Am Fam Physician. 2015;92(11):1017-1018
Author disclosure: No relevant financial affiliations.
A 29-year-old woman delivered at 39 weeks' gestation by elective repeat cesarean delivery. After this delivery, she was gravida 3, para 2, aborta 1. There was a nuchal cord during delivery, but the newborn had Apgar scores of 8 and 9. The pregnancy was complicated by the mother's obesity and rubella nonimmune status. Her blood type was O Rh-positive.
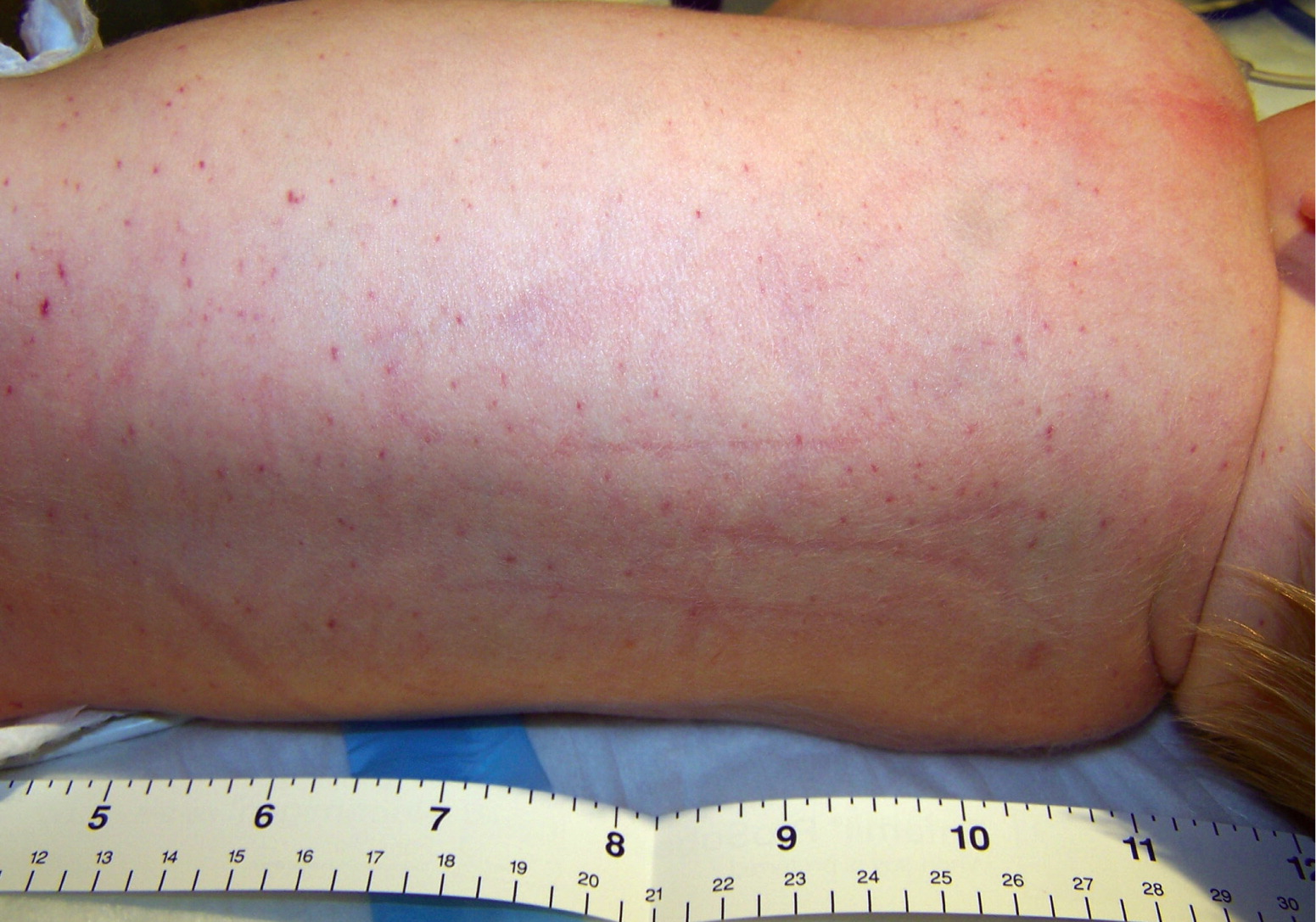
Findings on the initial newborn examination were normal, with a weight of 3,745 g (8 lb, 4 oz) and normal vital signs. However, at five hours of life, scattered petechiae had developed over his trunk and extremities (Figure 1). A complete blood count showed a normal white blood cell count and hemoglobin level. The platelet count was abnormal at 14 × 103 per μL (14 × 109 per L). His blood type was O Rh-positive, and results of a direct antiglobulin test (Coombs test) were negative. His blood glucose level was normal. Maternal testing for anti-human platelet antigen 1a antibodies was positive with a normal platelet count.
Question
Discussion
The answer is C: neonatal alloimmune thrombocytopenia. This condition occurs when the mother develops immunoglobulin G antibodies to an antigen expressed on the fetal platelet that she does not possess. In whites, 80% to 90% of cases are caused by human platelet antigen 1a.1 The onset may occur in utero or in the first 72 hours of life.2 One-half of cases occur in the first pregnancy, and the prevalence is estimated to be 0.5 to 2 cases per 1,000 deliveries.3
The clinical presentation is typically petechiae with or without ecchymosis, and may include visceral bleeding, bleeding after a circumcision, or sometimes intracranial hemorrhage.3 The diagnosis is made by testing for maternal alloantibodies.4 Treatment strategies for the newborn may include transfusion of platelets (for platelet counts less than 30 × 103 per μL [30 × 109 per L]), intravenous immune globulin, and corticosteroids.2,5 The newborn should be screened for intracranial hemorrhage with ultrasonography of the head.2 Subsequent pregnancies should be monitored closely because more severe thrombocytopenia is likely; treatment consists of maternal administration of intravenous immune globulin, corticosteroids, fetal platelet transfusion, and cesarean delivery two to four weeks before term.4,6
Maternal immune thrombocytopenic purpura can cause neonatal thrombocytopenia by transplacental transfer of maternal antiplatelet antibodies. Approximately 9% of children born to mothers with immune thrombocytopenic purpura will have platelet counts less than 50 × 103 per μL (50 × 109 per L).2 The condition causes early onset of multiple petechiae in the newborn that self resolve. The lack of maternal immune thrombocytopenia and a normal maternal platelet count effectively rule it out as the source of a newborn's thrombocytopenia.
Kasabach-Merritt syndrome is a rare syndrome that presents with kaposiform or tufted hemangiomas in the skin or solid organs and is associated with thrombocytopenia. It is apparent at birth or during early infancy. The lack of an obvious vascular malformation on the initial physical examination significantly diminishes the possibility of Kasabach-Merritt syndrome.
Perinatal infections such as group B streptococcus, Escherichia coli, or Haemophilus influenzae can cause thrombocytopenia in newborns. However, it is more likely to develop after 72 hours of life and is associated with other clinical signs such as fever, hypothermia, leukocytosis, or neutropenia.2 Delaying antibiotics in a septic newborn is associated with a poor prognosis; therefore, antibiotics are initiated pending results of blood cultures.
Thrombocytopenia can be associated with RhD alloimmunization. However, platelets do not express the RhD antigen and are not directly affected by maternal RhD antibodies. When thrombocytopenia is associated with RhD alloimmunization, it usually occurs with fetal hydrops and has a poor prognosis.7 In our case, the newborn has the same blood type as his mother and the Coombs test result is negative, ruling out this condition.
| Condition | Characteristics |
|---|---|
| Immune thrombocytopenic purpura | Multiple petechiae, early onset, self-resolving; maternal immune thrombocytopenia |
| Kasabach-Merritt syndrome | Syndrome of kaposiform or tufted hemangiomas of the skin or solid organs; associated with thrombocytopenia |
| Neonatal alloimmune thrombocytopenia | Early-onset petechiae with or without ecchymosis; visceral bleeding, bleeding after a circumcision, or sometimes intracranial hemorrhage; normally no maternal thrombocytopenia |
| Perinatal infection | Rapid development of thrombocytopenia, usually after 72 hours of life; presents with other clinical signs such as fever, hypothermia, leukocytosis, or neutropenia |
| RhD alloimmunization | Maternofetal Rh incompatibility, positive findings on direct antiglobulin test (Coombs test), fetal hydrops |
The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, or the U.S. government.