
Am Fam Physician. 2017;96(1):44-51
Patient information: See related handout on paronychia, written by the author of this article.
Author disclosure: No relevant financial affiliations.
Paronychia is inflammation of the fingers or toes in one or more of the three nail folds. Acute paronychia is caused by polymicrobial infections after the protective nail barrier has been breached. Treatment consists of warm soaks with or without Burow solution or 1% acetic acid. Topical antibiotics should be used with or without topical steroids when simple soaks do not relieve the inflammation. The presence of an abscess should be determined, which mandates drainage. There are a variety of options for drainage, ranging from instrumentation with a hypodermic needle to a wide incision with a scalpel. Oral antibiotics are usually not needed if adequate drainage is achieved unless the patient is immunocompromised or a severe infection is present. Therapy is based on the most likely pathogens and local resistance patterns. Chronic paronychia is characterized by symptoms of at least six weeks' duration and represents an irritant dermatitis to the breached nail barrier. Common irritants include acids, alkalis, and other chemicals used by housekeepers, dishwashers, bartenders, florists, bakers, and swimmers. Treatment is aimed at stopping the source of irritation while treating the inflammation with topical steroids or calcineurin inhibitors. More aggressive techniques may be required to restore the protective nail barrier. Treatment may take weeks to months. Patient education is paramount to reduce the recurrence of acute and chronic paronychia.
Paronychia is defined as inflammation of the fingers or toes in one or more of the three nail folds. The condition can be acute or chronic, with chronic paronychia being present for longer than six weeks. Although both result from loss of the normal nail-protective architecture, their etiologies are different, thus their treatments differ. Infections are responsible for acute cases, whereas irritants cause most chronic cases.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Ultrasonography can be used to determine the presence of an abscess or cellulitis when it is not clinically evident. | C | 10–12 |
| The addition of topical steroids to topical antibiotics decreases the time to symptom resolution in acute paronychia. | B | 19 |
| Oral antibiotics are not needed when an abscess has been appropriately drained. | C | 25, 26 |
| Chronic paronychia is treated by topical anti-inflammatory agents and avoidance of irritants. Antifungals should not be used. | C | 1, 29 |
| Recommendation | Sponsoring organization |
|---|---|
| Avoid antibiotics and wound cultures in emergency department patients with uncomplicated skin and soft tissue abscesses after successful incision and drainage and with adequate medical follow-up. | American College of Emergency Physicians |
Acute paronychia usually involves only one digit at a time; more widespread disease warrants a broader investigation for systemic issues (Table 1).1,2 Chronic paronychia typically involves multiple digits. Paronychia usually affects the fingernails, whereas ingrown nails (onychocryptosis) are more common with the toenails. Although ingrown toenails resulting from abnormal growth of the nail plate into the nail fold are a cause of acute paronychia, this article will not address the management of ingrown nails, which has been addressed previously in American Family Physician.3 Although prevalence data are lacking, acute paronychia is one of the most common hand infections in the United States. It is three times more common in women, possibly because of more nail manipulation in this population.4
| Common |
| Eczema |
| Herpetic whitlow |
| Psoriasis |
| Less common |
| Dermatomyositis |
| Granuloma annulare |
| Hematomas from pulse oximetry |
| Pyogenic granuloma |
| Reiter syndrome |
| Uncommon |
| Food hypersensitivity |
| Melanoma |
| Pemphigus vulgaris |
| Squamous cell carcinoma |
Anatomy
The relevant anatomy includes the nail bed, nail plate, and perionychium1 (Figure 15 ). The nail bed is composed of a germinal matrix, which can be seen as the lunula, the crescent-shaped white area at the most proximal portion of the nail. The germinal matrix is responsible for new nail growth. The more distal portion of the nail bed is made by the flesh-colored sterile matrix, which is responsible for strengthening the nail plate. The perionychium comprises the three nail folds (two lateral and one proximal) and the nearby nail bed.
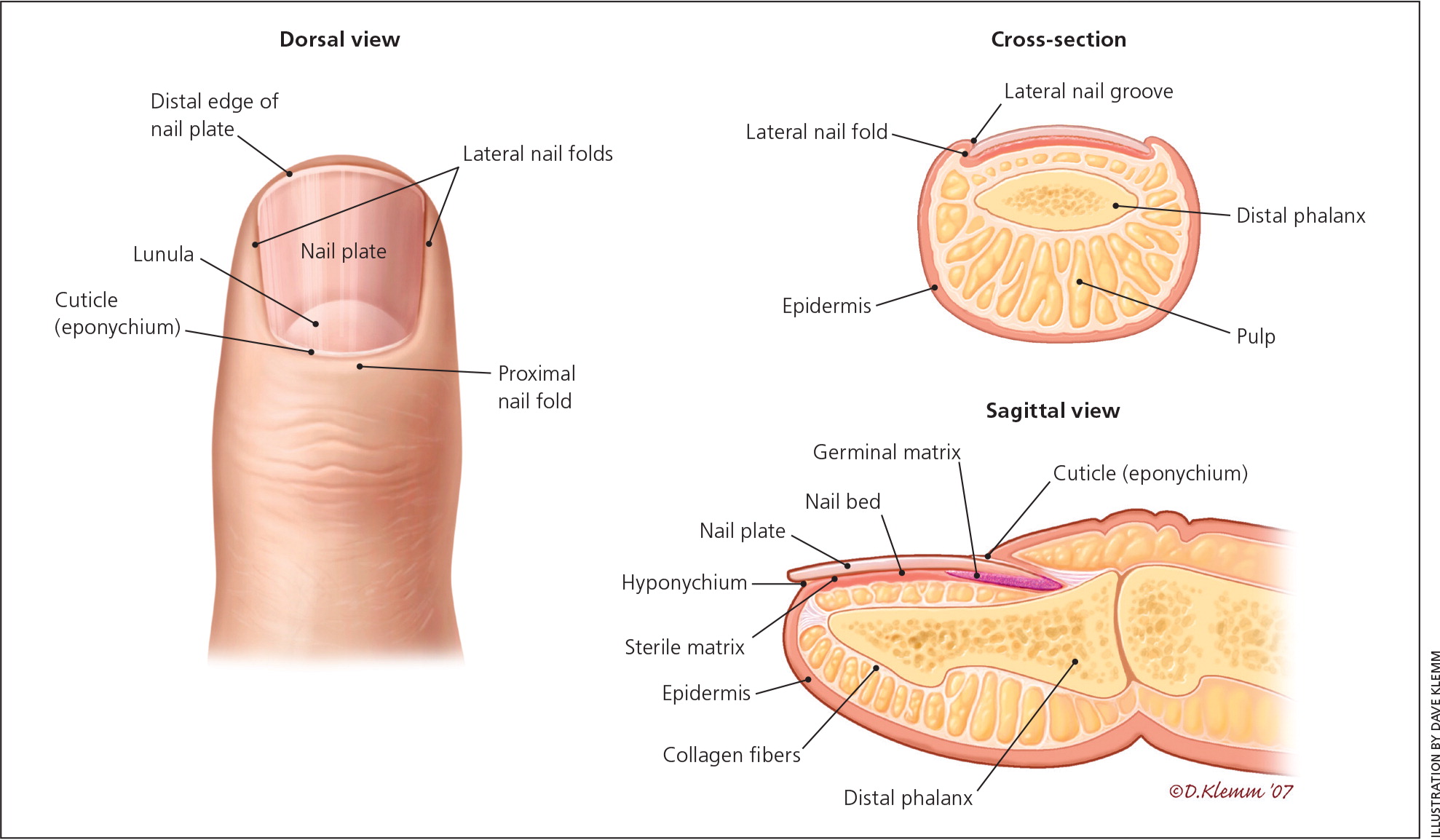
The proximal nail fold is unique compared with the two lateral folds. The nail plate itself arises from a mild depression in the proximal nail fold. The nail divides the proximal nail fold into two parts, the dorsal roof and the ventral floor, both of which contain germinal matrices. The eponychium (also called the cuticle), an outgrowth of the proximal nail fold, forms a watertight barrier between the nail plate and the skin, protecting the underlying skin from pathogens and irritants.2
Acute Paronychia
DIAGNOSIS
Acute paronychia is the result of a disruption of the protective barrier of the nail folds. Once this barrier is breached, various pathogens can create inflammation and infection. Table 2 lists the most common risks of nail fold disruption.5 Patients typically present with rapid onset of an acute, inflamed nail fold and accompanying pain (Figure 2). The diagnosis is clinical, but imaging may be useful if a deeper infection is suspected.6 It is not helpful to send expressed fluid for culture because the results are often nondiagnostic and do not affect management.7,8 In a study of patients requiring hospitalization for paronychia who underwent incision and drainage with culture, only 4% of the cultures were positive, with a polymicrobial predominance of bacteria.6 The most common pathogens isolated are listed in Table 3.2,6 Pseudomonas infections can be identified by a greenish discoloration in the nail bed9 (Figure 3). Other diagnostic tools such as radiography or laboratory tests are needed only if the clinical presentation is atypical. The differential diagnosis of acute paronychia includes a felon, which is an infection in the finger pad or pulp.1,2 Although acute paronychia can lead to felons, they are differentiated by the site of the infection.
| Risk factors |
| Accidental trauma |
| Artificial nails |
| Manicures |
| Manipulating a hangnail (i.e., shred of eponychium) |
| Occupational trauma (e.g., bartenders, housekeepers, dishwashers, laundry workers) |
| Onychocryptosis (i.e., ingrown nails) |
| Onychophagia (nail biting) |
| Recommendations to prevent recurrent paronychia* |
| Apply moisturizing lotion after hand washing. |
| Avoid chronic prolonged exposure to contact irritants and moisture (including detergent and soap). |
| Avoid nail trauma, biting, picking, and manipulation, and finger sucking. |
| Avoid trimming cuticles or using cuticle removers. |
| Improve glycemic control in patients with diabetes mellitus. |
| Keep affected areas clean and dry. |
| Keep nails short. |
| Provide adequate patient education. |
| Use rubber gloves, preferably with inner cotton glove or cotton liners when exposed to moisture and/or irritants. |

| Pathogen | Antibiotic options |
|---|---|
| Gram-negative aerobes | |
| Fusobacterium | Amoxicillin/clavulanate (Augmentin), clindamycin, fluoroquinolones |
| Pseudomonas | Ciprofloxacin |
| Gram-negative anaerobe | |
| Bacteroides | Amoxicillin/clavulanate, clindamycin, fluoroquinolones |
| Gram-negative facultative anaerobes | |
| Eikenella | Cefoxitin |
| Enterococcus | Amoxicillin/clavulanate |
| Klebsiella | Trimethoprim/sulfamethoxazole, fluoroquinolones |
| Proteus | Amoxicillin/clavulanate, fluoroquinolones |
| Gram-positive aerobes | |
| Staphylococcus | Cephalexin (Keflex) |
| For suspected methicillin-resistant Staphylococcus aureus infections: clindamycin, doxycycline, trimethoprim/sulfamethoxazole | |
| Streptococcus | Cephalexin |

If there is uncertainty about the presence of an abscess, ultrasonography can be performed. Fluid collection indicates an abscess, whereas a subcutaneous cobblestone appearance indicates cellulitis.10–12 The digital pressure test has been suggested as an alternative to confirm the presence of an abscess. To perform the test, the patient opposes the thumb and affected finger, applying light pressure to the distal volar aspect of the affected digit. The pressure within the nail fold causes blanching of the overlying skin and clear demarcation of an abscess, if present.13
TREATMENT
Treatment of acute paronychia is based on the severity of inflammation and the presence of an abscess. If only mild inflammation is present and there is no overt cellulitis, treatment consists of warm soaks, topical antibiotics with or without topical steroids, or a combination of topical therapies. Warm soaks have been advocated to assist with spontaneous drainage.14 Although they have not been extensively studied, Burow solution (aluminum acetate solution) and vinegar (acetic acid) combined with warm soaks have been used for years as a topical treatment. Burow solution has astringent and antimicrobial properties and has been shown to help with soft tissue infections.15 Similarly, 1% acetic acid has been found effective for treating multidrug-resistant pseudomonal wound infections because of its antimicrobial properties.16 Soaking can lead to desquamation, which is normal.17 Topical antibiotics for paronychia include mupirocin (Bactroban), gentamicin, or a topical fluoroquinolone if pseudomonal infection is suspected. Neomycin-containing compounds are discouraged because of the risk of allergic reaction (approximately 10%).18 The addition of topical steroids decreases the time to symptom resolution without additional risks.19
If an abscess is present, it should be opened to facilitate drainage. Soaking combined with other topical therapies can be tried, but if no improvement is noted after two to three days or if symptoms are severe, the abscess must be mechanically drained5 (Figure 44 ). No randomized controlled trials have compared methods of drainage, and treatment should be individualized according to the clinical situation and skill of the physician. An instrument such as a nail elevator or hypodermic needle can be inserted at the junction of the affected nail fold and nail.20
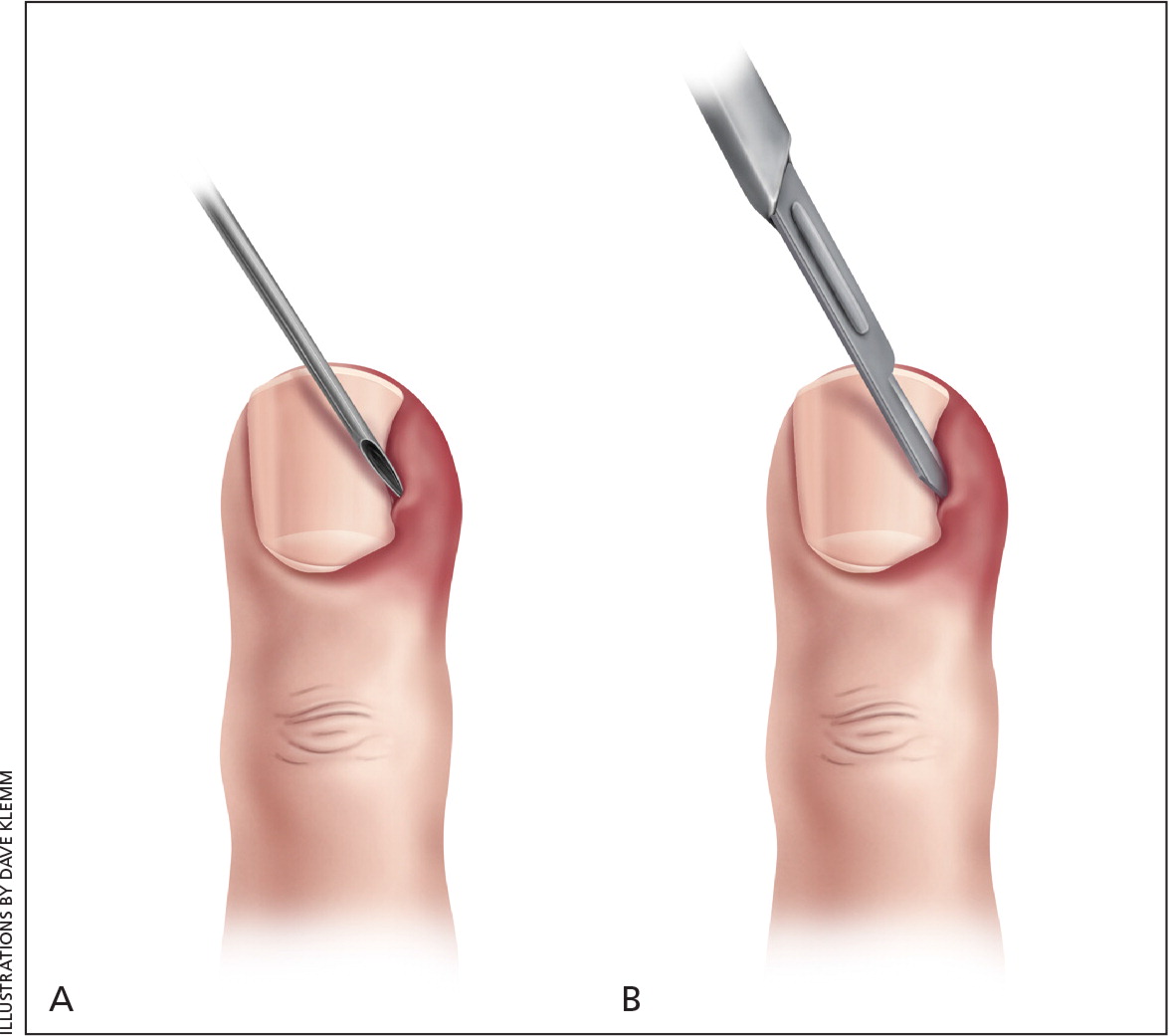
Once the abscess has been opened, spontaneous drainage should occur. If it does not, the digit can be massaged to express the fluid from the opening. If massage is unsuccessful, a scalpel can be used to create a larger opening at the same nail fold–nail junction. If spontaneous drainage still does not occur, the scalpel can be rotated with the sharp side down to avoid cutting the skin fold. Spontaneous drainage should ensue, but if it does not, the area should be massaged to facilitate drainage. The skin directly over the abscess can be opened with a needle or scalpel if elevation of the nail fold and nail does not result in drainage. Ultrasonography can be performed if there is uncertainty about whether an abscess exists or if difficulty is encountered with abscess drainage.10,11
Anesthesia is generally not needed when using a needle for drainage.20 More extensive procedures will likely require anesthesia. Applying ice packs or vapocoolant spray may suffice. If not, infiltrative or digital block anesthesia should be administered. Infiltrative anesthesia or a wing block is faster than a digital block and has less risk of damaging proximal digital blood vessels and nerves.21 A wing block is accomplished by inserting a 30-gauge or smaller needle just proximal to the eponychium and slowly administering anesthetic until the skin blanches (see https://www.youtube.com/watch?v=47qHTmEEHdg). The needle is then directed to each lateral nail fold, and another small bolus of anesthetic is delivered until the skin blanches. Significant resistance is often encountered because of the small needle gauge and tight space. The needle is then removed and reinserted distally along each lateral nail fold until the entire dorsal nail tip is anesthetized. The anesthetic must be injected slowly to avoid painful tissue distension. The pulp and finger pad should not be injected. Several anesthetic agents are available, but 1% to 2% lidocaine is most common. Lidocaine with epinephrine is safe to use in patients with no risk factors for vasospastic disease (e.g., peripheral vascular disease, Raynaud phenomenon). The use of epinephrine allows for a nearly bloodless field without the use of a tourniquet and prolongs the effect of the anesthesia. Buffering and warming the anesthetic aids in patient comfort.22
A wider incision may be needed if the infection extends around the nail. If the entire eponychium is involved, the nail plate can be removed or the Swiss roll technique (reflection of the proximal nail fold) can be performed.23 The Swiss roll technique involves parallel incisions from the eponychium just distal to the distal interphalangeal joint (see Figure 78-4 at http://musculoskeletalkey.com/hand-infections). The tissue is folded over a small piece of non-adherent gauze and sutured to the digit on each side. The exposed nail bed is thoroughly irrigated and dressed with non-adherent gauze, then reevaluated in 48 hours. If no signs of infection are present, the sutures can be removed and the flap of skin returned and left to heal by secondary intention.
Antibiotics are generally not needed after successful drainage.24 Prospective studies have shown that the addition of systemic antibiotics does not improve cure rates after incision and drainage of cutaneous abscesses, even in those due to methicillin-resistant Staphylococcus aureus,25,26 which is more common in athletes, children, prisoners, military recruits, residents of long-term care facilities, injection drug users, and those with previous infections.27 Post-drainage soaking with or without Burow solution or 1% acetic acid is generally recommended two or three times per day for two to three days, except after undergoing the Swiss roll technique. The addition of a topical antibiotic and/or steroids can be considered, but there are no evidence-based recommendations to guide this decision.
The use of oral antibiotics should be limited.7,8 Patients with overt cellulitis and possibly those who are immunocompromised or severely ill may warrant oral antibiotics.25 When they are required, therapy should be directed against the most likely pathogens. If there are risk factors for oral pathogens, such as thumb-sucking or nail biting, medications with adequate anaerobic coverage should be used. Table 3 lists common pathogens and suggested antibiotic options,2,6 but local community resistance patterns should be considered when choosing specific agents.27
Recurrent acute paronychia can progress to chronic paronychia. Therefore, patients should be counseled to avoid trauma to the nail folds. Systemic diseases such as psoriasis and eczema can cause acute paronychia; in these cases, treatment should be directed at the underlying cause.
Chronic Paronychia
DIAGNOSIS
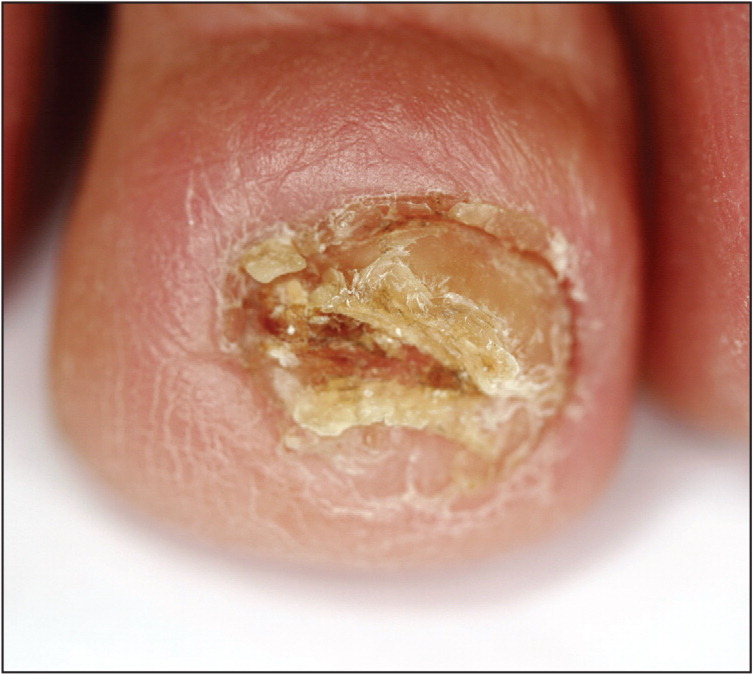
Chronic paronychia results from irritant dermatitis rather than an infection.2 Common irritants include acids, alkalis, or other chemicals commonly used by housekeepers, dishwashers, bartenders, laundry workers, florists, bakers, and swimmers. Once the protective nail barrier is disrupted, repeated exposure to irritants may result in chronic inflammation. Chronic paronychia is diagnosed clinically based on symptom duration of at least six weeks, a positive exposure history, and clinical findings consistent with nail dystrophy (Figure 5).5 The cuticle may be totally absent, and Beau lines (deep side-to-side grooves in the nail that represent interruption of nail matrix maturation) may be present.28 Multiple digits typically are involved. If only a single digit is affected, the possibility of malignancy, such as squamous cell cancer, must be considered (Figure 6).5 The presence of pus and redness may indicate an acute exacerbation of a chronic process.

Fungal infections are thought to represent colonization, not a true pathogen, so antifungals are generally not used to treat chronic paronychia.29 Several classes of medications can cause chronic paronychia: retinoids, protease inhibitors (4% of users), antiepidermal growth factor receptor antibodies (17% of users), and several classes of chemotherapeutic agents (35% of users).30–32 The effect can be immediate or delayed up to 12 months.
TREATMENT
Treatment of chronic paronychia consists of stopping the source of irritation, controlling inflammation, and restoring the natural protective barrier.1 Topical anti-inflammatory agents, steroids, or calcineurin inhibitors are the mainstay of therapy.33 In a randomized, unblinded, comparative study, tacrolimus 0.1% (Protopic) was more effective than betamethasone 17-valerate 0.1%.33 In severe or refractory cases, more aggressive treatments may be required to stop the inflammation and restore the barrier. If the Swiss roll technique is used, the nail bed will need to be exposed for a longer duration (seven to 14 days) than for acute cases (two to three days).23
If a medication is the cause, the physician and patient must decide whether the adverse effects are acceptable for the therapeutic effect of the drug. Discontinuing the medication should reverse the process and allow healing. Doxycycline has been found effective for treatment of paronychia caused by antiepidermal growth factor receptor antibodies.5 A case report describes successful treatment with twice-daily application of a 1% solution of povidone/iodine in dimethyl sulfoxide until symptom resolution in patients with chemotherapy-induced chronic paronychia.34 Zinc deficiency is known to cause nail plate abnormalities and chronic paronychia; treatment with 20 mg of supplemental zinc per day is helpful.35 It is important to inform the patient that the process can take weeks to months to restore the natural barrier. Effective strategies to avoid offending irritants are listed in Table 2.5
This article updates previous articles on this topic by Rockwell4 and by Rigopoulos, et al.5
Data Sources: A PubMed search was completed using the key terms paronychia and nail disorders. The search included systematic and clinical reviews, meta-analyses, reviews of clinical trials and other primary sources, and evidence-based guidelines. Also searched were the Cochrane database, the National Institute for Health and Care Excellence guidelines, the Choosing Wisely Campaign, Essential Evidence Plus, and UpToDate. References from these sources were consulted to clarify statements made in publications. Search dates: December 1, 2015, through January 28, 2017.
The views expressed in this article are those of the author and do not necessarily reflect the official policy or position of the Department of Defense or the U.S. government.