
This encounter form can help you to prevent minor operations from becoming major billing headaches.
Fam Pract Manag. 2005;12(9):47-50
Skin procedures are among the most complicated services that family physicians have to code. Many who otherwise do their own coding prefer to delegate this job to someone else. But even if someone else is doing your coding, you have to know the rules, use the correct terminology and pay attention to detail to ensure that your documentation leads your coding staff to the correct code. Remember: They can’t read your mind – only your documentation. In my experience, the most effective strategies are familiarizing yourself with the most common pitfalls in skin coding and using an encounter form designed to help you document skin procedures correctly.
Costly coding mistakes
In a recent review of coding at local practices representing about 75 physicians, I noticed a number of coding mistakes that appeared repeatedly, including the following:
Incorrectly documenting the details of the procedure, such as the size or location of the lesion, the number of lesions, the length of the laceration, the type of skin closure, whether debridement was performed or the size of margins excised.
Submitting one code when two or more codes should be used, such as when two or more biopsies are performed, when two to 14 plantar warts or keratoses are treated, when more than 15 skin tags are removed, and when deep layering or undermining is used to close an excision.
Using the wrong codes. For example, it is incorrect to use flat wart codes 17110 and 17111 for plantar wart treatment, or to use biopsy codes when the lesion is completely excised.
Improperly documenting the patient’s complaint (e.g., pruritic, bleeding or painful lesions) or your reason for removing the skin lesion (e.g., suspicious for malignancy). This can result in denial of payment from Medicare or private insurance carriers because they don’t pay for “cosmetic surgery.”
Using incorrect terminology to describe what you did, such as biopsy when what you really did was shave.
IS IT COVERED?
Medicare does not cover cosmetic surgery. Unless a benign skin lesion is a threat to the patient’s health or function, its removal isn’t considered medically necessary. Medicare reimburses skin tag, seborrheic keratosis, wart and flat wart removal only if they are bleeding, painful, very pruritic, inflamed or possibly malignant. Treatment of molluscum and pre-malignant lesions such as actinic keratosis are covered. It is best to document both the patient’s symptoms and your physical findings to avoid denials.
The encounter form
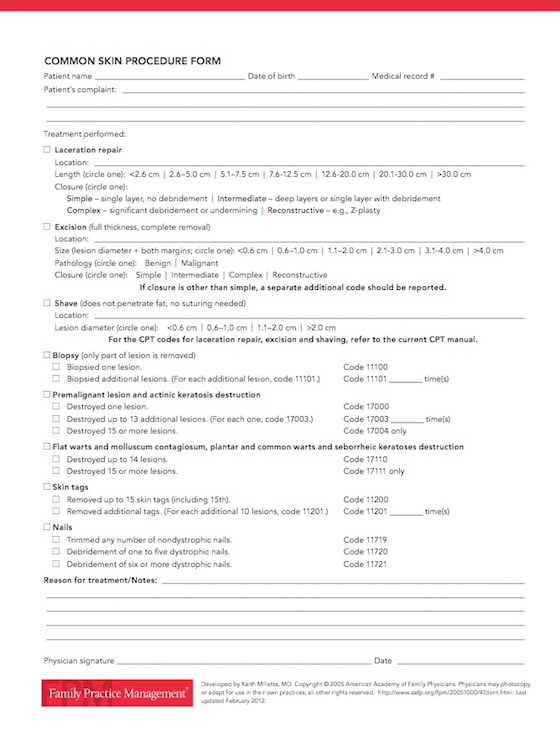
To simplify documenting and coding skin procedures, I’ve developed an encounter form that highlights the most common scenarios. While using the form, it’s important to keep the following in mind:
The CPT codes for laceration, excision and shaving are not on the form because of space limitations. They can be found in the current CPT manual.
Excision, shave, biopsy and destruction of warts are listed in order of declining reimbursement. So if you code for shaving when you actually excised the lesion, or if you code for biopsy when you completely excised the lesion, you are penalizing yourself by not using the correct terminology.
The form can look a bit daunting at first, but the following reminders should help you put it to good use:
Laceration repair. Be sure to document the laceration’s size, location and the wound closure. Measure the length of the laceration in centimeters. If multiple lacerations of similar types are repaired in the same body area, add those lengths together. Closure is classified as simple, intermediate, complex or reconstructive. Simple closure is a single-layered closure with no significant debridement. Intermediate closure involves putting in deep layers, or it can be a single layer with some debridement required. Complex closure can include extensive debridement or undermining. Reconstructive closure involves adjacent tissue transfer or rearrangement (e.g., Z-plasty).
Excision. This procedure involves completely removing the skin lesion by cutting completely through the dermis (full-thickness removal). Be careful not to use the term “biopsy” or “punch biopsy removal” in your documentation or a second party may incorrectly code the procedure as a biopsy, which would result in less reimbursement. Record the size of the lesion as the lesion’s maximum diameter plus the sum of the narrowest margins used to excise the lesion. To assign the proper code, you’ll need to hold off on billing until you know whether the lesion is benign or malignant. Excision of a malignant lesion is reimbursed at a higher rate. If something other than simple closure (e.g., intermediate or complex closure) is needed to repair the excision, don’t forget to code for closure in addition to the excision.
Shave. This procedure involves horizontal cutting to remove a lesion. It is not a full-thickness excision; it does not penetrate the fat layer. The wound does not need suturing. The lesion’s location and size needs to be documented before you can assign the proper code.
Biopsy. Bill for this when only part of the lesion is removed to obtain tissue for pathology. If the entire lesion is removed, use excision codes instead. Submit 11100 for the first biopsy. For each separate biopsy after the first one, use add-on code 11101. For example, if three lesions are biopsied, you would submit codes 11100, 11101 and 11101 again.
Plantar wart and keratosis destruction. The treatment of common warts, plantar warts, actinic keratosis and seborrheic keratosis by most methods (application of acid, freezing, laser or electrocautery) is covered by “destruction” codes. Use 17000 for destruction of the first lesion. Use add-on code 17003 for each lesion between two and 14. For example, if you treat four lesions, submit codes 17000, 17003, 17003 and 17003. Many times code 17003 is incorrectly submitted only once when more than two lesions are removed, resulting in lost reimbursement. If you remove 15 or more lesions, submit only code 17004.
Flat wart and molluscum contagiosum destruction. Use codes 17110 and 17111 for treatment of fl at warts and molluscum by any method. If you treat between one and 14 lesions, submit 17110. If 15 or more lesions are treated, submit only code 17111.
Skin tags. For removal of skin tags by any method, use codes 11200 and 11201. For the first 15 skin tags removed, use code 11200. For each additional 10 skin tags removed, also report code 11201. For example, if you removed 35 skin tags, then you would submit codes 11200, 11201 and 11201.
Nails. For trimming of any number of nondystrophic nails, use code 11719. For debridement of dystrophic nails by any method, use code 11720 if one to five nails are treated. Submit code 11721 only if six or more nails are debrided.
COMMON SKIN PROCEDURE FORM
Note: This tool has been updated since its original publication date. Download the most current version below.
Clear coding
As you begin to master the rules for coding skin procedures, your documentation will be more thorough, your billing will be more accurate and your reimbursement will begin to approach the correct level. Until then, confused coding could be costing you reimbursement you deserve.