
Am Fam Physician. 2015;92(9):807-812
Patient information: See related handout on cognitive behavior therapy, written by the authors of this article.
Author disclosure: No relevant financial affiliations.
Cognitive behavior therapy (CBT) is a time-limited, goal-oriented psychotherapy that has been extensively researched and has benefits in a number of psychiatric disorders, including anxiety, depression, posttraumatic stress disorder, attention-deficit/hyperactivity disorder, autism, obsessive-compulsive and tic disorders, personality disorders, eating disorders, and insomnia. CBT uses targeted strategies to help patients adopt more adaptive patterns of thinking and behaving, which leads to positive changes in emotions and decreased functional impairments. Strategies include identifying and challenging problematic thoughts and beliefs, scheduling pleasant activities to increase environmental reinforcement, and extended exposure to unpleasant thoughts, situations, or physiologic sensations to decrease avoidance and arousal associated with anxiety-eliciting stimuli. CBT can be helpful in the treatment of posttraumatic stress disorder by emphasizing safety, trust, control, esteem, and intimacy. Prolonged exposure therapy is a CBT technique that includes a variety of strategies, such as repeated recounting of the trauma and exposure to feared real-world situations. For attention-deficit/hyperactivity disorder, CBT focuses on establishing structures and routines, and clear rules and expectations within the home and classroom. Early intensive behavioral interventions should be initiated in children with autism before three years of age; therapy consists of 12 to 40 hours of intensive treatment per week, for at least one year. In many disorders, CBT can be used alone or in combination with medications. However, CBT requires a significant commitment from patients. Family physicians are well suited to provide collaborative care for patients with psychiatric disorders, in concert with cognitive behavior therapists.
Cognitive behavior therapy (CBT) is a group of time-limited, goal-oriented psychotherapies that have been extensively researched for the treatment of psychiatric disorders. CBT targets changes in symptoms of psychiatric disorders to reduce functional impairments and improve patients' overall quality of life. This article aims to provide a concise overview of CBT, including the types of disorders it can treat, how it can be combined with pharmacotherapy, and how family physicians can use CBT principles in their practice.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| CBT is an effective treatment for mild to moderate depression, anxiety disorders, posttraumatic stress disorder, obsessive-compulsive and tic disorders, autism, eating disorders, personality disorders, insomnia, and attention-deficit/hyperactivity disorder. | A | 1–18, 34–37 |
| Psychiatric medications are the primary treatment for schizophrenia and bipolar disorder, but CBT provides additional benefits. | B | 22, 23 |
| For many psychiatric conditions, CBT provides similar outcomes or additional benefits compared with psychiatric medications alone. | A | 5, 9–11, 18, 20, 22, 24–27 |
| Benzodiazepine use should be avoided in patients who are receiving CBT because it can interfere with exposure therapy. | C | 38–41 |
| Recommendation | Sponsoring organization |
|---|---|
| Avoid use of hypnotics as primary therapy for chronic insomnia in adults; instead, offer cognitive behavior therapy, and reserve medication for adjunctive treatment when necessary. | American Academy of Sleep Medicine |
| Do not prescribe medication to treat childhood insomnia, which usually arises from parent-child interactions and responds to behavioral intervention. | American Academy of Sleep Medicine |
Which Patients Benefit from CBT?
CBT is effective for the treatment of anxiety, depression, posttraumatic stress disorder (PTSD), attention-deficit/hyperactivity disorder (ADHD), autism, obsessive-compulsive and tic disorders, personality disorders, eating disorders, and insomnia. CBT-based treatments for specific disorders are available at http://www.abct.org/Information/?m=mInformation&fa=FactSheets.
EVIDENCE SUMMARY
CBT effectively targets symptoms of anxiety,1–4 depression,5–7 PTSD,8,9 ADHD,10,11 autism,12,13 obsessive-compulsive and tic disorders,14 personality disorders,15,16 eating disorders,17 and insomnia18 in children, adolescents, and adults. Numerous meta-analyses and reviews have demonstrated that CBT reduces psychiatric symptoms and functional impairments, and improves quality of life.1–18 The American Psychological Association lists CBT as an effective treatment for numerous disorders.19 Moreover, CBT has been shown to be as effective as or more effective than medications for depression, anxiety, and trauma-related disorders,5,9,20–29 and it is a useful adjunctive therapy for disorders such as ADHD, schizophrenia, and bipolar disorder.10–12,22,23
How Does CBT Work?
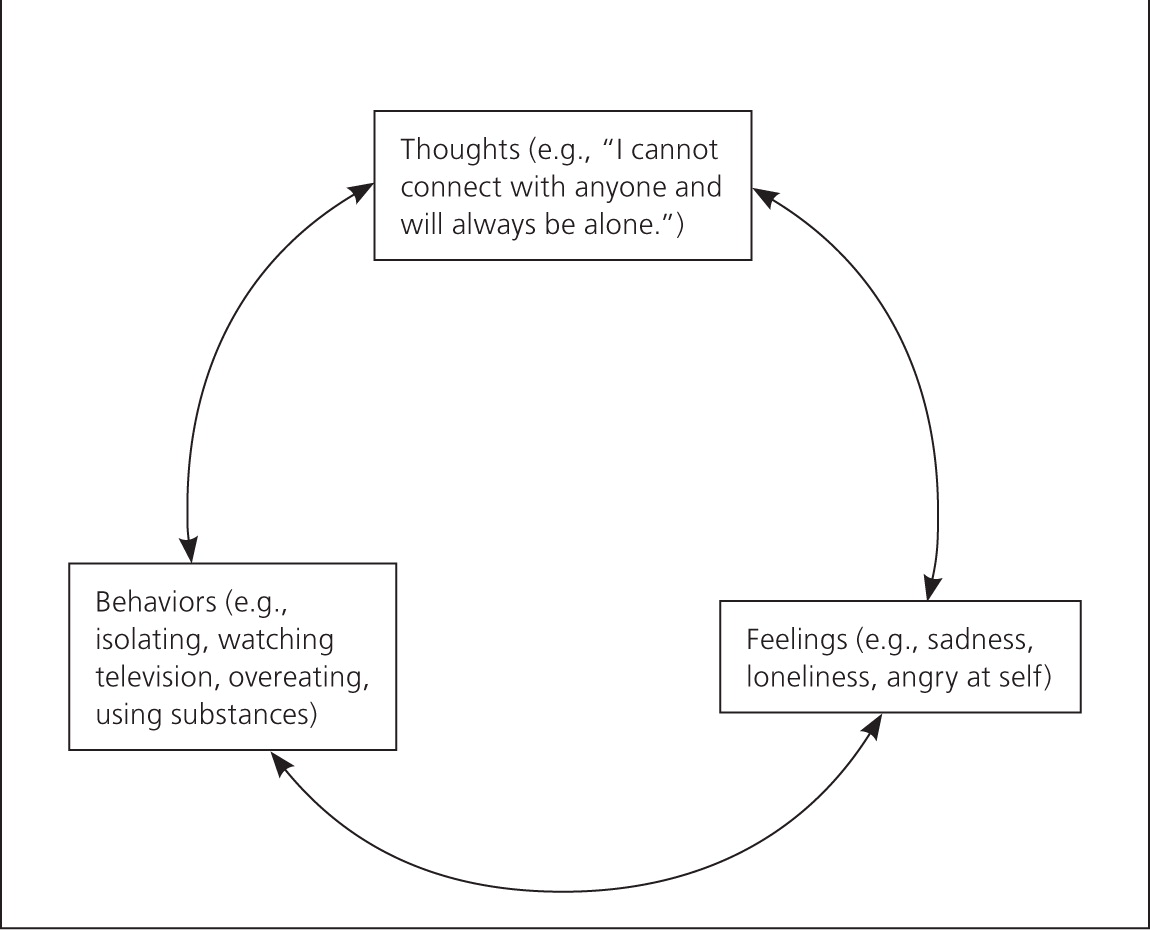
According to the cognitive behavioral model, psychopathology occurs because of problematic patterns in thinking and behavior that lead to difficult emotions and functional impairments (Figure 1). The aim of CBT is to help patients adopt more adaptive patterns of thinking and behavior to improve function and quality of life. Treatment goals are selected collaboratively with patients to determine whether progress is being made. CBT involves three core strategies applied alone or in combination, depending on the patients' needs: (1) identifying and challenging problematic thoughts and beliefs, with the goal of helping patients develop more realistic and adaptive thoughts and beliefs, (2) scheduling pleasant activities to increase environmental reinforcement, and (3) extended exposure to unpleasant thoughts, situations, or physiologic sensations to decrease avoidance and arousal associated with anxiety-eliciting stimuli.30
EVIDENCE SUMMARY
How Does CBT Improve Depression?
A cognitive behavior therapist whose patient feels sad and hopeless might choose to target the patient's maladaptive thoughts (“I cannot connect with anyone.”) or behaviors (isolating and watching television). Targeting changes in either domain leads to changes in the other and in the patient's emotions.5,6 For example, the therapist might challenge the patient's thoughts by eliciting examples of occasions when the patient was able to positively engage with others. This could cause the patient to feel less hopeless as he or she realizes that the thought was not accurate, and to call a friend to reconnect. Alternatively, the therapist could attempt to change the maladaptive behaviors by helping the patient schedule pleasant activities consistent with his or her values (calling a friend). This reconnection could boost the patient's mood and change the belief that he or she will always be alone. Although these examples misrepresent the amount of therapeutic work needed to change entrenched patterns of thoughts and behaviors, they give a sense of what the therapeutic process might involve.
EVIDENCE SUMMARY
CBT can be used to reduce symptoms of depression, with or without medication.5–7,20–29,31–33 Although treatment guidelines from the American Psychiatric Association suggest that medication should be used as a first-line treatment for depression, CBT should also be considered. Evidence has shown that CBT and paroxetine (Paxil) produce equivalent outcomes in patients with severe depression.34 Thus, family physicians must use their clinical judgment in determining which treatments to suggest for their patients.
How Does CBT Improve Anxiety and Trauma-Related Disorders?
Similar to the example above, therapists who are treating patients with anxiety and trauma-related disorders challenge problematic patterns of thoughts or behaviors. A more thorough description of CBT for PTSD is provided here as an example.
Evidence-based therapies for PTSD in adults include cognitive processing therapy and prolonged exposure therapy, whereas trauma-focused CBT is used in younger patients. Cognitive processing therapy includes psychoeducation about PTSD and focuses on challenging maladaptive thoughts and beliefs about safety, trust, control, esteem, and intimacy.35 Prolonged exposure therapy includes psychoeducation about PTSD, breathing retraining to decrease arousal, repeated recounting of the trauma to teach patients that the memories are not dangerous and do not need to be avoided, and in vivo exposure to feared real-world situations.8,9 In younger patients, trauma-focused CBT includes components similar to those for prolonged exposure and cognitive processing therapies, but also includes parallel and joint parental sessions.36
EVIDENCE SUMMARY
Is CBT Different When Used in Children vs. Adults?
Parental involvement in therapy is necessary when children receive CBT. Parents can ensure that their child engages in behavioral exercises between therapy sessions (e.g., in vivo exposures, pleasant activities), can change the child's environment to promote more effective behaviors, and can help the child target changes in maladaptive thoughts. In general, CBT for children focuses more on behavior changes and less on cognitive changes. Behavioral techniques used for children with ADHD and autism are described below.
ADHD
A recent review showed that behavioral parent training, behavioral classroom management, and behavioral peer interventions are well-established treatments for ADHD.11 Behavioral parent training and behavioral classroom management focus on strategies implemented by adults to help children with ADHD function more effectively, including creating structure and routines, setting clear rules and expectations, using effective commands, and rewarding or punishing the child based on his or her compliance. These techniques help reduce behavioral problems experienced by children with ADHD and decrease the need for polypharmacy to manage symptoms.11
AUTISM
Early intensive behavioral interventions are the only evidence-based treatment that confers significant benefits in children with autism.12 These interventions should be initiated before three years of age and often consist of 12 to 40 hours of intensive treatment per week, for at least one year. Parents and therapists engage in intensive exercises focused on reinforcing and rewarding adaptive behaviors. Behavioral treatments for autism produce significant improvements in IQ and adaptive behaviors.13
EVIDENCE SUMMARY
Is CBT Effective for Other Disorders?
CBT has been examined and tested across a wide range of psychiatric disorders. In addition, it has been examined as an adjunctive treatment for medical problems in which behavior change could enhance outcomes.
EVIDENCE SUMMARY
Although a thorough discussion of the effectiveness of CBT for all psychiatric disorders is beyond the scope of this article, it has been shown to have significant benefits for patients with insomnia,18 psychosis,23 bipolar disorder,22 eating disorders,17 and personality disorders.15,16 Family physicians are encouraged to seek adjunctive CBT for patients diagnosed with these disorders.
When Can CBT Be Combined with Medications?
CBT can be used alone or in combination with medications for a variety of psychiatric disorders. Medications can be used to stabilize patients and promote recovery, whereas CBT can be used to encourage long-term changes in thoughts and behaviors.
EVIDENCE SUMMARY
CBT generally produces equivalent outcomes or provides additional benefits compared with the use of psychiatric medications alone.5,9,12,20–23,26,34 Moreover, CBT is often more cost-effective, has more enduring effects,9,21–23,27,28 and lacks the adverse effects associated with many psychiatric medications. The effects of CBT are reduced in patients who are receiving benzodiazepines38–40; therefore, these medications should be avoided in patients with anxiety and trauma-related disorders. Although a combination of CBT and benzodiazepines may initially seem beneficial (e.g., reduced arousal, improved sleep), this approach may actually limit the gains made with CBT (e.g., patients may not be able to engage in exposure exercises when arousal is reduced as a result of medication use).38,41
What Are the Potential Limitations of CBT?
CBT is most effective when patients complete therapeutic exercises outside of the treatment session; therefore, it requires a significant commitment from patients. Some of the therapeutic strategies may involve anxiety-eliciting stimuli, which can be distressing—although short-lived—for some patients. The structured nature of CBT is not a good fit for patients who are seeking insight into the underlying causes of their distress. Lastly, CBT is not a substitute for pharmacotherapy for some disorders. For example, CBT should be considered an adjunctive treatment in the management of bipolar disorder, psychotic disorders, and depression with psychotic features.
How Can Family Physicians Integrate CBT into Practice and Provide Referrals to Effective Therapists?
When discussing psychiatric disorders with patients, family physicians are well suited to help patients decide which services to seek. In addition to asking about patients' personal and family histories of psychiatric disorders, family physicians can help patients identify thoughts and behaviors that are contributing to their problems. For example, avoidance behaviors (e.g., avoiding crowded stores, avoiding interacting with the opposite sex) help maintain anxiety disorders and PTSD. Family physicians can encourage patients to face safe stimuli and, if possible, seek safe fear-eliciting stimuli. For patients with depressive symptoms, encouraging engagement in a daily pleasant activity is helpful.32
Family physicians are on the front line when it comes to treatments for psychiatric disorders and can be influential when recommending treatments to their patients. Building a collaborative relationship with community-based behavior therapists enables family physicians to provide comprehensive care. Table 1 provides resources for CBT, including websites for locating therapists and information to help patients select a therapist. For patients who are already engaged in therapy, family physicians can help determine whether they would benefit from CBT, especially if the alternative is a potentially longer-term, less cost-effective form of psychotherapy. Table 2 lists key features of CBT that physicians can incorporate into discussions to optimize their patients' care.
| Academy of Cognitive Therapy – Therapist locator | |
| http://www.academyofct.org | |
| American Psychological Association – Therapist locator | |
| http://locator.apa.org/ | |
| Association for Behavioral and Cognitive Therapies | |
| http://www.abct.org/Information/?m=mInformation&fa=FactSheets, http://www.abct.org/information/?m=mInformation&fa=fs_GUIDELINES_CHOOSING, and http://www.abctcentral.org/xFAT/ | |
| Psychology Today – Therapist locator | |
| https://therapists.psychologytoday.com/rms/prof_search.php | |
| One 60- to 90-minute session per week, typically for eight to 12 weeks |
| Symptom measures are collected frequently |
| Treatment is goal-oriented and collaborative; patient is expected to be an active participant |
| Treatment is focused on changing current problematic or maladaptive thoughts or behaviors |
| Weekly homework assignments |
Data Sources: A PsycINFO search was completed using the key terms cognitive behavioral therapy, cognitive therapy, and behavior therapy. The search included meta-analyses, randomized controlled trials, clinical trials, and reviews. Search dates: October and November 2014. In addition, we used an evidence summary from Essential Evidence Plus.
