
Do you know what it costs your practice to provide an adult physical, a well-child exam or an office procedure? A “unit cost analysis” will tell you that and more.
Fam Pract Manag. 2004;11(4):41-45
A unit cost analysis is one of the most useful yet underused tools for managing a family practice. It takes into account all of the resources associated with providing a particular service and calculates how much it costs to provide that service at the smallest practical unit.1–3 For example, you might want to know the true cost of providing an adult physical exam, a well-child visit or a particular procedure.
Cost-per-unit data can be highly useful to you when developing budgets, setting fees, planning for expansion or negotiating rates with health care insurers. You may find, for example, that the true cost of providing an adult physical exam is significantly higher than the current reimbursement rate of a local health plan. You might then be able to use the data to negotiate a higher reimbursement rate, or at least decide whether the contract is worth renewing. Similarly, you may find that the costs of doing a certain procedure make it unprofitable given the level of reimbursement and the demand for the procedure.
In our recent experience at a medium-sized community health center in the Midwest, the unit cost analysis proved to be an insightful tool. It showed us, for example, that our laboratory expenses for patients with HIV account for about half of the cost of each of their medical visits. When this information was shared with a funding agency, it decided to increase its financial support of the clinic. The analysis also provided a foundation for further inquiries, including a time study of patient and staff work flow that will be used to improve the clinic’s efficiency.
While most physicians would agree on the theoretical utility of unit cost information, they might doubt the practicality of actually performing a unit cost analysis, fearing that it requires vast and expensive resources such as consultants, sophisticated computer systems or accounting training. Fortunately, these elements are not needed to conduct a unit cost analysis. By following the steps provided below, you can acquire valid and actionable cost information about the care you provide regardless of practice size or resources.
KEY POINTS
Knowing the costs of your services can help you with setting fees, planning for the future and negotiating better rates with health plans.
A unit cost analysis does not require sophisticated computer systems or accounting training.
Family physicians can use a unit cost analysis to determine the true cost of providing an adult physical exam, a well-child visit, a particular procedure, etc.
Six steps to a unit cost analysis
Unit cost analysis is fairly straightforward. The most important thing to remember is that you can and should modify the methodology where necessary for your organization. In doing so, bear in mind that you are not striving to produce a publishable analysis that will stand up under peer review. Instead, you are simply trying to obtain accurate cost information that will enable sound management decisions.
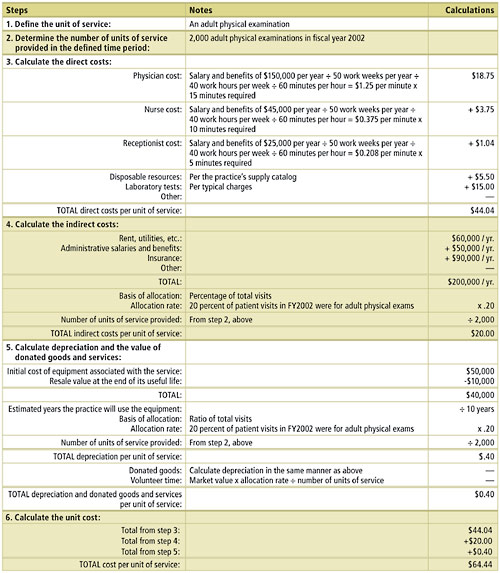
The sample unit cost analysis provided in this article will help illustrate how each of these steps can be applied in the real world. Both the example and this article take a “bottom up” approach (that is, you start by determining all of the individual costs associated with a unit of service and then add them together to determine the cost per unit). Practices with more sophisticated information management systems may be able to take a “top down” approach (that is, you start with the total costs associated with a service and then divide by the number of units of service provided to determine the cost per unit). Each of these methods will lead to the same destination (the cost per unit); they simply have different ways of getting there.
Step 1: Define the unit of service. The first step in a unit cost analysis is to identify the type of service whose cost you want to know. Common units of service are office visits, adult physicals, diabetes check-ups, well-child exams, etc. How you define a unit of a given service should be based on what is meaningful, familiar and useful to your practice. Your staff, for example, may be used to thinking about office visits in 15-minute intervals. This definition will be important when you begin to figure the costs of physician time, nurse time and support staff time associated with the service. Using familiar definitions will make it easier to acquire information, communicate findings with your staff and translate your results into action.
Another consideration in choosing and defining your units of service is your information management system. If your units of service correspond with data already captured by your computer system, it will be easier for you to find the data you need and analyze your practice’s costs. For example, if your computer system tracks claims better than visits, you might choose to calculate the costs of preventive medicine services coded 99381 to 99429.
Units of service can be further segmented, as needed, to provide more detailed cost data about particular types of patients. Patients for whom English is a second language, for example, may require the presence of an interpreter during their regular office visits as well as extra time with their physician. Likewise, patients being treated for chronic diseases may require more time with the physician, more lab tests or more nurse time devoted to patient education. By breaking down your units of service into these smaller components, you can identify costs that might be missed by looking at only the average costs of all patients.
Step 2: Determine the number of units of service provided. In determining the number of units provided, you will need to choose a time period to analyze and must adhere to this period throughout your analysis. Practices with a computerized practice management system should be able to produce the number of units of a particular service provided during a given time period fairly easily. Practices without a computerized system can use a basic chart audit to produce a reasonable estimate. Again, the goal is to acquire the most valid and reliable information available with the staff time and resources available.
Step 3: Calculate the direct costs. Direct costs are expenses you can easily relate to the provision of a specific service. Examples of direct costs include physician and support staff salaries and benefits, medical supplies, lab tests and other resources consumed at the time of the service. Unit costs are likely to be more sensitive to direct costs than any other component of the analysis, so a careful and detailed approach is crucial.
The largest and most important direct cost is often the physician time allocated to one unit of service. This component can be determined through one or a combination of four methods: 1) direct observation of physician activities; 2) time sheets or time diaries that physicians fill out; 3) time sheets or time diaries that patients fill out; or 4) patient cycle times (from check-in to checkout) generated from a practice management system. Support staff time can be determined similarly. For example, by keeping a time diary for one week, a physician may find that he spends an average of eight minutes in the exam room with the typical adult patient. Using his salary or hourly wage as a reference, the physician could then determine his cost for those eight minutes. (See step three of the example.)
Cost information for other resources – such as materials, supplies and laboratory tests – that are consumed during a particular service can be obtained through several different approaches as well. Often a discussion with the physicians or staff familiar with the resources used to provide the service will be sufficient. Reviews of invoices and budgets for the time period or direct observation can also be helpful in tallying the resources directly consumed. For example, to determine the resources associated with a typical office visit, your nurse might simply make a list of the items commonly used and consult the practice’s supply catalog to determine their costs.
Step 4: Calculate the indirect costs. Indirect costs are expenses shared by more than one area of the practice. These costs involve resources that are not directly consumed during the provision of a service, but without them the provision of that service would not be possible. Common examples include administrative staff salaries and benefits, facility costs, insurance premiums, office equipment and supplies, and marketing expenses.
To calculate the indirect costs associated with a particular service, begin by making a list of all indirect costs within the practice (e.g., rent and utilities = $60,000 per year; administrative salaries and benefits = $50,000 per year; malpractice and general liability insurance = $90,000 per year). Then, total these indirect costs (e.g., $200,000 per year). Next, decide how much of the practice’s indirect costs should be allocated to the service in question. Common bases for allocation include the ratio of the selected service to all services provided, the percentage of total revenue attributed to the service, the percentage of practice square-footage devoted to the service, or the percentage of the organization’s total direct costs attributed to the service. For example, the fact that 20 percent of a practice’s visits are adult physical exams can be used as a rationale for attributing 20 percent of the practice’s indirect costs to adult physical exams. (See step four of the example.) Often, more than one potential basis for assigning indirect costs will suggest themselves. In such cases you’ll simply want to decide which one makes the most sense for your practice as a whole.
Step 5: Calculate depreciation and the value of donated goods and services. Before you can figure the full cost of providing the service in question, you must incorporate estimates for depreciation and the value of any donated goods or services. Overlooking these expenses may lead you to underestimate long-term expenses, and it may impede long-range planning. “Straight line depreciation” is one generally accepted – and perhaps the most straightforward – way of calculating this cost. Take the initial cost of the equipment and subtract its estimated resale value at the end of its useful life (e.g, $50,000 - $10,000 = $40,000). Divide this number by the years you expect your practice to use the equipment (e.g., $40,000 ÷ 10 years = $4,000). Using a cost allocation similar to the one used in step 4, determine the amount of depreciation attributable to the service (e.g., $4,000 x .20 = $800). Divide this number by the number of units of service provided in the study time period to arrive at a depreciation cost per unit of service (e.g., $800 ÷ 2,000 adult physical exams per year = $0.40 per adult physical exam).
Some clinics also rely on the use of donated goods or volunteer services, and the market value of these items (i.e., the amount you would have had to pay to acquire the donated goods or services) should be included in your cost calculations. Since these resources may not always be available to a practice, the costs of replacing them to maintain current service levels can be significant. Documenting the financial importance of these donations can also be valuable for organizational fundraising and planning.
To calculate depreciation for donated goods, use the formula described above for depreciation of non-donated equipment. To calculate the cost of donated services, multiply the market value of the services by the allocation rate, and then divide by the number of units of service provided (e.g., $10,000 x .20 ÷ 2,000 adult physical exams provided per year = $1.00 per unit of service).
Step 6: Determine the full cost of the unit of service. This final step is the simplest: Add the costs from steps 3, 4 and 5 to arrive at a total cost per unit of service. In the example, the final cost for an adult physical examination was $64.44.
AN EXAMPLE: CALCULATING THE COST OF PROVIDING AN ADULT PHYSICAL EXAM
Family physicians in a two-person practice would like to know the true cost of providing an adult physical exam in their office. The practice wants to determine whether a private insurer is compensating them adequately and whether they should try to negotiate a better reimbursement rate.
Using data for fiscal year 2002, the physicians completed the following unit cost analysis. The practice also kept time diaries for one week to determine the physician and staff time required for an average adult physical examination.
In the end, the physicians found that an average adult physical examination costs $64.44.
Lessons learned
As family medicine continues to be practiced in a financially hostile health care environment, the need for accurate and actionable cost data has never been greater and will only increase in the future. A unit cost analysis can reliably yield this information and is a valuable tool for any family practice seeking to improve its management, efficiency and planning. By using an effective but realistic approach based on the six steps listed in this article, even the most resource-poor organizations can design and conduct a unit cost analysis that will help managers make the sound decisions needed not only to survive – but to succeed – within this environment.