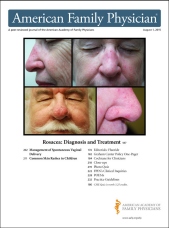
Am Fam Physician. 2015;92(3):211-216
Author disclosure: No relevant financial affiliations.
Because childhood rashes may be difficult to differentiate by appearance alone, it is important to consider the entire clinical presentation to help make the appropriate diagnosis. Considerations include the appearance and location of the rash; the clinical course; and associated symptoms, such as pruritus or fever. A fever is likely to occur with roseola, erythema infectiosum (fifth disease), and scarlet fever. Pruritus sometimes occurs with atopic dermatitis, pityriasis rosea, erythema infectiosum, molluscum contagiosum, and tinea infection. The key feature of roseola is a rash presenting after resolution of a high fever, whereas the distinguishing features in pityriasis rosea are a herald patch and a bilateral and symmetric rash in a Christmas tree pattern. The rash associated with scarlet fever usually develops on the upper trunk, then spreads throughout the body, sparing the palms and soles. Impetigo is a superficial bacterial infection that most commonly affects the face and extremities of children. Erythema infectiosum is characterized by a viral prodrome followed by the “slapped cheek” facial rash. Flesh-colored or pearly white papules with central umbilication occur with molluscum contagiosum, a highly contagious viral infection that usually resolves without intervention. Tinea is a common fungal skin infection in children that affects the scalp, body, groin, feet, hands, or nails. Atopic dermatitis is a chronic, relapsing inflammatory skin condition that may present with a variety of skin changes.
There are more than 12 million office visits annually for rashes and other skin concerns in children and adolescents, of which 68% are made to primary care physicians.1 Recognizing key features can help distinguish the different types of rashes (Table 1). This article includes common infectious and noninfectious inflammatory rashes in children.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Potassium hydroxide testing can be a helpful diagnostic tool to distinguish pityriasis rosea from tinea or other rashes with a scale. | C | 6 |
| Pityriasis rosea usually resolves spontaneously in two to 12 weeks without active treatment. | C | 6 |
| Rapid antigen tests have a sensitivity of 86% for diagnosing group A beta-hemolytic streptococcal pharyngitis. | C | 10 |
| Although impetigo is often self-limited, antibiotics are commonly prescribed to prevent complications and spread of the infection. | C | 12 |
| The use of emollients is recommended for children with atopic dermatitis. | C | 16 |
| Atopic lesions that do not respond to traditional therapies should be biopsied or cultured if there is concern for infection. | C | 16 |
| Recommendation | Sponsoring organization |
|---|---|
| Do not use oral antibiotics for atopic dermatitis unless there is clinical evidence of infection. | American Academy of Dermatology |
| Condition | Location | Appearance | Fever | Pruritus | Distinguishing features | Duration |
|---|---|---|---|---|---|---|
| Roseola infantum (exanthema subitum) | Trunk, spreads peripherally | Macular to maculopapular | High fever, usually greater than 102°F (39°C), precedes the rash; child is otherwise well-appearing | No | Can be confused with measles; measles rash begins on the face, and the child is usually ill-appearing | 1 to 2 days |
| Pityriasis rosea | Trunk, bilateral and symmetric, Christmas tree distribution | Herald patch on the trunk may present first, followed by smaller similar lesions; oval-shaped, rose-colored patches with slight scale | No | Occurs in up to one-half of patients | Often confused with tinea corporis; pityriasis rosea is typically widespread, whereas tinea corporis usually causes a single lesion | 2 to 12 weeks |
| Scarlet fever | Upper trunk, spreads throughout body, spares palms and soles | Erythematous, blanching, fine macules, resembling a sunburn; sandpaper-like papules | Occurs 1 to 2 days before rash develops | Usually no | Petechiae on palate; white strawberry tongue; test positive for streptococcal infection | Several weeks |
| Impetigo | Anywhere; face and extremities are most common | Vesicles or pustules that form a thick, yellow crust | Usually no | No | May be a primary or secondary infection; bullous form is typical in neonates, and nonbullous form is more common in preschool- and school-aged children | Usually self-limited but often treated to prevent complications and spread of the infection |
| Erythema infectiosum (fifth disease) | Face and thighs | Erythematous “slapped cheek” rash followed by pink papules and macules in a lacy, reticular pattern | Low grade | Yes | May be confused with scarlet fever; the slapped cheek rash can differentiate erythema infectiosum | Facial rash lasts 2 to 4 days; lacy, reticular rash may last 1 to 6 weeks |
| Molluscum contagiosum | Anywhere; rarely on oral mucosa | Flesh-colored or pearly white, small papules with central umbilication | No | Yes, if associated with dermatitis | Usually resolves spontaneously without treatment | Months or up to 2 to 4 years |
| Tinea infection | Anywhere | Alopecia or broken hair follicles on the scalp (tinea capitis), erythematous annular patch or plaque with a raised border and central clearing on the body (tinea corporis) | No | Yes | Often confused with pityriasis rosea; potassium hydroxide microscopy can help confirm diagnosis | Usually requires antifungal treatment |
| Atopic dermatitis | Extensor surfaces of extremities, cheeks, and scalp in infants and younger children; flexor surfaces in older children | Erythematous plaques, excoriation, severely dry skin, scaling, vesicular lesions | No | Yes | Emollients and avoidance of triggers are the mainstay of treatment; topical corticosteroids may be needed for flare-ups | Chronic, relapsing |
History and Physical Examination
The initial approach to a child with a rash begins with the history, which should include the duration of the rash, the initial appearance and how it has evolved, the location, and any treatments that have been used. Parents should also be asked if other household members have a similar rash and if there have been any new medication, product, or environmental exposures. The presence or absence of associated symptoms can help clinicians develop a differential diagnosis. A fever is likely with roseola, erythema infectiosum, and scarlet fever. Pruritus sometimes occurs with atopic dermatitis, pityriasis rosea, erythema infectiosum, molluscum contagiosum, and tinea infection.
On physical examination, certain clinical findings may be useful in determining a diagnosis. It is important to determine the type of lesions, such as macules, papules, vesicles, plaques, or pustules. Other important characteristics include location and distribution, arrangement, shape, color, and presence or absence of scale.
Roseola Infantum (Exanthema Subitum)
Roseola is most commonly caused by human herpesvirus 6 and affects infants and children younger than three years.2 It is characterized by the abrupt onset of high fever lasting one to five days. During this period, children often appear well with no focal clinical signs except possible mild cough, rhinorrhea, or mild diarrhea. Once the fever resolves, an erythematous macular to maculopapular rash usually appears, starting on the trunk and spreading peripherally. This rash is similar in appearance to that of rubeola (measles). In contrast with roseola, the rash associated with measles starts on the face (usually behind the ear) or mouth (Koplik spots) and moves downward.3 Children with roseola usually appear well, whereas those with measles are typically more ill-appearing. Roseola is a self-limited illness requiring no treatment, and the diagnosis is clinical.4
Pityriasis Rosea
Approximately 80% of patients with pityriasis rosea present with a single oval-shaped, rose-colored patch, usually on the trunk. This lesion, commonly known as the herald patch, is typically 2 to 10 cm in diameter and may have a peripheral scale5 (Figure 1). It may be present for a few weeks before the development of smaller lesions that are similar to the herald patch, maintaining a classic peripheral scale overlying pink thin papules.

The herald patch may be misdiagnosed as tinea corporis because of the annular lesion with raised edges, fine scale, and central clearing. There is usually a single plaque with tinea corporis, without eruptions of smaller lesions typical with pityriasis rosea. The rash of pityriasis rosea is usually bilateral and symmetric, distributed parallel to the Langer lines in a Christmas tree pattern. Children with pityriasis rosea may have a history of mild upper respiratory tract infection symptoms, and up to one-half have pruritus.6 A potassium hydroxide preparation can help distinguish pityriasis rosea from tinea infection or other rashes. The rash associated with pityriasis rosea may be present for two to 12 weeks, and treatment is supportive.6 Although the etiology is not fully known, it is thought to be infectious, with some studies implicating human herpesvirus 6 and 7.5,7
Scarlet Fever
Scarlet fever is diagnosed in 10% of children presenting with streptococcal tonsillopharyngitis.8 It is caused by certain strains of group A beta-hemolytic streptococci that release a streptococcal pyrogenic exotoxin (erythrogenic toxin). Patients who have a hypersensitivity to the toxin may develop the characteristic rash associated with scarlet fever.
Most children have a fever and sore throat one to two days before the rash develops on the upper trunk. The rash spreads throughout the body, sparing the palms and soles, with characteristic circumoral pallor. This differs from some viral exanthems that develop more slowly. The rash is characterized by confluent, erythematous, blanching, fine macules, resembling a sunburn, and sandpaper-like papules (Figure 2). In skinfolds, such as the axilla, antecubital fossa, and buttock creases, an erythematous, nonblanching linear eruption (Pastia lines) may develop. Petechiae on the palate may occur, as well as erythematous, swollen papillae with a white coating on the tongue (white strawberry tongue). Red strawberry tongue occurs after desquamation of the white coating. After several weeks, the rash fades and is followed by desquamation of the skin, especially on the face, in skin-folds, and on the hands and feet, potentially lasting four to six weeks.9

With a sensitivity of 90% to 95%, throat culture is the first-choice method for diagnosis of group A streptococcal infection, but this is not always practical.8 Rapid antigen tests are routinely used in clinicians' offices and have a sensitivity of approximately 86%.10 Cultures may be ordered when the suspicion for group A streptococcal infection is high, but the rapid antigen test result is negative.11
Penicillin is the therapy of choice for streptococcal infection. Those allergic to penicillin and cephalosporins may be treated with oral macrolides (erythromycin, azithromycin [Zithromax]) or clindamycin.10.
Impetigo
Impetigo is a primary or secondary bacterial infection of the epidermis of the skin. Primary infections occur when bacteria enter breaks in the skin, whereas secondary infections develop at the site of an existing dermatosis. There are bullous and nonbullous forms of the infection, with the bullous form typically occurring in neonates and the nonbullous form most common in preschool- and school-aged children.12 Although Streptococcus pyogenes was once the most common cause of nonbullous impetigo, Staphylococcus aureus has surpassed it in more recent years. However, S. pyogenes may still be the predominant cause in warm and humid climates. S. aureus is the main source of bullous impetigo. Initially, children may develop vesicles or pustules that form a thick, yellow crust (Figure 3). With autoinoculation, the lesions may quickly spread. The face and extremities are most commonly affected. Although impetigo is usually a self-limited disease, antibiotics are often prescribed to prevent complications and spread of the infection.12

Erythema Infectiosum
Erythema infectiosum, or fifth disease, is caused by parvovirus B19. It is a common childhood infection characterized by a prodrome of low-grade fever, malaise, sore throat, headache, and nausea followed several days later by an erythematous “slapped cheek” facial rash (Figure 4). After two to four days, the facial rash fades. In the second stage of the disease process, pink patches and macules may develop in a lacy, reticular pattern, most often on the extremities. After one to six weeks, the rash resolves but may reappear with sun exposure, heat, or stress. Arthralgias occur in approximately 8% of young children with the disease but are much more common in teens and young adults. Patients are no longer considered infectious once the rash appears. Treatment is symptomatic and includes nonsteroidal anti-inflammatory drugs for arthralgias and antihistamines for pruritus.13

Molluscum Contagiosum
Molluscum contagiosum is a skin infection caused by a poxvirus. This highly contagious viral infection most commonly affects children two to 11 years of age.14 It also occurs in sexually active adolescents. The lesions are flesh-colored or pearly white, small papules with central umbilication (Figure 5). The oral mucosa is rarely affected, but lesions may appear on the genital region and conjunctiva. Typically, children have 10 to 20 lesions, but occasionally there may be up to hundreds.14 Molluscum may also occur in conjunction with dermatitis. It can erupt and spread quickly in a child with underlying atopic dermatitis, or it can induce dermatitis in a child with previously clear skin (molluscum dermatitis).

The diagnosis of molluscum contagiosum is made clinically. The condition is self-limited, but clinicians should advise parents to use gentle skin care products on the patient and that lesions may last for months or up to two to four years. Treatment options, including cryotherapy, imiquimod (Aldara), and intralesional immunotherapy, are available if physical appearance is a concern. Dermatitis (occurring as molluscum dermatitis or a flare-up of atopic dermatitis) requires treatment to resolve pruritus and limit spread of the molluscum.14
Tinea Infection
Tinea is a common fungal skin infection in children that may affect the scalp (tinea capitis), body (tinea corporis), groin (tinea cruris), feet (tinea pedis), hands (tinea manus), or nails (tinea unguium). The diagnosis is based on physical examination findings and is confirmed by potassium hydroxide microscopy, periodic acid–Schiff staining of hair follicles, or fungal culture.
Tinea capitis, the most common skin infection in children in the United States, is characterized by scaling or circumscribed alopecia and broken hair follicles (Figure 6). Posterior cervical lymphadenopathy is another useful finding to distinguish tinea capitis from other causes of alopecia. The characteristic lesion found in children with tinea corporis is an erythematous annular patch or plaque with a raised border and central clearing; scaling along the border is common (Figure 7). This lesion is often referred to as ringworm.15 Tinea capitis is treated with oral griseofulvin and terbinafine (Lamisil), depending on the most common etiologic agent in the geographic area. Tinea corporis is usually effectively treated with topical antifungals, with oral agents reserved for severe cases.15


Atopic Dermatitis
Atopic dermatitis is a common childhood inflammatory skin disease that affects approximately 20% of children in the United States.16 This chronic, pruritic skin disease is relapsing in nature. Atopic dermatitis typically presents in infancy and early childhood and may persist into adulthood. Children may present with a variety of skin changes, including erythematous plaques and papules, excoriations, severely dry skin, scaling, and vesicular lesions (Figure 8).

The distribution of atopic dermatitis lesions can vary based on the age of the child. Infants and younger children often have lesions on the extensor surfaces of extremities, cheeks, and scalp. Older children and adults often present with patches and plaques on the flexor surfaces (antecubital and popliteal fossa). Hands and feet are also commonly affected. Thickened plaques with a lichenified appearance may be seen in more severe cases. Children with atopic dermatitis often have dry, flaky skin and are at risk of secondary cutaneous infections.16 The treatment is aimed at controlling, not curing, the disease with parent counseling on good skin care (e.g., liberal use of emollients and avoidance of triggers, such as cold weather, frequent hot baths, fragrant products, and harsh detergents). Despite good skin care practices, topical corticosteroids are usually needed during flare-ups. Atopic lesions that do not respond to traditional therapies should be biopsied or cultured if there is concern for infection.16
Data Sources: We searched MEDLINE, MEDLINE In-Process, Cochrane Database of Systematic Reviews, Clinical Evidence, DynaMed, Essential Evidence Plus, ClinicalKey, and the National Guideline Clearinghouse. Retrieval was limited to English, all child (0 to 18 years), or pediatric terms. Keywords were atopic dermatitis, erythema infectiosum, exanthema subitum, impetigo, pityriasis rosea, Roseolovirus infections, scarlet fever, tinea, onychomycosis, tinea capitis, tinea favosa, tinea pedis, molluscum contagiosum. We emphasized evidence-based outcomes, including randomized and nonrandomized clinical trials, systematic reviews, meta-analyses, comparative studies, and guidelines. Search dates: June and October 2014, and May 2015.
The authors thank Susan Meadows and Susan Elliott for assistance with the literature search.