
Am Fam Physician. 2016;94(10):810-816
Author disclosure: No relevant financial affiliations.
Acute monoarthritis can be the initial manifestation of many joint disorders. The most common diagnoses in the primary care setting are osteoarthritis, gout, and trauma. It is important to understand the prevalence of specific etiologies and to use the appropriate diagnostic modalities. A delay in diagnosis and treatment, particularly in septic arthritis, can have catastrophic results including sepsis, bacteremia, joint destruction, or death. The history and physical examination can help guide the use of laboratory and imaging studies. The presence of focal bone pain or recent trauma requires radiography of the affected joint to rule out metabolic bone disease, tumor, or fracture. If there is a joint effusion in the absence of trauma or recent surgery, and signs of infection (e.g., fever, erythema, warmth) are present, subsequent arthrocentesis should be performed. Inflammatory synovial fluid containing monosodium urate crystals indicates a high probability of gout. Noninflammatory synovial fluid suggests osteoarthritis or internal derangement. Pitfalls in the diagnosis and early treatment of acute monoarthritis include failure to perform arthrocentesis, administering antibiotics before aspirating the joint when septic arthritis is suspected (or failing to start antibiotics after aspiration), and starting treatment based solely on laboratory data, such as an elevated uric acid level.
Monoarthritis refers to the clinical presentation of pain or swelling in a single joint.1 The diagnosis can pose a considerable challenge in the primary care setting because the pain may be limited to the joint, or it may represent early manifestation of a systemic disease.2 Understanding the clinical clues associated with potential diagnoses and using an evidence-based, systematic clinical approach are of utmost importance.3 A delay in diagnosis and treatment, particularly with septic arthritis, can have catastrophic results including sepsis, bacteremia, joint destruction, or death.3–5 Pitfalls in the diagnosis and early treatment of acute monoarthritis include failure to perform arthrocentesis, administering antibiotics before aspirating the joint when septic arthritis is suspected (or failing to start antibiotics after aspiration), and starting treatment based solely on laboratory data, such as an elevated uric acid level.3–5
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Radiography is not necessary for an accurate diagnosis of monoarthritis in the absence of trauma or focal bone pain. | C | 3, 4 |
| Analysis of synovial fluid distinguishes infectious and inflammatory causes of acute monoarthritis from noninflammatory causes. | C | 3, 4, 11, 14 |
| Gouty arthritis may be diagnosed without synovial fluid analysis using a diagnostic rule. | C | 24 |
| Disseminated gonococcal infections may not result in septicemia or positive synovial fluid cultures; therefore, cultures should be obtained from the potentially infected mucosal site. | C | 31, 32 |
| Inflammatory synovial fluid containing monosodium urate crystals, particularly in the presence of podagra, is highly suggestive of gout. | C | 23, 24 |
| Erythrocyte sedimentation rate and C-reactive protein level are more useful for following a disease course than discriminating the presence or absence of the disease in patients with monoarthritis. | C | 19, 33 |
Etiology of Acute Monoarthritis
| Common | |
| Avascular necrosis | |
| Crystals | |
| Calcium oxalate | |
| Calcium pyrophosphate dihydrate (pseudogout) | |
| Hydroxyapatite | |
| Monosodium urate (gout) | |
| Hemarthrosis | |
| Infectious arthritis | |
| Bacteria | |
| Fungi | |
| Lyme disease | |
| Mycobacteria | |
| Virus | |
| Internal derangement | |
| Osteoarthritis | |
| Osteomyelitis | |
| Overuse | |
| Trauma | |
| Less common | |
| Ankylosing spondylitis | |
| Bone malignancies | |
| Bowel disease–associated arthritis | |
| Hemoglobinopathies | |
| Juvenile rheumatoid arthritis | |
| Loose body | |
| Psoriatic arthritis | |
| Reactive arthritis | |
| Rheumatoid arthritis | |
| Sarcoidosis | |
| Systemic lupus erythematosus | |
| Rare | |
| Amyloidosis | |
| Behçet syndrome | |
| Familial Mediterranean fever | |
| Foreign-body synovitis | |
| Hypertrophic pulmonary osteoarthropathy | |
| Intermittent hydrarthrosis | |
| Pigmented villonodular synovitis | |
| Relapsing polychondritis | |
| Synovial metastasis | |
| Synovioma | |
| Systemic onset juvenile idiopathic arthritis (Still disease) | |
| Vasculitic syndromes | |
Symptoms consistent with osteoarthritis include pain that tends to worsen with activity, morning stiffness lasting less than 30 minutes, and asymmetric joint pain.7 The most commonly affected joints are the hands, knees, hips, and spine.7 Although osteoarthritis often follows an insidious course, acute flare-ups are common and can be mistaken for other etiologies. The presence of focal bone pain or recent trauma requires radiography of the affected joint to rule out metabolic bone disease, tumor, or fracture.3,4
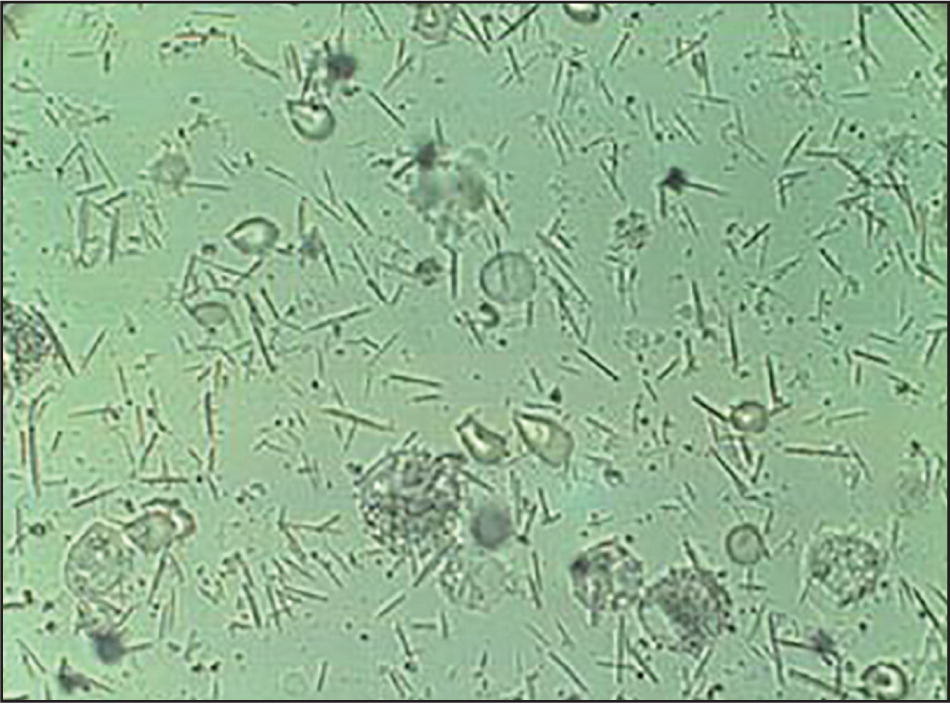
Gout is a common disorder with a 3% prevalence worldwide. It accounts for more than 7 million ambulatory visits in the United States annually.8,9 Crystal-induced arthritis presents as a rapidly developing monoarthritis with swelling and erythema, and most commonly involves the first metatarsophalangeal joint.8 Over time, the joint space can be irreversibly damaged with tophi formation.8,10 The presence of monosodium urate crystals indicates gout; these crystals are identified by their needle-like appearance and strong negative birefringence3,8 (Figure 16 ). Calcium pyrophosphate dihydrate crystals are polymorphic, weakly positive under birefringent microscopy, and their presence indicates pseudogout.3 Other crystal-induced arthritis etiologies include calcium oxalate and hydroxyapatite.1
Infection is a common etiology of joint pain. When infection is suspected in the presence of a joint effusion or inflammation, arthrocentesis should be performed, in addition to further laboratory testing as indicated (Figure 26 ). (A video of arthrocentesis of the knee is available at https://www.youtube.com/watch?v=fZ2dcZhoGP8.) Gonococcal arthritis is the most common type of nontraumatic acute monoarthritis in young, sexually active persons in the United States.11
Septic arthritis is a key consideration in adults presenting with acute monoarthritis, particularly in the presence of joint pain, erythema, warmth, and immobility.12 The most important risk factors for septic arthritis are a prosthetic joint, skin infection, joint surgery, rheumatoid arthritis, age older than 80 years, diabetes mellitus, and renal disease.11 One study found that among persons presenting with acute joint pain and a predisposing condition, 10% had septic arthritis.4 When septic arthritis is suspected, it is important to begin empiric antibiotics immediately following arthrocentesis, because failure to initiate prompt antibiotic therapy can lead to subchondral bone loss and permanent joint dysfunction.5,11,12 The most common route of entry into the joint is hematogenous spread during bacteremia4,12–16; therefore, isolation of the causative agent through synovial fluid culture is essential for the diagnosis and guidance of antibiotic therapy.12
Less common causes of monoarthritis include systemic diseases such as spondyloarthropathies (e.g., psoriatic arthritis, reactive arthritis, ankylosing spondylitis), sarcoidosis, Behçet syndrome, systemic lupus erythematosus, and rheumatoid arthritis.1 Rheumatic diseases and corticosteroid use can cause avascular necrosis of the bone.1
Diagnosing Acute Monoarthritis
The diagnosis of acute monoarthritis begins with a comprehensive history and physical examination to reveal potential diagnostic clues3,6,17 (Table 21,3,6,12,18,19 ). Key elements of the patient history include a review of systems, age, previous joint disease, recent trauma, medication use, family history of gout, concurrent illness, sexual history, diet, travel history, tick bites, alcohol use, intravenous drug use, and an occupational assessment.3,6,17
| Clues from history and physical examination | Diagnoses to consider | Evaluation |
|---|---|---|
| Active range of motion restricted more than passive range of motion | Periarticular pathology | Radiography and/or MRI if indicated |
| Back pain, eye inflammation | Ankylosing spondylitis | HLA-B27 testing, radiography |
| Coagulopathy, use of anticoagulants | Hemarthrosis | CBC, ESR, arthrocentesis to confirm diagnosis and rule out infection |
| Diuretic medication, presence of tophi, renal stones | Gout | CBC, ESR, uric acid level, arthrocentesis with evaluation for crystals |
| Hilar adenopathy, erythema nodosum | Sarcoidosis | CBC, ESR, ACE level, chest radiography, pulmonary referral |
| Immunosuppression and/or intravenous drug abuse | Septic arthritis | CBC, ESR, arthrocentesis for cell count and cultures |
| Insidious onset of pain and swelling over days to weeks | Indolent infection, osteoarthritis, infiltrative disease, tumor | CBC, ESR, arthrocentesis for cell count and cultures, radiography and possible MRI if tumor is a consideration |
| Maximum pain at limits of range of motion (i.e., stress pain) | Osteoarthritis | Radiography |
| Normal joint examination | Referred pain | Consider alternative diagnosis |
| Onset of pain and swelling over several hours or one to two days | Infection, crystal deposition disease, other inflammatory arthritic condition | CBC, ESR, uric acid level, arthrocentesis with evaluation for crystals |
| Pain elicited by joint movements against resistance only | Tendinitis, bursitis | MRI or ultrasonography if diagnosis in question |
| Previous acute attacks in any joint with spontaneous resolution | Crystal deposition disease, other inflammatory arthritic condition | CBC, ESR, uric acid level, arthrocentesis with evaluation for crystals |
| Prolonged course of corticosteroid therapy | Infection, avascular necrosis | CBC, ESR, arthrocentesis for cell count and cultures if concern for infection, radiography and possible MRI if considering avascular necrosis |
| Psoriatic skin plaques, nail pitting, dactylitis | Psoriatic arthritis | CBC, ESR, arthrocentesis, HLA-B27 testing, ANA testing; none of these tests are diagnostic but can exclude other conditions |
| Restricted active and passive range of motion | Intra-articular pathology | Radiography and/or MRI if indicated |
| Sudden onset of pain in seconds or minutes | Fracture, internal derangement, trauma, loose body | Radiography |
| Urethritis, conjunctivitis, diarrhea, rash, sacroiliitis | Reactive arthritis | CBC; ESR; arthrocentesis; HLA-B27 testing; urine PCR testing for Chlamydia trachomatis; stool cultures for Salmonella, Shigella, and Campylobacter |
| Young adult, migratory polyarthralgias, tendons inflamed | Gonococcal arthritis | Urine PCR testing, blood culture, and synovial fluid analysis for Neisseria gonorrhoeae |
Symptoms that worsen with activity and improve with rest suggest a mechanical process, whereas symptoms with an inflammatory process often worsen with rest and present with morning stiffness.1 Osteoarthritis often starts as mild joint inflammation that may initially arouse suspicion for new-onset inflammatory diseases, such as rheumatoid arthritis.20 Morning stiffness and its duration in the affected joint, pain with activity or rest, recent history of trauma, history of previous joint symptoms, and family history of joint inflammation are all important factors that can help differentiate etiologies.12 Osteoarthritis typically worsens with activity, particularly after a period of rest (gelling phenomenon).18 Morning stiffness from osteoarthritis usually lasts for a shorter duration than that of rheumatoid arthritis, which typically lasts 45 minutes or more.7
A gout attack typically begins at night and peaks within 24 hours, causing pain, swelling, and erythema.20 Common clues from the patient history include obesity, a high-calorie diet, alcohol intake, and the use of loop and thiazide diuretics.8 Trauma may also precipitate an acute gout flare-up,8,21 and the presentation can closely resemble septic arthritis.20
Determining whether a condition is truly monoarticular can prove beneficial, because prodromal arthralgias can suggest infection.1 Gonococcal arthritis is often preceded by migratory arthritis and tenosynovitis before settling in a primary joint.1 Conducting a sexual history is imperative, as is documenting any urinary problems, purulent discharge from the urethra, or other signs of infection, such as pharyngitis.11,12 Risk factors such as intravenous drug use, tick bites, and travel history can lead to a diagnosis of infectious or reactive arthritis.1
Axial skeleton inflammatory arthritis (e.g., sacroiliitis) in addition to symptoms in a single peripheral joint suggest a spondyloarthropathy.1 Spondyloarthropathies can often present as monoarthritis and progress from joint to joint in a migratory or additive pattern.20 It is important to ask patients about other symptoms, such as enthesopathy (tenderness at the muscle or fascia attachment sites) and dactylitis (sausage-like swelling of fingers or toes), because these are common.20 Some patients also present with ocular inflammation (uveitis) and urethritis (Reiter syndrome).20 A history of skin conditions and a positive family history of inflammatory arthritis suggest psoriatic arthritis, which can present as monoarthritis in the early stages.20
Physical Examination
The physical examination should focus on the involved and contralateral joints, the surrounding area, possible systemic manifestations, or polyarticular involvement.3,6,17 The first step is to confirm that the joint pain is truly localized and not a periarticular process, such as tendinitis, bursitis, or cellulitis.1 The presence of a joint effusion signifies intra-articular pathology, with patients typically reporting painful limitation of active and passive joint motion.1
A diagnosis of osteoarthritis can often be based on the history and physical examination.3 The characteristic presentation includes painful and limited range of motion, crepitus, effusions, instability, or deformities.18 Heberden and Bouchard nodes are pathognomonic for osteoarthritis. They result from hard, bony thickening that gradually forms around the distal and proximal interphalangeal joints of the fingers, respectively.20 The first carpometacarpal joint is one of the most common sites of osteoarthritis.20
There are many superficial examination findings that can suggest specific diagnoses. Subcutaneous nodules (tophi) and podagra (gouty arthritis of the first metatarsophalangeal joint) are highly specific for gout.20 Erythema nodosum may be a manifestation of sarcoidosis or inflammatory bowel disease; psoriatic skin plaques are associated with psoriatic arthritis; and oral ulcers can indicate reactive arthritis or Behçet syndrome.1
Septic arthritis is most likely to seed within a larger joint,1,22 and to be accompanied by erythema, warmth, and immobility.12 Although clinical manifestations have low sensitivity,12 acute monoarthritis with fever should be considered to have a bacterial etiology until proven otherwise because of the potential consequences of inadequate treatment.20 For example, morbidity associated with septic arthritis includes functional deterioration, arthrodesis, and amputation11,12; the mortality rate is 10% to 20%.12
Diagnostic Tests
Because the causes of acute monoarthritis vary widely, a stepwise approach to diagnosis can aid decision making (Figure 26 ). In the setting of trauma, radiography of the affected joint is required to rule out dislocation or fracture before performing active physical examination maneuvers.1 Radiography can also show signs of osteoarthritis, such as joint space narrowing, osteophytes, and subchondral sclerosis.1 If a joint effusion is present in the absence of traumatic injury, arthrocentesis should be performed, particularly when other inflammatory signs are present and there is a reasonable concern for infection (e.g., fever, erythema, warmth).1
Analysis of synovial fluid distinguishes infectious and inflammatory causes of acute monoarthritis (e.g., rheumatoid, septic, and crystal-induced arthritis) from non-inflammatory causes (e.g., trauma, osteoarthritis).3,4,11,14 Analysis should include cell count and differential, white blood cell count, Gram stain, cultures, and crystal evaluation.1,4
Many cases of acute gouty arthritis are diagnosed without synovial fluid analysis.23 To improve the predictive value of clinical diagnosis, a gout calculator has been developed24,25 (Table 324 ). Seven predictive variables are included in this rule, and a scoring system has been developed to guide the decision to treat the patient for gout, pursue synovial fluid analysis, or search for other causes.24,25 A complete blood count and uric acid level can also aid in the diagnosis, especially if synovial fluid cannot be successfully obtained.3,19
| Patient with monoarthritis | ||
| Male sex | 2 points | |
| Previous patient-reported arthritis attack | 2 points | |
| Onset within 1 day | 0.5 point | |
| Joint redness | 1 point | |
| Involvement of first metatarsophalangeal joint | 2.5 points | |
| Hypertension or ≥ 1 cardiovascular diseases* | 1.5 points | |
| Serum uric acid > 5.88 mg per dL (350 μmol per L) | 3.5 points | |
| Total score: | ________ | |
| ≤ 4 points | > 4 and < 8 points | ≥ 8 points |
| Non-gout in 95% | Uncertain diagnosis | Gout in 87% |
| Consider alternative diagnosis, such as CPPD arthritis, reactive arthritis, septic arthritis, rheumatoid arthritis, osteoarthritis, or psoriatic arthritis | Perform arthrocentesis and analysis with polarization microscopy for the presence of crystals; if not possible or available, then extensive follow-up of the patient | Manage the patient as having gout, including care for cardiovascular risk |
A synovial fluid white blood cell count greater than 50,000 per mm3 (50.0 × 109 per L) with at least 90% neutrophils is the most useful laboratory finding for making an early diagnosis of septic arthritis.3 This traditional cutoff lacks sensitivity because there can be wide overlap with inflammatory conditions, but higher white blood cell counts in the synovial fluid have a greater association with septic arthritis.1,26 Staphylococci and streptococci are the most common bacterial causes at 40% and 28%, respectively, and their presence may suggest drug abuse. These organisms are also associated with cellulitis, endocarditis, and chronic osteomyelitis.12,27,28
Gram-stain results should guide initial antibiotic choice. Gram-negative organisms account for 10% to 21% of cases of septic arthritis.1,12,29 Mycobacterial and fungal arthritis typically present in immunocompromised patients, and Lyme arthritis often presents as a late manifestation of Lyme disease.1,12,30 Special consideration should be given to patients with prosthetic joint infection because the cutoff values for infection may be as low as 1,100 white blood cells per mm3 (1.1 × 109 per L), with a neutrophil differentiation greater than 65%.3 Gonococci are cultured from joints in fewer than 50% of cases of gonococcal arthritis1,31,32; therefore, it is often necessary to obtain cultures from appropriate mucosal sites of infection.1,31,32 Noninflammatory synovial fluid (less than 2,000 cells per mm3 [2.0 × 109 per L]) is suggestive of osteoarthritis or internal derangement.1 Inflammatory synovial fluid containing monosodium urate crystals is highly suggestive of gout, particularly in the presence of podagra; however, the absence of crystals does not exclude crystal-induced arthritis, such as pseudogout.23,24
Erythrocyte sedimentation rate and C-reactive protein level are often elevated in inflammatory conditions.19,33 Literature comparing these two values is limited; however, it has been determined that these tests are more useful for following a disease course than discriminating the presence or absence of the disease.19,33
Data Sources: PubMed and Medline searches were performed using the key terms arthritis, crystal, gonorrhea, gout, infectious, inflammatory, and synovial fluid. The search included reviews, clinical trials, and meta-analyses. Also searched were the Cochrane Database of Systematic Reviews and Essential Evidence Plus. Search dates: September through November 2015, and September 2016.
