
Am Fam Physician. 2016;94(6):486-489
Author disclosure: No relevant financial affiliations.
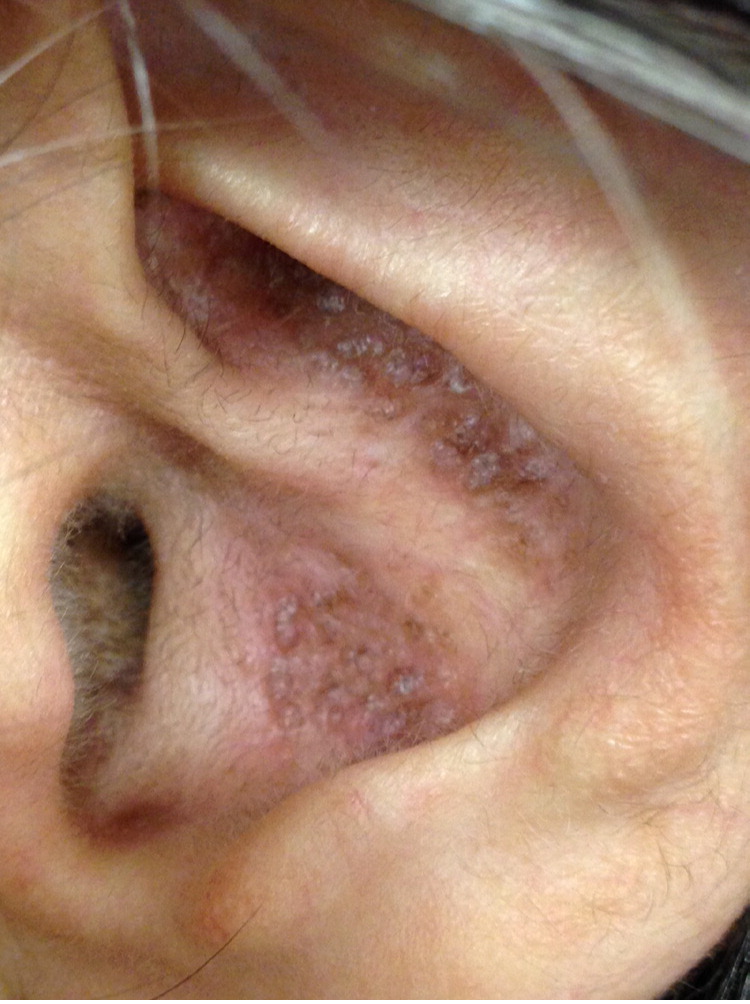
A 59-year-old woman presented with several years of persistent and worsening bilateral pruritic auricular lesions. The rash was limited to the ears, and the patient did not have a history of a similar rash on other areas of her body. She reported rubbing and scratching her ears often. A trial of ketoconazole shampoo and triamcinolone cream was ineffective.

Question
Discussion
The answer is A: amyloidosis. Amyloid deposition in the skin can occur with systemic disease such as multiple myeloma, in which amyloid is derived from immunoglobulin light chains. It can also occur without systemic disease in primary localized cutaneous variants of amyloidosis in which amyloid is derived from epidermal keratin.
Auricular amyloidosis, also known as amyloidosis of the auricular concha or collagenous papules of the ear, is a variant of primary localized cutaneous amyloidosis.1,2 Patients present with papules or plaques limited to the auricular concha. Lichen amyloidosis is another form that presents on the front of the shins and extensor aspect of the forearms.3 The calves, ankles, dorsal feet, thighs, and trunk may also be affected.4
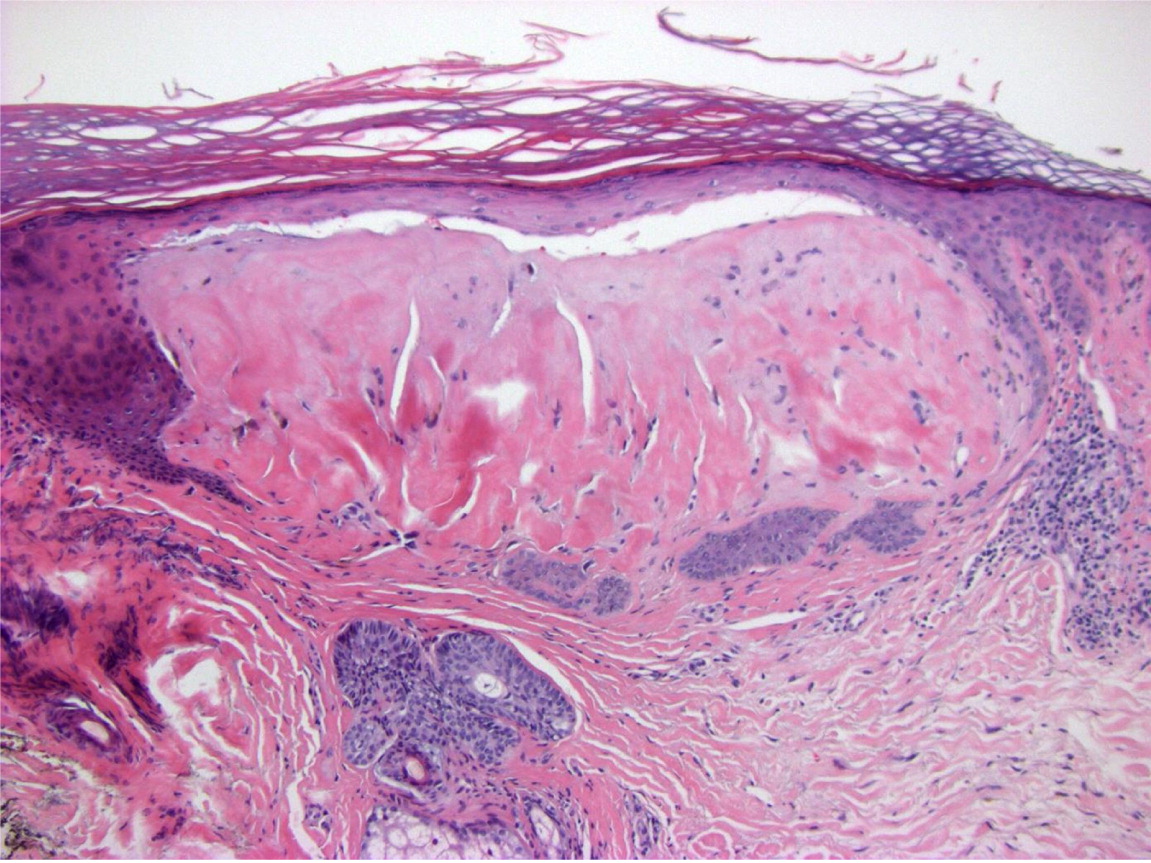
The punch biopsy revealed pale homogenous eosinophilic globules in the papillary dermis (Figure 3), which is characteristic of amyloid deposition. The Congo red stain was reactive. Chronic irritation to the skin has been proposed as the etiology of the amyloid deposition in primary localized cutaneous amyloidosis.5 The chronic damage to the epidermis is thought to induce apoptosis of keratinocytes, leading to amyloid deposition high in the papillary dermis.6 Histochemically, the amyloid stains selectively with Congo red, leading to the characteristic apple-green birefringence under polarized light.1
Colloid milium is a rare disorder in which dome-shaped, translucent to yellow-brown papules develop in sun-exposed areas of the skin. It is thought to be related to photoinduced damage to dermal elastic fibers. On histopathology, nodules composed of homogenous eosinophilic colloid material are seen in the papillary dermis with a staining profile similar to amyloidosis.7
Flat warts, or verrucae plana, appear as flat, flesh-colored papules. The warts are caused by human papillomavirus types 2, 3, and 10. The presentation can vary from a few solitary papules to numerous confluent papules. Histologic examination reveals hyperkeratosis with cytoplasmic vacuolation of the keratinocytes in the upper part of the stratum spinosum.8
Intertriginous granular parakeratosis presents as pruritic, brownish-red, keratotic papules that can coalesce into plaques in intertriginous sites, such as the axillae. It is thought to be caused by a keratinization disorder. The histopathology is characterized by parakeratosis with retention of basophilic granules within the areas of parakeratosis.9
| Condition | Characteristics | Area affected | Demographic affected |
|---|---|---|---|
| Amyloidosis | Highly pruritic, pigmented papules and plaques | Shins, upper back, auricular concha; other sites of chronic scratching | Adults |
| Colloid milium | Dome-shaped, translucent to yellow-brown papules | Sun-exposed areas | Middle-aged, fair-skinned individuals |
| Flat warts (verrucae plana) | Flat, flesh-colored papules | Face, dorsal hands, and shins are most common | Usually children |
| Intertriginous granular parakeratosis | Pruritic, brownish-red, keratotic papules that can coalesce into plaques | The axillae are most common, but any intertriginous site can be affected | Adult form almost always occurs in women; childhood form in diaper area affects boys and girls equally |
