
Am Fam Physician. 2017;96(2):121-122
Author disclosure: No relevant financial affiliations.
A 47-year-old man presented with general fatigue, chills, dyspnea, dry cough, and occasional subjective fever that began two months earlier. He had an unprovoked deep venous thrombosis about one year before presentation that was treated with rivaroxaban (Xarelto) for six months. His medical history was also notable for spinal stenosis and gastroesophageal reflux. He was not taking any medications. He had no history of smoking or substance abuse. He quit chewing tobacco and drinking alcohol one year before presentation. He was divorced and sexually active.
He had a regular pulse of 122 beats per minute, unlabored respirations at 21 breaths per minute, oxygen saturation of 78% on room air, and a body temperature of 100.8°F (38.2°C). Physical examination revealed a new oily and scaly erythematous rash on his forehead, nose, and cheeks. Pulmonary examination showed good air movement but diffuse rales bilaterally. Arterial blood gas measurements showed partial pressure of oxygen was 50 mm Hg and partial pressure of carbon dioxide was 26 mm Hg. Other laboratory testing showed a white blood cell count of 11,000 per μL (11.0 × 109 per L) and hemoglobin level of 11 g per dL (110 g per L).
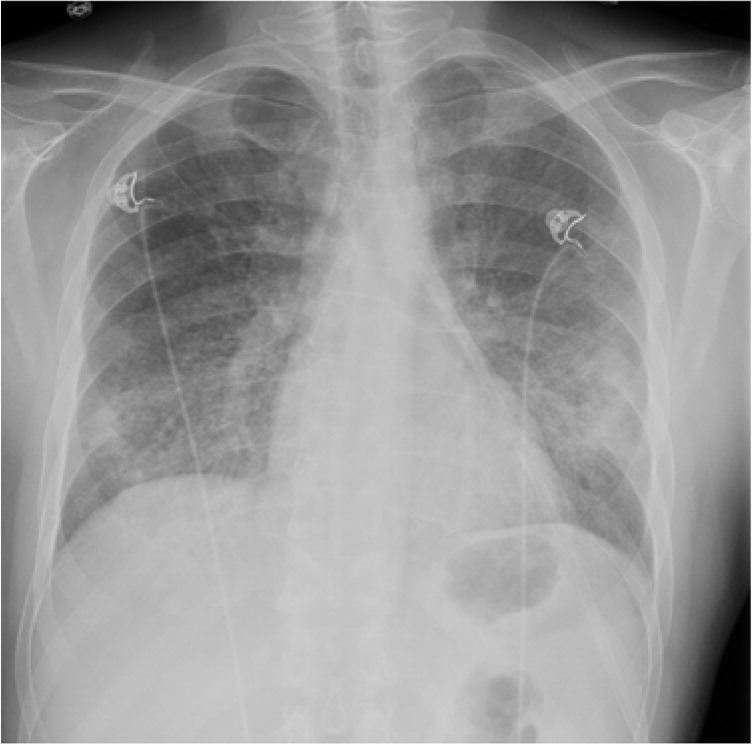
Chest radiography demonstrated diffuse hazy opacities (Figures 1 and 2). A high-resolution computed tomography (CT) scan of the chest also showed diffuse opacities, some with haziness or ground-glass appearance. Limited bedside echocardiography showed no evidence of left ventricular dysfunction or right ventricular strain.

Question
Discussion
The answer is C: Pneumocystis jiroveci pneumonia, previously known as Pneumocystis carinii pneumonia. It is the second most common AIDS-defining opportunistic infection after esophageal candidiasis.1 It is an atypical fungal infection that is uncommon in patients without human immunodeficiency virus (HIV) infection. Bronchoscopic lavage and biopsy confirmed the diagnosis, with a methenamine silver stain highlighting the fungal cyst walls. An HIV antibody test was positive. His viral load was 914,000 copies per mL, and his CD4 cell count was severely depressed at 25 per mm3.
The incidence of P. jiroveci pneumonia among patients with HIV has been reported at 3.9 cases per year.1 The infection typically manifests as subacute dyspnea and nonproductive cough. Findings on chest radiography include bilateral interstitial infiltrates, and chest CT findings include nonspecific ground-glass opacities.2 An additional clue in this patient was new-onset seborrheic dermatitis, which is common in patients with HIV.1,3 First-line treatment for P. jiroveci pneumonia with moderate to severe hypoxemia (arterial partial pressure of oxygen less than 70 mm Hg) is high-dose trimethoprim/sulfamethoxazole and glucocorticoids.4
Miliary tuberculosis that involves the lung can manifest as fever, cough, dyspnea, and hypoxemia. Findings on chest radiography include diffuse reticulonodular infiltrates, whereas CT may show diffuse 2- to 3-mm nodules or nonspecific ground-glass opacities. Because of the nonspecific findings on radiography, diagnosis must be confirmed with histopathology, acid-fast stain, and molecular tests demonstrating the presence of Mycobacterium tuberculosis.5
Mycoplasma (atypical) pneumonia manifests as fever, cough, wheezing, and occasionally dyspnea. Findings on chest radiography may include airspace opacities, reticular opacities, and bronchial thickening. CT findings include airspace consolidations, peribronchial and interstitial thickening, and centrilobular nodules.6
Pulmonary embolism is an important consideration in this patient, especially given his history of deep venous thrombosis. Typical symptoms and signs of pulmonary embolism include dyspnea, cough, chest pain, tachycardia, and hypoxemia. Findings on chest radiography are usually nonspecific but may include atelectasis. In this case, CT angiography was negative for embolus, the chest radiograph showed bilateral interstitial infiltrates, and a bedside echocardiogram showed no sign of right heart strain, making pulmonary embolism unlikely.
| Condition | Imaging findings |
|---|---|
| Miliary tuberculosis | Diffuse reticulonodular infiltrates on chest radiography; diffuse 2- to 3-mm nodules or nonspecific ground-glass opacities on CT |
| Mycoplasma (atypical) pneumonia | Airspace opacities, reticular opacities, and bronchial thickening on radiography; airspace consolidations, peribronchial and interstitial thickening, and centrilobular nodules on CT |
| Pneumocystis jiroveci pneumonia | Bilateral interstitial infiltrates on chest radiography; nonspecific ground-glass opacities on CT |
| Pulmonary embolism | Nonspecific radiographic findings; arterial embolus on CT |
The opinions and assertions contained herein are the private views of the author and are not to be construed as official or as reflecting the views of the U.S. Army Medical Department or the U.S. Army Service at large.
