
Fam Pract Manag. 1999;06(8):17-18
Accountability, measurement can increase performance
The third annual State of Managed Care Quality report “confirms that public accountability and rigorous performance measurement together are the keys to driving quality improvement,” says Margaret E. O'Kane, president of the National Committee for Quality Assurance (NCQA), which released the report.
According to the NCQA, health plans with a two- or three-year history of publicly reporting their performance outscored those new to the reporting process in several areas:
Adolescent immunization rates (67.9 percent vs. 42.9 percent),
Beta blocker treatment after a heart attack (85 percent vs. 72.8 percent),
Cholesterol screening (63.6 percent vs. 55.3 percent),
Chicken pox vaccination (52.6 percent vs. 49.8 percent).
Cholesterol screening and chicken pox vaccination were both new performance measures, according to the NCQA, suggesting that “embracing performance measurement has a positive impact that extends beyond those aspects of care currently being measured.”
Patients value coordination of care, not ‘gatekeeping’
Patients overwhelmingly value their primary care physicians and their role as coordinator of care, says a recent study led by Kevin Grumbach, MD, of the University of California-San Francisco. Ninety-four percent of the 7,700 patients surveyed said they value having a primary care physician who knows their medical history; depending on the specific medical problem, 75 percent to 91 percent said they prefer to seek care first from their primary care physicians.
The study also found that 23 percent of patients felt their primary care physician or medical group limited their access to specialists. Such patients were nearly three times as likely to report low trust in their primary care physicians.

The researchers concluded that although patients want protection from overly restrictive policies that limit access to care, they also want a system that preserves the primary care physician's role as coordinator of care.
The study was sponsored by the Agency for Health Care Policy and Research and appeared in the July 21 issue of the Journal of the American Medical Association.
Fraud-fighters suspected of fraud
Recent testimony before the House Commerce Subcommittee on Oversight and Investigations has revealed that at least six Medicare contractors have settled civil or criminal cases for obstructing government audits in attempts to disguise their poor performance. Two other Medicare contractors have pleaded guilty of similar conduct, with several others currently under investigation. “It is totally unacceptable for this type of behavior by Medicare contractors to continue,” said Fred Upton (R-Mich.), chairman of the subcommittee. “They are supposed to be our watchdogs, but all too often, it turns out that they were foxes guarding the hen house.”
A hearing is scheduled this month to examine allegations of conspiracy and fraud by Medicare contractors.
Y2K Update: HCFA urges providers to test claims processing
HCFA is strongly encouraging all Medicare providers to contact their contractors to test whether their data exchange process can handle claims dated with the year 2000. Although HCFA's internal and contractor systems are reported to be Y2K ready, recent testing of year-2000-dated claims revealed significant external problems. (See http://www.hcfa.gov/y2k/y2kprbpv.htm for a full report of the testing performed.)
Upon request, providers can submit year-2000 test claims to their contractors, who will evaluate them for Y2K compliance. Left uncorrected, these problems could delay reimbursement and disrupt cash flow for Medicare providers in the year 2000.
New vaccine requirements
As of June 1, under the National Childhood Vaccine Injury Act, all health care providers who administer vaccines must provide patients or their guardians with copies of the relevant Vaccine Information Statements, produced by the CDC. The information sheets must be presented prior to each dose of vaccines containing diphtheria, tetanus, pertussis, measles, mumps, rubella, polio, hepatitis B, haemophilus influenzae type b (Hib) or varicella.
The act also requires that providers document in the patient's chart the date the materials were provided to the patient or guardian and the edition date printed on the materials. Providers are still required to document the name, address and title of the individual who administers the vaccine, the date of administration and the vaccine manufacturer and lot number as well.
The Vaccine Information Statements are available from state health departments or at http://www.cdc.gov/vaccines/pubs/vis/default.htm.
Market for primary care physicians cools a little
The aggressive recruitment of primary care physicians that occurred during most of the 1990s may be over, but primary care physicians just out of residency should have no problem finding jobs, according to a recent survey by Merritt, Hawkins & Associates, a Dallas-based health care staffing firm. Fifty-three percent of the U.S.-trained, final-year primary care residents surveyed reported receiving 26 or more recruitment solicitations, down from 63 percent in 1997. “While primary care physicians can still find practices in most markets, the ‘feeding frenzy’ in primary care recruitment is over,” said Merritt's chief executive officer, Joseph Hawkins.
The survey also found a growing reluctance among residents to practice in a managed care environment and a preference for practicing in single- or multi-specialty groups.
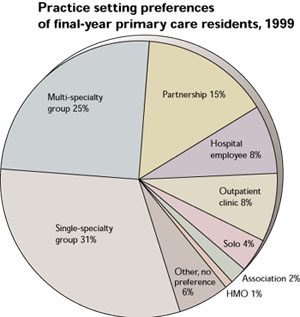
Source: Merritt, Hawkins & Associates, 1999 Survey of Final-Year Medical Residents.
Rural physicians face challenges in providing high-quality care
Physicians in rural areas practice in an environment that makes high-quality patient care difficult to provide, according to a recent report from the University of Missouri-Columbia, under the direction of E. Andrew Balas, MD, PhD. Balas' report summarizes the findings of several rural health research efforts.
Research has found that rural physicians spend on average 16 percent more time in direct patient care and perform 38 percent more patient visits per week, compared with their urban counterparts. In addition, rural physicians often do not have information and support systems to help them coordinate care. This extra workload takes time away from activities such as practice management, patient education and preventive care.
The result, say Balas and his colleagues, is poorer health care in rural areas. For example, rural women were screened for breast and cervical cancer 10 percent less frequently than urban women, and only 15 percent of rural patients with diabetes had received a glycosylated hemoglobin.
The researchers' proposed solutions include funding for quality improvement systems in rural areas, the promotion of evidence- based clinical practices and the use of telemedicine networks to improve access and coordination of care.
Quote. Endquote.
“By threatening not to pay for it [emergency department visits], you create what I call a ‘psychological co-payment.’ The jawboning and bullying reduces the use.”
Uwe Reinhardt, Princeton University health care economist, commenting in a July 20 Wall Street Journal article regarding managed care patients' use of the ED.