A more recent article on systemic lupus erythematosus is available.
Am Fam Physician. 2016;94(4):284-294
Patient information: See related handout on lupus, written by the authors of this article.
Related Close-Up: Joint Pain and Fatigue: It Could Be Anything.
Author disclosure: No relevant financial affiliations.
Systemic lupus erythematosus is an autoimmune disease that affects many systems, including the skin, musculoskeletal, renal, neuropsychiatric, hematologic, cardiovascular, pulmonary, and reproductive systems. Family physicians should be familiar with the manifestations of lupus to aid in early diagnosis, monitoring patients with mild disease, recognizing warning signs that require referral to a rheumatologist, and helping to monitor disease activity and treatment in patients with moderate to severe disease. The American College of Rheumatology has 11 classification criteria for lupus. If a patient meets at least four criteria, lupus can be diagnosed with 95% specificity and 85% sensitivity. All patients with lupus should receive education, counseling, and support. Hydroxychloroquine is the cornerstone of treatment because it reduces disease flares and other constitutional symptoms. Low-dose glucocorticoids can be used to treat most manifestations of lupus. The use of immunosuppressive and cytotoxic agents depends on the body systems affected. Patients with mild disease that does not involve major organ systems can be monitored by their family physician. Patients with increased disease activity, complications, or adverse effects from treatment should be referred to a rheumatologist. To optimize treatment, it is important that a rheumatologist coordinate closely with the patient's family physician to improve chronic care as well as preventive health services.
Systemic lupus erythematosus (SLE) is an autoimmune disease that affects the skin and musculoskeletal, renal, neuropsychiatric, hematologic, cardiovascular, pulmonary, and reproductive systems. Its course is typically recurrent, with periods of relative remission followed by flares. SLE can be fatal and significantly increases the risk of cardiovascular disease.
| Recommendation | Sponsoring organization |
|---|---|
| Do not test antinuclear antibodies (ANA) subserologies without a positive ANA and clinical suspicion of immune-mediated disease. | American College of Rheumatology |
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| The initial evaluation for suspected SLE should include an antinuclear antibody test. | C | 15 |
| Patients diagnosed with SLE must meet at least four of the 11 American College of Rheumatology diagnostic criteria. | C | 8 |
| Treatment of mild SLE includes patient education, expectations of treatment, and counseling to avoid extensive ultraviolet light exposure and overexertion. | C | 8 |
| Hydroxychloroquine (Plaquenil) has been shown to reduce arthritis pain associated with SLE. | A | 32 |
| A combination of glucocorticoid plus immunosuppressant is more effective than glucocorticoids alone in preserving renal function in patients with SLE. | A | 32 |
| A combination of glucocorticoid and mycophenolate (Cellcept) or cyclophosphamide is effective in achieving remission in patients with SLE nephritis. | A | 28 |
SLE affects about 300,000 persons in the United States.1 It is twice as prevalent in black persons as in white persons, and it is 10 times more common in females than in males.2 Over the past decade, the five-year survival rate of patients with SLE has improved to more than 95% because of more effective recognition and treatment of infectious and renal complications.3,4 Because patients with SLE are living longer, the focus of care should be comprehensive, including preventive services in addition to treatment.5
Role of the Primary Care Physician
A qualitative study in the United Kingdom noted a lack of detailed knowledge about SLE by family physicians and the need for more cohesive health care.6 There is a need for well-coordinated, multidisciplinary health care teams including subspecialists and family physicians to improve chronic care and preventive health services for these patients.7
A committee of the American College of Rheumatology (ACR) recommended that the role of primary care physicians is understanding the manifestations of SLE to aid in early diagnosis, treating and monitoring patients with mild disease, recognizing warning signs to refer to a rheumatologist appropriately, and helping to monitor disease activity and treatment in patients with moderate to severe disease.8
Diagnosis
SLE is difficult to diagnose in primary care because many of the symptoms (e.g., fatigue, rash, joint pain) are nonspecific and overlap with those of more common conditions. Furthermore, biomarkers are often negative or normal early in the course of the illness. The most common presenting symptoms are constitutional, such as fatigue, weight loss, and fever without a focal infection, occurring in up to 90% of patients.9 Other common presenting symptoms include arthralgia and myalgia, which occur in up to 95% of patients with SLE.10 Less common presenting symptoms include malar rash (31%), photosensitivity (23%), pleuritic chest pain (16%), new-onset Raynaud phenomenon (16%), and mouth sores (12.5%).11
| Differential diagnosis | Distinguishing features | Diagnostic approach |
|---|---|---|
| Adult-onset Still disease | Arthralgia, fever, lymphadenopathy, splenomegaly | Tests for elevated ESR, leukocytosis, and anemia |
| Behçet syndrome | Aphthous ulcers, arthralgia, uveitis | Recurrent oral ulcers plus two of the following: eye lesions, genital ulcers, skin lesions |
| Chronic fatigue syndrome | Persistent and unexplained fatigue that significantly impairs daily activities | Tests to rule out other diseases: complete blood count, ESR, CRP, complete metabolic panel, TSH, urinalysis |
| Endocarditis | Arterial emboli, arthralgia, fever, heart murmur, myalgia | Positive echocardiography findings with vegetation on heart valve; positive blood culture |
| Fibromyalgia | Poorly localized pain above and below waist on both sides, involving neck, back, and chest | 11 of 18 sites (bilateral) perceived as painful. Posteriorly, the sites are: occiput, trapezius, supraspinatus, gluteal, greater trochanter. Anteriorly, they are: low cervical, second rib, lateral epicondyle, knee |
| HIV infection | Arthralgia, fever, lymphadenopathy, malaise, myalgia, peripheral neuropathy, rash | Western blot assay for detection of HIV antibodies |
| Inflammatory bowel disease | Diarrhea, peripheral arthritis, rectal bleeding, tenesmus | Colonoscopy to assess disease activity; measure CRP level, platelets, and ESR; test for anemia |
| Lyme disease | Arthritis, carditis, erythema migrans, neuritis | Serologic testing for Lyme disease |
| Mixed connective tissue disease | Arthralgia, myalgia, puffy fingers, Raynaud phenomenon, sclerodactyly | Tests for elevated ESR and hypergammaglobulinemia, positive anti-U1RNP antibodies |
| Psoriatic arthritis | Psoriasis before joint disease, nail changes in fingers and toes | Inflammatory articular disease and more than three of the following: psoriasis, nail changes, negative rheumatoid factor, dactylitis, radiographic evidence of new bone formation in hand or foot |
| Reactive arthritis | Acute nonpurulent arthritis from infection elsewhere in the body | Clinical diagnosis to identify triggers; serologic findings of recent infections may be present |
| Rheumatoid arthritis | Morning joint stiffness lasting more than one hour; affected joints are usually symmetric, tender, and swollen | Positive tests for rheumatoid factor and anticyclic citrullinated antibodies; synovial fluid reflects inflammatory state |
| Sarcoidosis | Cough, dyspnea, fatigue, fever, night sweats, rash, uveitis | Chest radiography, bilateral adenopathy with biopsy revealing non-caseating granuloma, elevated angiotensin-converting enzyme level |
| Systemic sclerosis | Arthralgia, decreased joint mobility, myalgia, Raynaud phenomenon, skin induration | Tests for specific autoantibodies |
| Thyroid disease | Dry skin, fatigue, feeling cold, weakness | Measure TSH |
INITIAL EVALUATION
SLE should be suspected in a patient with symptoms in at least two of the following organ systems: constitutional, musculoskeletal, skin, renal, neuropsychiatric, hematologic, cardiac, pulmonary, gastrointestinal, or reticuloendothelial.8 Specific symptoms are listed in Table 2.8,13 Discoid rash (positive likelihood ratio [LR+] = 18), malar rash (LR+ = 14), unexplained seizures or psychosis (LR+ = 13), and photosensitivity (LR+ = 11) provide the strongest evidence in favor of SLE.14
| System | ACR criteria* | SLICC criteria† |
|---|---|---|
| Cardiac/pulmonary | Pleuritis (pleuritic pain or rub, or pleural effusion), or pericarditis (documented by electrocardiography, rub, or pericardial effusion) | Serositis (pleurisy for more than one day, pleural effusion, or pleural rub; pericardial pain more than one day, pericardial effusion, pericardial rub, or pericarditis) |
| Hematologic | Hemolytic anemia, or leukopenia (< 4,000 cells per mm3), or lymphopenia (< 1,500 cells per mm3), or thrombocytopenia (< 100,000 cells per mm3) | Hemolytic anemia Leukopenia (< 4,000 cells per mm3) more than once or lymphopenia (< 1,000 cells per mm3) more than once Thrombocytopenia (< 100,000 cells per mm3) |
| Immunologic | Positive ANA result | Positive ANA result |
| Elevated anti-dsDNA, anti-Sm, or antiphospholipid antibodies | Elevated anti-dsDNA, anti-Sm, or antiphospholipid antibodies, low complement (C3, C4, CH 50), or direct Coombs test (in the absence of hemolytic anemia) | |
| Discoid rash | Chronic cutaneous lupus | |
| Photosensitivity | Nonscarring alopecia | |
| Oral ulcers or nasal ulcers | Oral ulcers or nasal ulcers | |
| Musculoskeletal | Nonerosive arthritis involving two or more joints | Synovitis involving two or more joints, or tenderness at two or more joints and at least 30 minutes of stiffness in the morning |
| Neuropsychiatric | Seizure or psychosis | Seizures, psychosis, mononeuritis complex, myelitis, or peripheral or cranial neuropathy |
| Renal | Persistent proteinuria > 0.5 g per day or > 3+ on urine dipstick testing, or cellular casts | Urinary creatinine (or 24-hour urinary protein) > 500 mg, or red blood cell casts |
| Skin/mucosal | Malar rash | Acute cutaneous lupus or subacute cutaneous lupus |
Once SLE is suspected, the initial evaluation should include an antinuclear antibody (ANA) test.15 This is a highly sensitive test, with positive results in about 94% of patients with SLE.15 SLE is unlikely in a patient with negative results. However, it also has low specificity, and may be positive in healthy patients. Although most patients with SLE have positive ANA test results, most patients with positive ANA results do not have SLE. If results show a 1:40 titer or higher, more specific tests should be performed, including measurement of anti–double-stranded DNA (anti-dsDNA), anti-Smith, anti-RNP, anticardiolipin, and beta-2 glycoprotein antibodies and lupus anticoagulant; elevated levels of one or more of these biomarkers increase the likelihood of SLE. Similarly, low levels of complements C3 and C4 increase the likelihood of SLE.8 Other tests that should be performed at initial evaluation include urinalysis, comprehensive metabolic panel, complete blood count, and direct Coombs test. The erythrocyte sedimentation rate (LR+ = 5.3 if greater than 100 mm per hour) and C-reactive protein level are useful to quantify disease activity.14
DIAGNOSTIC CRITERIA
Diagnosis of SLE begins with a high index of suspicion. The ACR has 11 diagnostic criteria for SLE8; if a patient meets at least four, SLE can be diagnosed with 95% specificity and 85% sensitivity.16,17 The criteria include malar or discoid rash; photosensitivity; oral ulcers; arthritis; serositis; abnormal ANA titers; and renal, neurologic, hematologic, or immunologic disorders.8
In 2012, the Systemic Lupus International Collaborating Clinics (SLICC) revised and validated the ACR criteria.13 In the SLICC system, a patient must meet at least four criteria, including at least one abnormal clinical criterion and one abnormal immunologic criterion, or the patient must have biopsy-confirmed lupus nephritis and elevated ANA or anti-dsDNA levels.13 The SLICC criteria, which have not been endorsed by the ACR, have greater sensitivity (97%) but lower specificity (84%) compared with the ACR criteria.13 Because the SLICC criteria have not been tested for the purpose of diagnosis, the ACR criteria continue to be the diagnostic standard.13
Manifestations and Management
There are many manifestations of SLE, and multiple organ systems may be affected (Table 3).8–11,18–21 Fatigue and arthralgia are present in almost all patients with SLE, whereas renal involvement manifests in about 50% of patients.22 The most important predictors of disease progression are older age at diagnosis, black race, and low income.23
The management of SLE depends on the system involved. All patients with SLE should receive education, counseling, and support. Hydroxychloroquine (Plaquenil) is the cornerstone of treatment because it reduces disease flares and other constitutional symptoms.24,25 Low-dose glucocorticoids can be used to treat most manifestations. Figure 2 is an algorithm for managing SLE.8,24–31
| Symptoms | Lifetime prevalence | Treatment | Prevention and screening |
|---|---|---|---|
| Arthralgia | 95% | Glucocorticoids, hydroxychloroquine (Plaquenil), methotrexate, nonsteroidal anti-inflammatory drugs | — |
| Fatigue | 90% | Aerobic exercise (possibly) | Minimize exertion, get adequate sleep |
| Cutaneous lupus | 70% to 80% | Topical glucocorticoids, chloroquine (Aralen), hydroxychloroquine | Use sunscreen and wear protective clothing |
| Hematologic | Most patients symptoms | Azathioprine (Imuran), mycophenolate (Cellcept), rituximab (Rituxan); transfusion for anemia (possibly) | Monitor and treat infection, especially in patients with leukopenia |
| Renal symptoms | 50% | Azathioprine, cyclophosphamide, glucocorticoids, mycophenolate | Urinalysis and serum creatinine test every three months |
| Cardiovascular symptoms | 28% to 40% | Antihypertensive agents, cholesterol-lowering agents | Treat risk factors aggressively |
| Neuropsychiatric symptoms | 12% to 23% | Glucocorticoids; anticonvulsants, antidepressants, and antipsychotics for depression and headaches; antithrombotic agents and cyclophosphamide for thrombotic symptoms and cerebritis | Control aggravating factors and symptoms |
| Pulmonary symptoms | 16% | Depends on type of involvement and severity; azathioprine, cyclophosphamide, glucocorticoids, mycophenolate, plasmapheresis | — |
MUSCULOSKELETAL SYSTEM
Musculoskeletal involvement is present in 95% of patients with SLE and manifests as arthralgias, myalgias, or nonerosive inflammatory arthritis.10 The arthritis is usually symmetric and polyarticular, with a predilection for smaller joints. Fibromyalgia is also more common among patients with SLE. Antimalarials and low-dose glucocorticoids are first-line agents used to treat arthritis pain associated with SLE.26,32 Hydroxychloroquine is favored over chloroquine (Aralen) because it is less toxic. Nonsteroidal anti-inflammatory drugs can be used as adjunctive therapy to treat joint pain.
INTEGUMENTARY SYSTEM
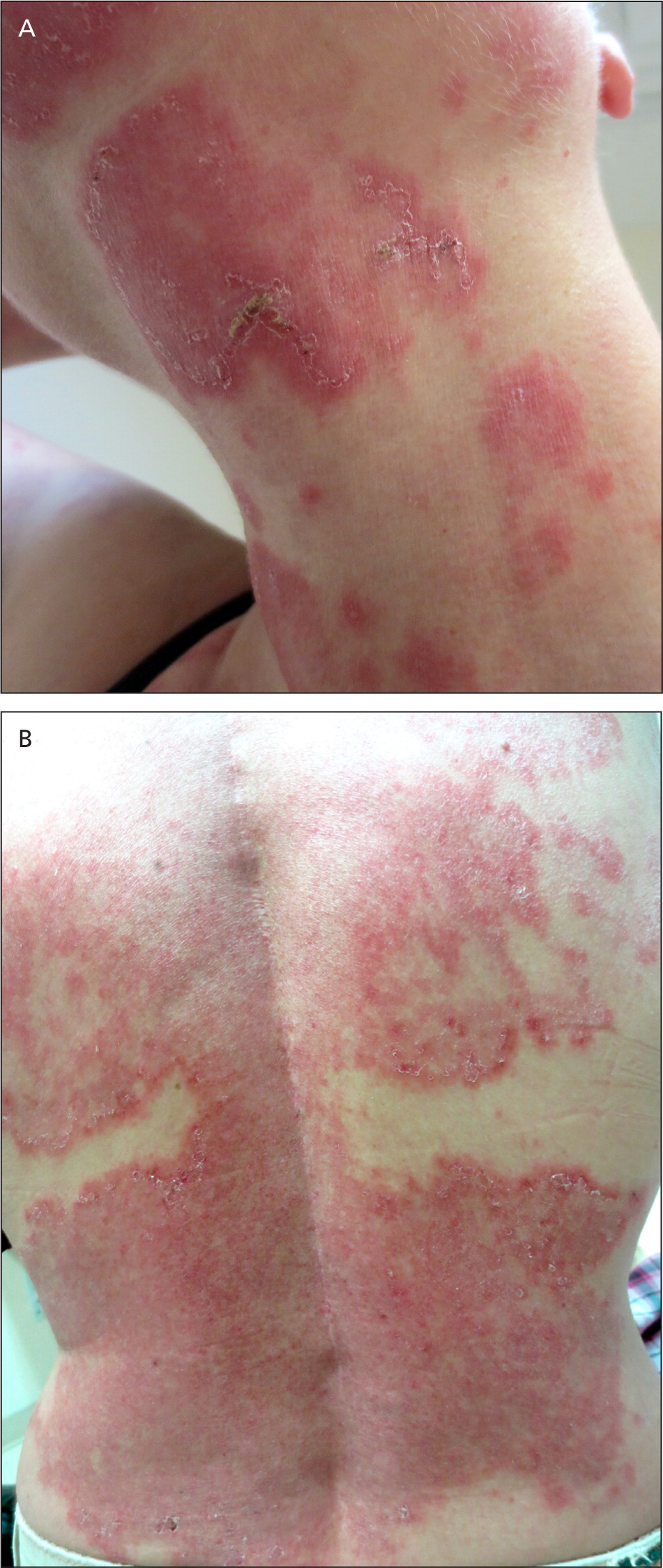
About 70% to 80% of patients with SLE develop skin lesions during the course of disease.18 Malar rash occurs in about 30% of patients.18 Acute and subacute cutaneous lupus rash (Figure 3) can present anywhere on the body, but most commonly occurs on sun-exposed areas. Patients with SLE should use sunscreens with sun protective factors of 15 or higher.32 Mucous membrane involvement, hair loss, and Raynaud phenomenon are also common (Figure 4).

URINARY SYSTEM
The visceral organ most commonly involved in SLE is the kidney.18 Although almost all patients with SLE have immunoglobulin deposits in the glomeruli, only 50% develop clinical renal disease.22 Screening for nephritis with urinalysis and serum creatinine measurement should be done at three- to six-month intervals.8,33 When a patient with SLE has clinical or laboratory features that suggest nephritis, 24-hour urine testing for protein or a spot urine protein:creatinine ratio should be obtained.27 Referral for renal biopsy should be considered in patients with proteinuria of at least 1 g in 24 hours, or at least 0.5 g in 24 hours with hematuria or cellular casts. A combination of glucocorticoid plus immunosuppressant is more effective than glucocorticoids alone in preserving renal function in patients with SLE.32 Standard treatment includes mycophenolate (Cellcept) or cyclophosphamide plus a glucocorticoid.27–29,34
NERVOUS SYSTEM
The nervous system is affected in about 12% to 23% of patients with SLE.11 Neuropsychiatric manifestations of SLE include headaches, seizures, cerebrovascular disease, psychosis, cranial neuropathy, and movement disorder.35 Magnetic resonance imaging of the brain should be considered in patients with headache or seizure because white matter lesions are common in neuropsychiatric SLE.35 Treatment includes glucocorticoids and cyclophosphamide.26,30,31
HEMATOLOGIC SYSTEM
Hematologic abnormalities associated with SLE can include leukopenia, lymphopenia, hemolytic anemia, and thrombocytopenia.18 Patients with severe leukopenia are at increased risk of infection, and patients with anemia may need supportive care and transfusion.
CARDIOVASCULAR SYSTEM
Premature-onset cardiovascular disease is much more common in women with SLE. Compared with an age-matched group in the Framingham cohort, women 35 to 44 years of age who had SLE had a greatly increased risk of myocardial infarction (rate ratio = 52; 95% confidence interval, 22 to 98).42 The increased risk of accelerated atherosclerosis suggests that there are other SLE-related factors, such as renal disease, cytokines, inflammatory mediators, antiphospholipid antibodies, oxidized low-density lipoprotein, and adverse effects of treatment, that cause accelerated cardiovascular disease.19,43 SLE is an independent risk factor for the development of atherosclerosis, and is identified as such by the American Heart Association.19,44
It is important to counsel patients to reduce traditional cardiovascular risk factors such as smoking and obesity, and to have routine screenings for diabetes mellitus, hypertension, and dyslipidemia. The recent Joint National Committee-8 guideline for hypertension and the Adult Treatment Panel IV guideline for hyperlipidemia do not make separate recommendations for patients with SLE.45,46 Family physicians should be aware of the increased risk of cardiovascular events in patients with SLE, and should take steps to optimize risk in accordance with national guidelines. Although guidelines do not address this need, patients with SLE may benefit from treatment with a statin because of their increased 10-year risk of a cardiovascular event.47,48 Blood pressure should also be treated to a goal similar to that for patients with comorbid conditions such as diabetes (less than 140/90 mm Hg).44,45,47,49
RESPIRATORY SYSTEM
Lung involvement in SLE can vary from minor pleuritic pain in serositis to life-threatening complications such as alveolar hemorrhage.50 Pleuritis occurs in 17% to 60% of patients with SLE.50,51 Treatment is based on the type and severity of lung involvement, and may include glucocorticoids, immunosuppressive agents, and plasmaphersis.32,52
REPRODUCTIVE SYSTEM
Pregnant women with SLE have an increased risk of spontaneous abortions, stillbirths, and fetal growth restriction.26 Pregnancy may also increase disease activity and precipitate disease flares.20 Although women with SLE can use most contraceptive methods, those with antiphospholipid syndrome should not use estrogen-containing contraceptives because of an increased risk of thrombosis.53 Women with recurrent pregnancy loss should be screened for antiphospholipid syndrome.
Monitoring and Complications
All patients with SLE should receive ongoing education, counseling, and support. Those with mild SLE that does not involve major organ systems can be monitored by primary care physicians.8 Patients with increased disease activity, complications, or adverse effects from treatment should be referred to a rheumatologist.8 Family physicians can monitor disease activity and therapy in patients with moderate to severe SLE.8
Measurement of anti-dsDNA antibodies, complements, and creatinine; a complete blood count; and urinalysis should be performed every three to six months to monitor disease activity.8 Annual eye examinations are required for patients receiving hydroxychloroquine.36 Screening for dyslipidemia, diabetes, and osteoporosis should be performed regularly in patients receiving glucocorticoids. For patients with chronic kidney disease who are receiving long-term immunosuppressive therapy, immunization with 13-valent pneumococcal conjugate vaccine (Prevnar) followed by 23-valent pneumococcal polysaccharide vaccine (Pneumovax) should be considered.54 Live vaccines should not be given to patients with SLE when they are receiving immunosuppressive therapy, and they should be delayed for at least one month after completion of the therapy. Table 4 includes details for monitoring medications used in SLE treatment.8,24–27,55,56
| Medications | Indications | Dosage | Monitoring and precautions | Cost* |
|---|---|---|---|---|
| Azathioprine (Imuran) | Lupus nephritis, severe SLE | 1.5 to 2.5 mg per kg per day | CBC and complete metabolic panel at least every three months to monitor for myelosuppression, hepatotoxicity, and lymphoproliferative disorders | $21 ($410) for 60 50-mg tablets |
| Belimumab (Benlysta) | SLE | 10 mg per kg IV per day | Monitor for serious infection and malignancies | NA ($1,630) per 400-mg vial |
| Cyclophosphamide | Lupus nephritis, severe SLE | 1 to 3 mg per kg per day | CBC and complete metabolic panel at least every three months to monitor for myelosuppression, malignancy, immunosuppression, and hemorrhagic cystitis | $365 (NA) for 30 50-mg capsules |
| Glucocorticoids | Low dose for treating SLE without major organ damage; higher doses for cerebritis, lupus nephritis, refractory conditions, and thrombocytopenia | Low dose: ≤ 10 mg prednisone per day Higher dose: 40 to 60 mg prednisone per day | Glucose levels every three to six months, and total cholesterol level and bone density testing annually; use with caution in patients with hypertension, hyperglycemia, hyperlipidemia, osteoporosis, or infection | $5 (NA) for 30 10-mg tablets; $9 (NA) for 60 20-mg tablets |
| Hydroxychloroquine (Plaquenil) | Long-term protective effect on SLE-related organ damage | 200 to 400 mg per day | Ophthalmologic examination every six to 12 months to monitor for macular damage | $41 ($197) for 30 200-mg tablets |
| Methotrexate | Arthritis, cutaneous lupus, serositis, severe SLE | 7.5 to 25 mg per week | CBC and complete metabolic panel at least every three months to monitor for myelosuppression, hepatic fibrosis, and pulmonary infiltrates and fibrosis | $15 (NA) for 12 2.5-mg tablets |
| Mycophenolate (Cellcept) | Lupus nephritis, refractory SLE | 2 to 3 g per day | CBC and complete metabolic panel at least every three months to monitor for myelosuppression and infection | $49 ($1,880) for 240 250-mg capsules |
| Nonsteroidal anti-inflammatory drugs | Lupus joint pain | Depends on preparation | CBC and renal testing annually; use with caution in patients with gastrointestinal bleeding, liver or kidney disease, or hypertension | Depends on preparation |
| Rituximab (Rituxan) | Refractory severe SLE | Two 1-g doses IV, two weeks apart | CBC every two to four months; use with caution in patients with history of infusion reaction | NA ($12,000 to $15,600) per 1-g infusion |
Patients with SLE have a higher mortality rate due to circulatory disease, infections, renal disease, non-Hodgkin lymphoma, and lung cancer.57 Damage related to SLE is most common in the musculoskeletal (15%), neuropsychiatric (11%), cardiovascular (9%), and hematologic (3%) systems.57 Osteoporosis is a potentially preventable complication of SLE.57 The incidence of non-Hodgkin lymphoma is increased three- to fourfold compared with the general population.57
| Complication | Frequency of follow-up | Prevention, monitoring, and management |
|---|---|---|
| None; mild, stable SLE8 | Every three to six months | History for features of SLE, physical examination, CBC, creatinine level, urinalysis, anti-dsDNA, complements; keep all health maintenance screenings and vaccinations up to date |
| Cardiovascular abnormalities49,57 | Every visit | Optimal lupus control with minimal glucocorticoid use; judicious use of antimalarial and other immunosuppressive agents; smoking cessation, adequate exercise, low-cholesterol diet, lipid-lowering therapy, blood pressure control, screening for diabetes mellitus |
| Infection8,57 | Every visit | Assure that vaccinations are up to date; judicious use of immunosuppressive agents |
| Malignancy57,58 | Yearly | Assure that routine cancer screenings are up to date; screen for high-risk cancers (e.g., hematologic, non-Hodgkin lymphoma, lung, cervical) |
| Moderate to severe SLE with complications8 | Frequent | Monitor in conjunction with rheumatologist and lupus care subspecialists |
| New-onset nephritis8,27 | Monthly or more frequently | Urinalysis, 24-hour urinary protein level, creatinine clearance, CBC, levels of cholesterol, calcium, phosphorus, alkaline phosphatase, sodium, and potassium; useful to assess complements and anti-dsDNA |
| Receiving high-dose glucocorticoids8,57 | Every visit | Consider steroid-sparing agent; use lowest dose possible to achieve optimum disease control; glucose testing every three to six months; cholesterol testing annually; DEXA every one to two years; maintain high index of suspicion for avascular necrosis if patient has acute joint pain |
| Receiving hydroxychloroquine (Plaquenil)8,36 | Every six to 12 months | Ophthalmologic examination to screen for retinal toxicity; keep dosage to no more than 6.5 mg per kg per day |
| Receiving immunosuppressive or cytotoxic agents8 | Every one to two weeks initially, then every one to three months | CBC and liver function testing at baseline, then every one to two weeks at initiation of therapy, then one to three months; judicious use of immunosuppressive medications, vigilance for signs and symptoms of infection; routine cancer screening; avoidance of live vaccines; if live vaccines are needed, administer one month after therapy completion |
| Receiving low-dose glucocorticoids8 | Every visit to every one to two years | Keep dosage as low as possible; healthy diet with adequate physical activity; smoking cessation; annual cholesterol and glucose testing; consider DEXA every one to two years for patients receiving long-term therapy |
| Renal abnormalities8,27,54 | Every three months or more frequently, depending on disease state | Regular screening for proteinuria and hematuria; regular serum creatinine level; for patients with chronic kidney disease, vaccination with 13-valent pneumococcal conjugate vaccine (Prevnar) or 23-valent pneumococcal polysaccharide vaccine (Pneumovax), as indicated |
| Severe hemolytic anemia8 | Weekly | Hematocrit and reticulocyte count; may require transfusion |
| Severe thrombocytopenia (< 50,000 cells per mm3)8 | Weekly | Platelet count weekly initially; may require transfusion |
Data Sources: Searches were done in Essential Evidence Plus, Clinical Evidence, the Cochrane Database of Systematic Reviews, and DynaMed. Key terms included systemic lupus erythematosus, manifestation, treatment, and management. Search dates: January 28 to February 15, 2015; September 23, 2015; and April 8, 2016.
The authors thank Robert Langan, MD, FAAFP, for assistance with the manuscript.