
A more recent article on fibromyalgia is available.
Am Fam Physician. 2015;91(7):472-478
Author disclosure: No relevant financial affiliations.
Fibromyalgia has a distinct pathophysiology involving central amplification of peripheral sensory signals. Core symptoms are chronic widespread pain, fatigue, and sleep disturbance. Most patients with fibromyalgia have muscle pain and tenderness, forgetfulness or problems concentrating, and significant functional limitations. Fibromyalgia is diagnosed using an updated set of clinical criteria that no longer depend on tender point examination; laboratory testing may rule out other disorders that commonly present with fatigue, such as anemia and thyroid disease. Patients with fibromyalgia should be evaluated for comorbid functional pain syndromes and mood disorders. Management of fibromyalgia should include patient education, symptom relief, and regular aerobic physical activity. Serotonin-norepinephrine reuptake inhibitors, tricyclic antidepressants, antiepileptics, and muscle relaxants have the strongest evidence of benefit for improving pain, fatigue, sleep symptoms, and quality of life. Multiple complementary and alternative medicine therapies have been used but have limited evidence of effectiveness. Opioids should be used to relieve pain in carefully selected patients only if alternative therapies are ineffective.
Patients who present with chronic pain, mood symptoms, and fatigue can represent a diagnostic challenge for the primary care physician. Many of these patients meet the criteria for fibromyalgia, a condition that can generate uncertainty and potential frustration in primary care management. Recent studies have improved our understanding of the pathophysiology, clinical diagnosis, and effective management of this condition, making it a disorder that can be appropriately managed by the primary care physician.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| A combination of the 2010 diagnostic criteria from the American College of Rheumatology, symptom scores, and presence of chronic widespread pain with fatigue and sleep symptoms should be used to diagnose fibromyalgia. | C | 1, 4, 5 |
| Patients with fibromyalgia should be evaluated for comorbid functional pain syndromes and mood disorders. | C | 7–12 |
| Aerobic exercise (20 to 30 minutes two or three days per week) improves pain symptoms and fatigue in patients with fibromyalgia. | A | 17, 18 |
| Tricyclic antidepressants, serotonin-norepinephrine reuptake inhibitors, and cyclobenzaprine (Flexeril) have the strongest evidence of benefit for improvements in pain, sleep, and quality of life in patients with fibromyalgia. Tricyclic antidepressants and serotonin-norepinephrine reuptake inhibitors improve symptoms of fatigue. | A | 22, 23, 25 |
| Antiepileptics may provide benefits for pain, sleep, and quality of life in patients with fibromyalgia. | C | 24 |
| Recommendation | Sponsoring organization |
|---|---|
| Do not test ANA subserologies without a positive ANA and clinical suspicion of immune-mediated disease. | American College of Rheumatology |
| Do not test for Lyme disease as a cause of musculoskeletal symptoms without an exposure history and appropriate physical examination findings. | American College of Rheumatology |
How Is Fibromyalgia Diagnosed?
Fibromyalgia should be suspected in patients with a combination of widespread chronic pain, fatigue, and sleep disturbance. There is no preferred method to diagnose fibromyalgia, and different methods identify slightly different (overlapping) populations of patients. “Tender point” diagnostic criteria were developed for use in clinical trials, and newer criteria will detect additional patients who have fibromyalgia but do not meet tender point criteria. Laboratory testing may be helpful to rule out other disorders that commonly present with fatigue, such as anemia and thyroid disease. However, extensive testing is usually not necessary.
EVIDENCE SUMMARY
Patients with fibromyalgia represent a heterogeneous population, with variable presence and severity of symptoms, and variable functional impairment and impact on quality of life. The core symptoms include widespread pain (right and left sides of the body, above and below the waist, and in the axial skeleton) of at least three months' duration, fatigue, and sleep disturbance. Tenderness of muscles and tendon insertion sites, joint stiffness, mood disturbance, and cognitive symptoms (e.g., forgetfulness, problems concentrating) are typical symptoms, and patients often report limitations in physical functioning.1
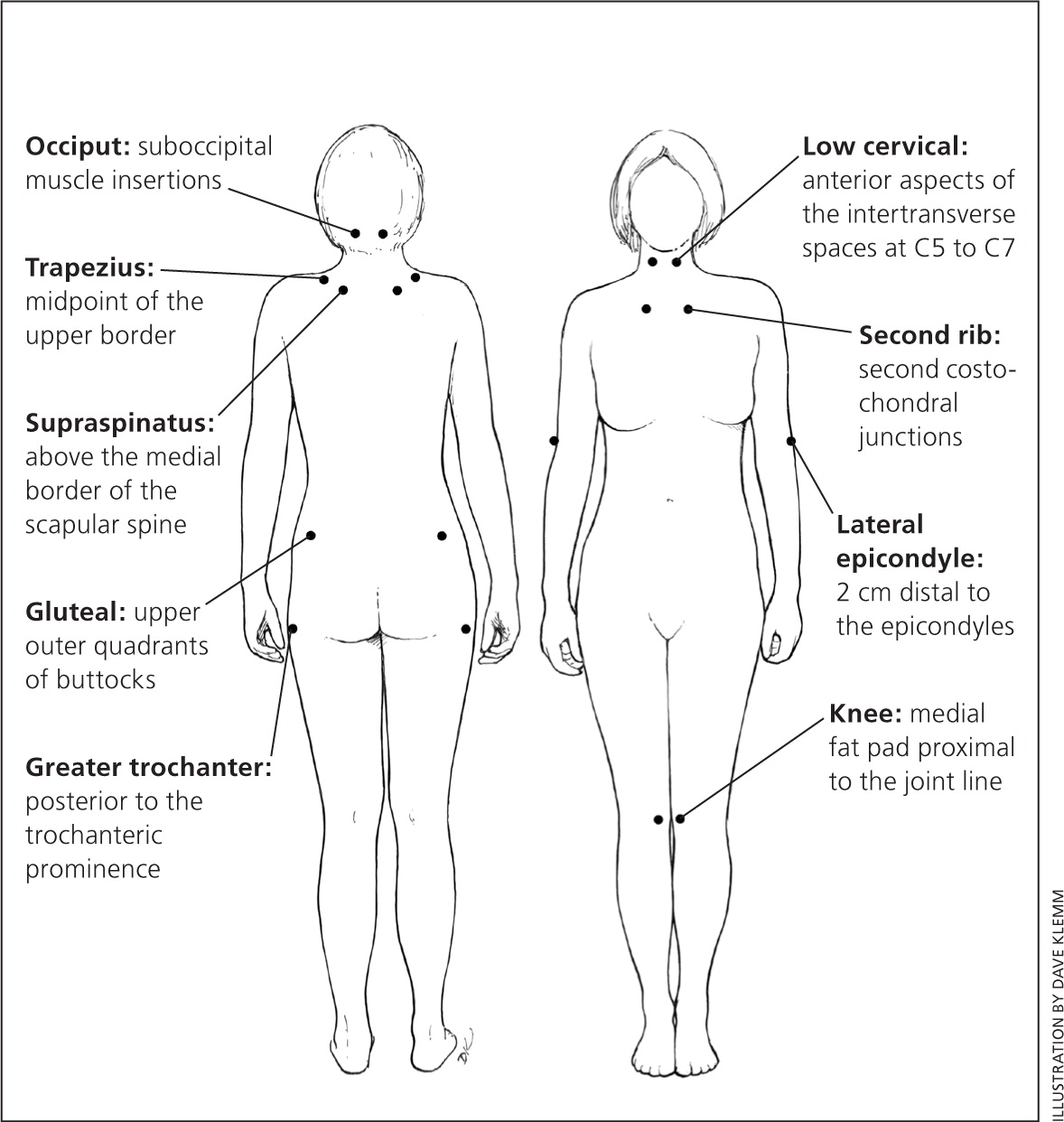
The 1990 American College of Rheumatology diagnostic criteria for fibromyalgia emphasized pain on digital palpation of at least 11 of 18 designated tender point sites (Figure 12 ), as well as widespread chronic pain.3 Examiners should apply just enough pressure to cause the nail bed to blanch. These criteria have a sensitivity of 88% and a specificity of 81%,1 compared with patients who have an existing diagnosis of fibromyalgia using the investigator's usual method of diagnosis.3 Tender point criteria miss a subpopulation of patients with fibromyalgia, including those who do not meet the criteria at the time they are examined.
A comparison of diagnosis based on the tender point criteria, a symptom survey, and an overall assessment by an experienced clinician found that all three methods identify patients who are thought to have fibromyalgia.4 For example, among 120 patients who would be diagnosed by at least one method, 84% would be diagnosed by clinician assessment, 69% by survey diagnostic criteria, and 50% by tender point criteria; only 33% would be diagnosed by all three methods.
Laboratory testing is not necessary to diagnose fibromyalgia. However, testing patients with chronic fatigue for anemia, electrolyte disturbances, and thyroid disease is recommended. In the absence of suggestive symptoms, diagnoses such as systemic lupus erythematosus, rheumatoid arthritis, or other connective tissue disorders are unlikely. Erythrocyte sedimentation rate, C-reactive protein level, and rheumatoid factor testing have poor specificity and should be ordered only if connective tissue disorders are suspected.
Fibromyalgia should be strongly suspected based on clinical findings. Formal symptom surveys or tender point examination can be performed to support the diagnosis, but not to exclude it. Regardless of the method used, establishing the diagnosis will help validate the patient's experience of symptoms and lead to more efficient implementation of a treatment plan.
Which Conditions Are Associated with Fibromyalgia?
Fibromyalgia is caused by central amplification of peripheral sensory signals, so that normal sensations are perceived as painful. Because this pathophysiology is shared with other chronic functional pain syndromes, it is appropriate to evaluate patients for these conditions. Patients with fibromyalgia should be evaluated and treated for mood disorders and sleep disturbance. Posttraumatic stress disorder (PTSD), traumatic experiences, and chronic widespread pain coexist in many patients with fibromyalgia, although there is no clear causal or temporal relationship.
EVIDENCE SUMMARY
The underlying pathophysiology of fibromyalgia—heightened central sensitivity to peripheral sensations6—is shared by other functional pain syndromes,1 and these conditions are more common in patients with fibromyalgia. Approximately 30% of patients with irritable bowel syndrome have fibromyalgia, and 30% to 70% of patients with fibromyalgia have irritable bowel syndrome.7 Other functional pain disorders that are more common in patients with fibromyalgia include vulvodynia, interstitial cystitis, temporomandibular joint pain, chronic back pain, endometriosis, and noncardiac chest pain.8–11
Mood disturbance is a feature of many rheumatologic conditions. The association between pain and mood is complex and bidirectional.12 Depression and chronic pain seem to share many different underlying physiologic triggers.
The relationship between fibromyalgia and PTSD is complex. Up to 45% of patients with fibromyalgia meet criteria for PTSD, compared with 3% of population-based control subjects.13 Traumatic experiences and PTSD symptoms may precede or follow the onset of chronic widespread pain. PTSD is a risk factor for fibromyalgia, and vice versa; these conditions likely share antecedent traumatic experiences. A history of sexual abuse is associated with chronic nonspecific pain, and a history of rape is associated with fibromyalgia.14
How Do Patient Education and Counseling Affect Symptoms and Outcomes?
Establishing and explaining the diagnosis of fibromyalgia appear to improve patients' well-being and functionality, as well as reduce symptoms and costs of care.
EVIDENCE SUMMARY
Patients with fibromyalgia have often had disabling pain and fatigue for months or years, sought treatment from many physicians, had multiple diagnostic tests or ineffective treatments, and been told that there is nothing wrong. Establishing the diagnosis and educating patients about their illness are essential parts of fibromyalgia management.1 Once the diagnosis has been made, patients report improved satisfaction with health, fewer long-term symptoms, and reduced health care utilization and costs.15 Patient education, empiric treatment, and laboratory testing for other conditions that cause fatigue can proceed concurrently.
Does Exercise Benefit Patients with Fibromyalgia?
Pain and functionality are improved with regular exercise of moderate intensity in patients with fibromyalgia. Patients should be counseled about the effectiveness of exercise and given specific instructions for exercise type, frequency (at least two or three days per week), and duration (20 to 30 minutes at a time). Although aerobic exercise has the strongest evidence of effectiveness, stretching or flexibility exercises, strengthening exercises, yoga, and tai chi seem to improve symptoms as well. Patient interest and ability to continue the activity should guide the type of exercise. Frequent supportive reinforcement may be necessary to maximize adherence to exercise regimens.
EVIDENCE SUMMARY
Regular physical activity is an important part of fibromyalgia management. An exercise prescription specifying the type, frequency, and duration of activity may help ensure patient understanding and adherence. Aerobic exercise (moderate intensity, for 20 to 30 minutes two or three days per week) has the most consistent evidence for improvement in pain and mood symptoms, and in overall functional status.17,18 Other types of exercise, such as stretching or flexibility exercises, strengthening exercises,19,20 yoga, and tai chi,21 have limited evidence but seem to improve symptoms.
Which Pharmacologic Treatments Are Most Effective?
Duloxetine (Cymbalta), milnacipran, and pregabalin (Lyrica) are approved by the U.S. Food and Drug Administration for treatment of fibromyalgia. These drugs are effective for treating multiple symptoms. Serotonin-norepinephrine reuptake inhibitors are generally the most effective antidepressants, although tricyclic antidepressants are more effective for treating fatigue. Cyclobenzaprine (Flexeril) improves pain and sleep quality. Opioids, nonsteroidal anti-inflammatory drugs, and other analgesics are often used in patients with fibromyalgia, but they have limited effectiveness and are associated with serious adverse effects.
EVIDENCE SUMMARY
All studies and systematic reviews of drug treatments for fibromyalgia are hampered by small sample sizes and short study durations (typically not longer than a few months), which makes it difficult to compare long-term benefits. Antidepressants or antiepileptics are reasonable options for initial treatment, with subsequent assessment of patient response. A dosage adjustment, medication change, or addition of an adjunct medication may be effective in patients with partial or no response to antidepressants or antiepileptics.
Antidepressants. Tricyclic antidepressants reduce pain, fatigue, and sleep disturbances; selective serotonin reuptake inhibitors have slight benefit for reducing pain; and serotonin-norepinephrine reuptake inhibitors have some benefit for reducing pain, sleep disturbances, and depressed mood.22 The average benefit of amitriptyline, duloxetine, and milnacipran is small, and rates of adverse effects are similar.23 Amitriptyline is superior to duloxetine and milnacipran in reduction of pain, sleep disturbances, fatigue, and limitations of health-related quality of life. The approximate number needed to treat for a 30% pain reduction is four for amitriptyline, nine for duloxetine, and 11 for milnacipran.23
Antiepileptics. Pregabalin and gabapentin (Neurontin) may be useful adjunct treatments to reduce pain in some patients with fibromyalgia. However, their use is often limited by cognitive or other adverse effects.24
Muscle Relaxants. Muscle relaxants can be useful when combined with antidepressants or antiepileptics. Cyclobenzaprine improves fibromyalgia-associated pain and sleep quality, but not fatigue.25
Opioids. The use of opioids in patients with fibromyalgia is challenging and controversial.26 One meta-analysis of opioids for treatment of chronic noncancer pain found that tramadol (Ultram) and other opioids had some benefit for fibromyalgia pain and functionality scores.27 However, other systematic reviews have found no benefit and an increased rate of adverse effects, based on a small number of studies.28,29 The primary concerns for opioid use in fibromyalgia include an unclear mechanism of action, cognitive and other adverse effects, potential opioid-induced allodynia or hyperalgesia, and concerns about opioid addiction, misuse, and diversion. However, opioids can be used safely in some patients. A reduction in peripheral sensory signals may reduce central amplification of pain, suggesting a possible mechanism of benefit. Table 1 outlines patient selection principles for opioid use in fibromyalgia.30
| Try other treatments first |
| Reevaluate to confirm fibromyalgia as the diagnosis, potentially with rheumatology consultation |
| Ensure that adequate trials of multiple serotonin-norepinephrine reuptake inhibitors, antidepressants, antiepileptics, muscle relaxants, exercise interventions, and other treatments have been ineffective |
| Identify and treat psychiatric comorbidities |
| Document which treatments have been tried, and the outcomes of each |
| Assess for risk of medication misuse |
| Obtain and document personal or family history of medication or substance abuse |
| Consider using a formal risk assessment tool |
| Educate the patient |
| Discuss risks and benefits of opioid use |
| Describe need for periodic monitoring and assessment |
| Establish and assess treatment goals |
| Discuss treatment goals for pain relief and functional improvement; emphasize that complete pain relief is unlikely |
| Determine a method to track symptoms (e.g., symptom diary, smartphone app) |
| Select a medication regimen |
| Consider using a long-acting opioid on a scheduled (not as-needed) basis |
| Consider use of a bowel regimen to prevent drug-induced constipation |
| Monitor for misuse and adverse effects |
| Schedule regular follow-up visits |
| Obtain periodic urine drug tests |
| At subsequent visits, ask about symptom relief, functional status, and adverse effects |
| If available, obtain a report of controlled medication prescriptions |
Are There Any Effective Complementary and Alternative Medicine Treatments for Fibromyalgia?
Many complementary and alternative medicine (CAM) therapies are used by patients with fibromyalgia. Although individual patients may benefit from these therapies, none has strong evidence for effectiveness in the general population.
EVIDENCE SUMMARY
Most patients with fibromyalgia try CAM therapies at some point.31 Recent systematic reviews have evaluated various CAM therapies in fibromyalgia, including massage, hydrotherapy, acupuncture, homeopathic remedies (e.g., vitamins, plant-based products), anthocyanidins, capsaicin, and S-adenosylmethionine.31,32 None had any consistent benefit; however, they are considered promising for providing relief in some patients. Other CAM therapies (e.g., nutritional, herbal, and hormonal supplements; ayurvedic medicine; hypnosis) have not been adequately studied.
Physicians should work with patients who are interested in CAM therapies and use symptom diaries or other measures (including smartphone apps) to assess their impact. This approach allows patients to potentially benefit from treatments, while limiting adverse effects, drug-herb interactions, and needless costs.
Data Sources: We searched Medline using the keyword fibromyalgia and the medical subject heading fibromyalgia. The search was limited to English, human, core clinical journals (AIM), and publication years 2004 to 2014. Additional searches were conducted combining the baseline search with searches for the terms opioids, irritable bowel syndrome, exercise, PTSD, and other relevant terms. Reference lists of retrieved reviews were also used to identify additional relevant original studies. Search dates: April 18, 2014, and December 15, 2014.
