢ |
| Technetium 99m white blood cell scan of abdomen and pelvis | 2 | — | ☢☢☢☢ |

Left Lower Quadrant Pain
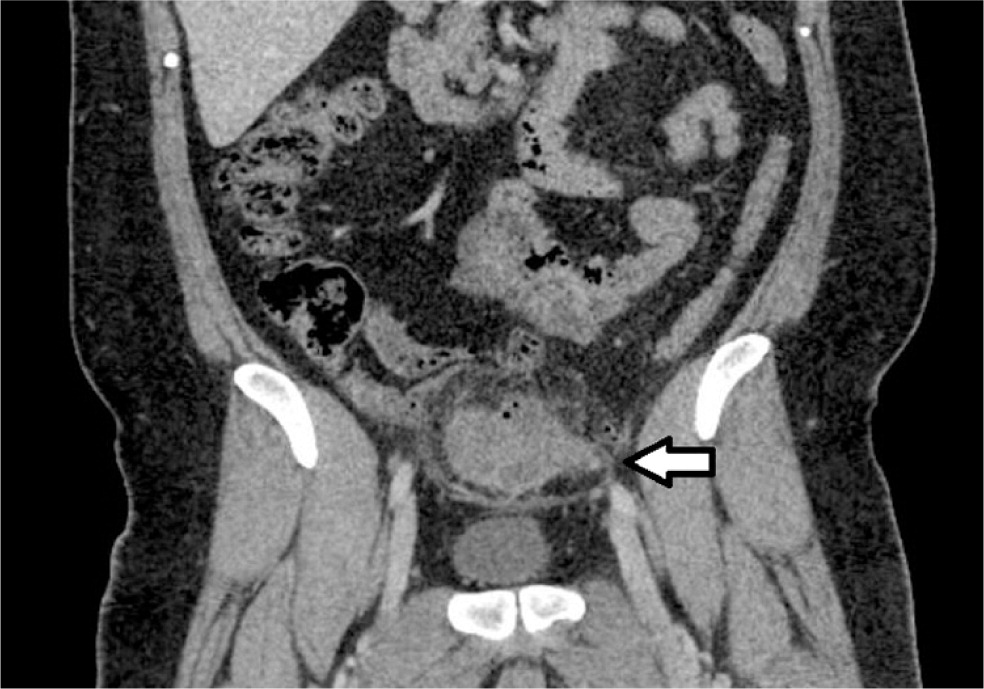
Acute sigmoid diverticulitis is the most common cause of left lower quadrant pain in adults and is the focus of imaging recommendations for this quadrant. Diverticulitis is often diagnosed clinically without radiologic examination, but imaging should be considered if the diagnosis is unclear or if complications (e.g., abscess, fistula, obstruction, perforation) are suspected (Figure 3). The ACR recommends CT as the initial imaging test for the evaluation of left lower quadrant pain (Table 4).8 CT has a sensitivity of greater than 95% for detecting diverticulitis,18 and it can provide information about the extent of disease and the presence of abscess formation.8 In addition, CT can reveal disease processes other than diverticulitis that have a similar clinical presentation.
| Radiologic procedure | Rating | Comments | Relative radiation level |
|---|---|---|---|
| CT of abdomen and pelvis with contrast media | 9 | For the procedure, oral and/or colonic contrast may be helpful for bowel luminal visualization | ☢☢☢☢ |
| CT of abdomen and pelvis without contrast media | 6 | — | ☢☢☢☢ |
| CT of abdomen and pelvis without and with contrast media | 5 | — | ☢☢☢☢ |
| MRI of abdomen and pelvis without contrast media | 5 | — | 0 |
| MRI of abdomen and pelvis without and with contrast media | 5 | See statement regarding contrast media under anticipated exceptions (Table 2) | 0 |
| Radiography with contrast enema | 4 | — | ☢☢☢ |
| Ultrasonography of abdomen, transabdominal graded compression | 4 | — | 0 |
| Radiography of abdomen and pelvis | 4 | — | ☢☢☢ |
| Ultrasonography of pelvis, transvaginal | 2 | — | 0 |
Ultrasonography has also been studied for evaluation of suspected diverticulitis. Although some studies have shown similar sensitivity of ultrasonography compared with CT for detecting diverticulitis, others have shown significantly lower sensitivity with ultrasonography.19 Variation in ultrasonography results may be due to the highly operator-dependent technique and the limitations of patient body habitus, compared with other imaging modalities. Preliminary data on the use of MRI for the evaluation of diverticulitis suggest that it may be useful, with sensitivity of 86% to 94% and specificity of 88% to 92%.8
Nonlocalized Abdominal Pain
Although certain disease processes such as cholecystitis, appendicitis, and diverticulitis commonly present with pain localized to a specific quadrant of the abdomen, diffuse abdominal pain is also a common clinical presentation. The differential diagnosis of acute nonlocalized abdominal pain is broad. CT is typically the imaging modality of choice if there is significant concern for serious pathology or if the diagnosis is unclear from history, physical examination, and laboratory testing (Table 5).3 A prospective study of 584 patients with nontraumatic abdominal pain in an emergency department setting found that CT results altered the leading diagnosis in 49% of patients and changed the management plan in 42% of patients.20
| Radiologic procedure | Rating | Comments | Relative radiation level |
|---|---|---|---|
| CT of abdomen and pelvis with contrast media | 8 | — | ☢☢☢☢ |
| CT of abdomen and pelvis without contrast media | 6 | — | ☢☢☢☢ |
| Ultrasonography of abdomen | 6 | — | 0 |
| Radiography of abdomen | 6 | To evaluate for bowel perforation | ☢☢ |
| MRI of abdomen and pelvis without contrast media | 5 | — | 0 |
| MRI of abdomen and pelvis without and with contrast media | 5 | See statement regarding contrast media under anticipated exceptions (Table 2) | 0 |
| Radiography of upper gastrointestinal series with small bowel follow-through | 4 | — | ☢☢☢ |
| Radiography with contrast enema | 4 | — | ☢☢☢ |
| CT of abdomen and pelvis without and with contrast media | 3 | May be helpful in select cases but should be used with caution because of increased radiation dose | ☢☢☢☢ |
| Gallium 67 scan of abdomen | 3 | — | ☢☢☢☢ |
| Technetium 99m white blood cell scan of abdomen and pelvis | 3 | — | ☢☢☢☢ |
| Indium 111 white blood cell scan of abdomen and pelvis | 3 | — | ☢☢☢☢ |
Special Considerations
CONVENTIONAL RADIOGRAPHY
Conventional radiography is widely available in the ambulatory setting and is often the initial imaging test for evaluation of outpatients with abdominal pain. However, studies have shown that it has limited diagnostic value for assessing abdominal pain and that the results rarely change patient treatment.21 Conventional radiography may be appropriate for a select group of patients. It has been shown to have good accuracy for diagnosing suspected bowel obstruction, perforated viscus, urinary tract calculi, or foreign bodies.22
IONIZING RADIATION
The use of CT for the evaluation of abdominal pain has increased significantly in recent years. In 2001, approximately 10% of patients with abdominal pain who presented to U.S. emergency departments underwent CT. By 2005, that number increased to more than 22% of patients.23 With the widespread use of CT comes concerns about exposing patients to ionizing radiation. Abdominal CT exposes a patient to an effective radiation dose of approximately 10 mSv, compared with the annual background radiation dose of 3 mSv in the United States.22
In the interest of decreasing radiation exposure, efforts have been made to use CT more judiciously. For example, studies have evaluated ultrasonography as the initial imaging modality for suspected appendicitis, using CT only if the ultrasonography results are inconclusive or negative. These studies have shown significant decreases in CT use while maintaining acceptable diagnostic sensitivity and specificity.5 The use of low-dose CT for evaluating suspected appendicitis is another strategy to decrease radiation exposure. A study of low-dose CT compared with standard-dose CT found no significant difference in the negative appendectomy rate between the two groups, and the median radiation dose of the low-dose protocol was 22% of the standard-dose protocol.24 MRI is an emerging modality in the evaluation of suspected appendicitis, showing excellent sensitivity and specificity (97% and 95%, respectively) in a meta-analysis of eight studies.5 MRI avoids radiation exposure altogether, but its high cost and lack of widespread availability continue to limit its use.
CONTRAST ENHANCEMENT
The decision to use oral or intravenous contrast media with abdominal imaging depends on the suspected diagnosis as well as specific patient characteristics. Oral contrast media is used for bowel visualization, and intravenous contrast media allows for enhanced visualization of vascular structures and solid organs.25 The ACR Appropriateness Criteria outline whether contrast is recommended for various indications (Tables 1 through 53–12 and eTable A), and note that protocols on the use of contrast media vary among institutions. Although studies have shown improved sensitivity and specificity for diagnosing acute abdominal pain with the use of contrast enhancement, the accuracy of CT or MRI remains high regardless of the use of contrast media.5
REPRODUCTIVE-AGED FEMALES
In females of reproductive age, gynecologic and obstetric causes of abdominal pain (e.g., ectopic pregnancy, ovarian cyst, ovarian torsion, pelvic inflammatory disease) are important considerations in addition to the diagnoses commonly made in the general population. Before ordering diagnostic imaging in premenopausal women, it is important to consider obtaining a beta human chorionic gonadotropin (β-hCG) measurement to narrow the differential diagnosis and to limit the possibility of exposing an embryo or fetus to ionizing radiation. Transvaginal or transabdominal ultrasonography of the pelvis is the recommended imaging study for reproductive-aged females in whom a gynecologic etiology is suspected or a β-hCG test result is positive.9
In pregnant patients with acute abdominal pain, ultrasonography and MRI are typically the imaging studies of choice because they lack ionizing radiation (eTable A). MRI has been shown to have excellent sensitivity and specificity for the diagnosis of appendicitis in pregnant women and is useful for evaluating other causes of abdominal pain as well.9 If ultrasonography and MRI are unavailable or inconclusive and if serious pathology remains a concern, CT can be used. The risk of a negative outcome for a developing embryo or fetus exposed to a single CT of the abdomen and pelvis is very low.26 The ACR practice parameter regarding the use of imaging with ionizing radiation in pregnant patients outlines the specific risks based on gestational age, and emphasizes the importance of obtaining informed consent from the patient before imaging is performed.26
| Radiologic procedure | Rating | Comments | Relative radiation level |
|---|---|---|---|
| Ultrasonography of abdomen | 8 | — | 0 |
| MRI of abdomen and pelvis without contrast media | 7 | — | 0 |
| CT of abdomen and pelvis with contrast media | 5 | Only after other studies without ionizing radiation have been used | ☢☢☢☢ |
| CT of abdomen and pelvis without contrast media | 5 | — | ☢☢☢☢ |
| Radiography of abdomen | 4 | To evaluate for bowel perforation | ☢☢ |
| CT of abdomen and pelvis without and with contrast media | 2 | May be helpful in select cases but should be used with caution because of increased radiation dose | ☢☢☢☢ |
| MRI of abdomen and pelvis without and with contrast media | 2 | Because it is unclear how gadolinium-based contrast agents will affect the fetus, these agents should be administered with extreme caution | 0 |
| Gadolinium-based contrast agents are recommended for use during pregnancy only when there are no alternatives and benefit outweighs risk | |||
| Radiography of upper gastrointestinal series with small bowel follow-through | 2 | — | ☢☢☢ |
| Radiography with contrast enema | 2 | — | ☢☢☢ |
| Gallium 67 scan of abdomen | 2 | — | ☢☢☢☢ |
| Technetium 99m white blood cell scan of abdomen and pelvis | 2 | — | ☢☢☢☢ |
| Indium 111 white blood cell scan of abdomen and pelvis | 2 | — | ☢☢☢☢ |
Data Sources: We reviewed the American College of Radiology Appropriateness Criteria at https://acsearch.acr.org/list. We reviewed the relevant guidelines on that website, including acute nonlocalized abdominal pain, left lower quadrant pain, right lower quadrant pain, right upper quadrant pain, and acute pelvic pain in the reproductive age group. We then conducted literature searches using PubMed with search terms including diagnostic imaging of abdominal pain in adults, trends in imaging abdominal pain, and pregnancy testing prior to diagnostic imaging. Search dates: May 2014 through January 2015.
