
Fam Pract Manag. 2005;12(9):23-26
Aetna goes public with physicians’ payment rates
In industries from airlines to home improvement, consumers pay attention to prices and are able to shop around. That hasn’t been the case in health care, until now. Aetna recently posted on its Web site the reimbursement rates it has negotiated with every physician in the Cincinnati area for common procedures and tests. Aetna is the first major health insurer to publicly disclose its rates and has said it hopes to duplicate this in other parts of the country, a move that will likely encourage other insurers to follow suit.
The company says the purpose of its recent action is to help patients make better decisions regarding their health care dollars. Price transparency could pave the way for consumer-directed health plans, which involve high-deductible policies and medical savings accounts.
P4P programs should offer true bonuses, says panel
A panel of health care leaders recently advised the Medicare Payment Advisory Commission (MedPAC) that any pay-for-performance program implemented by Medicare should offer true bonuses for meeting quality standards. MedPAC’s current plan would increase payments to high performers by 1 percent to 2 percent and would decrease payments to below-average performers.
Samuel Nussbaum, MD, chief medical officer for Well Point, cautioned that payment reductions could prohibit physicians from making infrastructure improvements that would boost performance. He also noted that “bonuses” of 1 percent to 2 percent would not be effective and recommended 10-percent bonuses for primary care physicians.
Are you giving patients more care than they want?
More than half of U.S. adults have chosen not to follow their physician’s recommendations because they were “unnecessary or too aggressive,” according to a recent Wall Street Journal Online/Harris Interactive poll of 2,286 adults nationwide. Respondents cited malpractice concerns, patient demands and the desire to earn more as key reasons doctors sometimes over treat.
OTHER FINDINGS
32 percent of U.S. adults have chosen not to fill a prescription they considered unnecessary,
21 percent have sought a second opinion because they thought their doctor’s recommendations were too aggressive,
16 percent have chosen not to undergo recommended diagnostic tests they considered unnecessary,
10 percent have chosen not to undergo recommended 10 surgical procedures,
9 percent have changed doctors because they felt their 9 doctor’s approach was too aggressive.
Quote. Endquote.
"Unless everyone is completely clear about the tasks that must be done, exactly who should be doing them, and just how they should be performed, the potential for error will always be high."
- Steven J. Spear, MD, senior fellow at the Institute for Healthcare Improvement, in "Fixing Healthcare From the Inside, Today," Harvard Business Review, September 2005.
Committee addresses hassles of verifying patients’ insurance
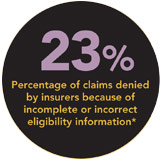
The process of verifying patients’ health coverage, co-payments and deductibles can be time-consuming and costly for physicians’ offices. But the Committee on Operating Rules for Information Exchange, made up of more than 50 health care organizations, including the AAFP, is hoping to change that. Convened by the Council for Affordable Quality Healthcare, the committee foresees a system in which physicians’ offices would be able to use an electronic system of their choice to access coverage information for any patient from any participating health plan at the point of care.
The committee is currently working to develop operating rules that will facilitate secure, electronic exchange of information, and it intends to have these rules in place by the end of 2005.
Small practices may profit from EHRs, says study
Solo or small-group practices may benefit financially from implementing an electronic health record (EHR) system, according to a report in the September/October issue of Health Affairs.
In the study, researchers assessed the costs of using EHR software, obtained from two vendors, at 14 solo or small-group primary care practices. Initial EHR costs averaged almost $44,000 per full-time-equivalent (FTE) provider, while ongoing costs averaged $8,400 per FTE provider per year. But financial benefits of using the EHR averaged $33,000 per FTE per year, mostly through increased coding levels, decreased staff costs, transcription savings and paper savings.
EHR implementation required physicians to work longer hours for four months, on average, as the staff learned the new system, entered patients’ data and made necessary process changes. After implementation, physicians benefited from being able the see the same number of patients in less time and from being able to access records from home. This enabled them to go home earlier, spend time with family and complete record review in the evening. It also improved their on-call experience.
Concerns over inappropriate screening tests spark ethical guidelines
The proliferation of direct-to consumer diagnostic imaging tests, such as full-body scans, which have not been scientifically validated, has raised questions about the appropriate use of such services. To help physicians practice ethically in this regard, the AMA’s Council on Ethical and Judicial Affairs recently offered the following guidelines (http://www.ama-assn.org/go/cejareports):
When offering a diagnostic test, obtain informed consent. This requires disclosing the nature of the test, benefits, risks and alternatives.
Explain that detection of a condition may have no effect on morbidity or mortality; therefore, testing may not be desirable.
Discuss test results and follow up with the patient even if there are few or no options for treatment.
Do not provide unnecessary tests. Services should be based on “scientific evidence, sound medical judgment, relevant professional guidelines, and due concern for economic prudence, as well as patient preferences.”
New resource offers Rx help for needy patients
After just 100 days of operation, the Partnership for Prescription Assistance has helped about 600,000 needy patients receive free or discounted medications. The service simplifies the process of finding and enrolling in drug-assistance programs by offering a single point of access to more than 475 public and private patient assistance programs, including more than 150 programs offered by pharmaceutical companies. Patients, physicians and staff can access the service online at http://www.pparx.org or by phone at 888-4PPA-NOW (1-888-477-2669).
The Pharmaceutical Research and Manufacturers of America helped launch this service in April. The AAFP is a founding partner.
Primary care sees larger pay jump than other specialties
While physician compensation was relatively flat in 2004, primary care physicians saw larger gains than specialists for the first time in several years, according to the Medical Group Management Association (MGMA) Physician Compensation and Production Survey: 2005 Report Based on 2004 Data. Primary care physicians’ compensation increased 3.13 percent in 2004, while other specialists’ compensation increased just 0.18 percent.
Family physicians saw a 2.32 percent increase in median compensation to $156,011; pediatricians saw a 1.47 percent increase to $161,188; and internists saw a 5.36 percent increase to $168,551.