
Am Fam Physician. 2015;91(9):649-650
Author disclosure: No relevant financial affiliations.
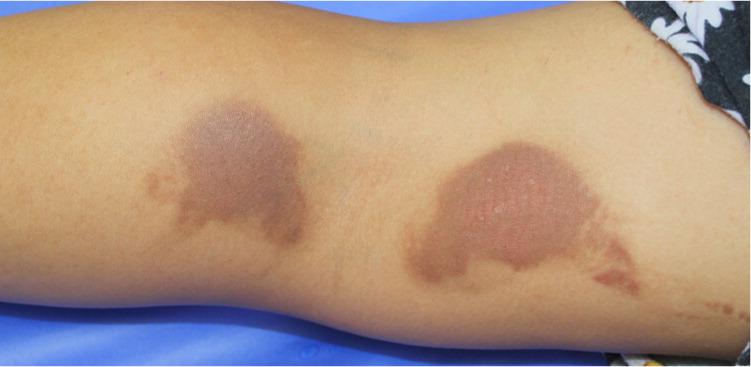
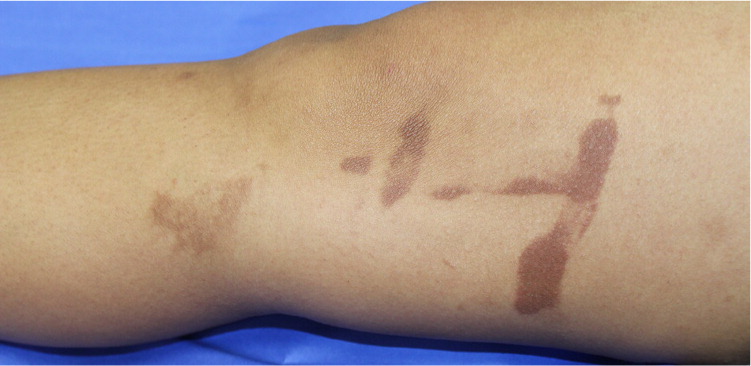
A 17-year-old girl presented with a bruise-like rash on her legs. The rash had appeared three days prior, after she had eaten limes and rolled down a grassy hill with friends. The rash was initially brightly erythematous, and it was associated with a burning sensation. She had a history of asthma and eczema.
Question
Discussion
The correct answer is D: phytophotodermatitis. Phytophotodermatitis is a phototoxic eruption (i.e., an enhanced sunburn) that occurs when the skin is exposed to a photosensitizing compound called a psoralen, then exposed to sunlight. The most common source of psoralen is citrus fruits such as lemons, limes, and bergamot oranges. Other sources include figs, parsnips, celery, carrots, dill, and mustard. Heat, sweating, and wet skin intensify the process. Phototoxic reactions differ from photoallergic reactions in that they can happen at any time, without prior sensitization.1–3 Phytophotodermatitis is more common in the summer. It may occur as an occupational hazard of bartenders, agricultural workers, florists, gardeners, and grocers.4
Phytophotodermatitis typically presents 24 hours after exposure with an erythematous rash that is accompanied by vesicles and a burning sensation. Symptom severity peaks within 48 to 72 hours, then characteristic hyperpigmentation gradually develops. The hyperpigmentation lasts weeks to months, but may occasionally last years in individuals with darker skin. The distribution offers diagnostic clues. Irregular or bizarre sunburns, preferential involvement of the dorsal hands and fingers, drip marks, hyperpigmented hand-prints, or kissing lesions on flexural surfaces suggest phytophotodermatitis.1–3
Allergic contact dermatitis manifests as an acute eczematous dermatitis after prior sensitization. The rash is characterized by pruritic papules and vesicles on an erythematous base. Causes include exposure to plants such as poison ivy and oak, topical medications such as bacitracin, metals such as nickel, and personal care products such as cosmetics, perfumes, lotions, and soaps. Allergen exposure, pruritus, and expansion of the rash slightly beyond the site of exposure differentiate allergic contact dermatitis from phytophotodermatitis.
Chemical burns may be difficult to distinguish from phytophotodermatitis because both present with erythema, vesicles, and eventual hyperpigmentation in odd, geometric shapes. Clinical history of exposure can differentiate between these two diagnoses.
Child abuse should be considered in the differential diagnosis of any injured child. Clues to abuse include an unusual distribution or location of lesions, a hand-print bruise that is adult-sized, or a pattern of bruises or marks in various stages of healing and incongruous with the patient's history.5,6
| Condition | Rash characteristics | Exposures |
|---|---|---|
| Allergic contact dermatitis | Pruritic papules and vesicles on an erythematous base, at the site of exposure or diffusely across the body | Plants (e.g., poison ivy and oak), topical medications (e.g., bacitracin), metals (e.g., nickel), personal care products (e.g., cosmetics, perfumes, lotions, soaps); prior sensitization is required |
| Chemical burns | Erythematous plaques and vesicles that resolve with hyperpigmentation | Cleaning agents, car battery acid, bleach, ammonia, denture cleaners, teeth whitening products, swimming pool chlorinating products |
| Child abuse | Geometric lesions resembling hands or fingers in various stages of healing; bruising in atypical locations (e.g., ear, soft tissue, cheek) | Injury secondary to foreign objects; patterns that are incongruous with history |
| Phytophotodermatitis | Brightly erythematous geometric patches associated with burning; resolves with hyperpigmentation, which may last for months | Psoralen; common sources include citrus fruits (e.g., lemons, limes, bergamot oranges), figs, parsnips, celery, carrots, dill, and mustard |
The views of this article are those of the authors and do not necessarily reflect the views or policy of the Department of the Navy, the Department of Defense, the U.S. government, or Naval Medical Center San Diego.
