
Who needs an EHR? Software you already have can help you make sure your patients get the care they need.
Fam Pract Manag. 2006;13(4):47-52
Dr. Ortiz is a family physician and flight surgeon at the 59th Medical Squadron at Brooks City-Base, Texas. He is also a clinical assistant professor with the Department of Family and Community Medicine at the University of Texas Health Science Center in San Antonio. The author would like to thank Brian Costello, MPAS, PA-C, for his assistance in developing this article. The opinions and assertions in this article are the author’s private views and are not to be construed as the official position of the U.S. Air Force Medical Service or the Department of Defense. Author disclosure: nothing to disclose.
Better patient outcomes. Improved chart legibility. Increased revenue from better coding. Easier disease management. These are just some of the reasons why family physicians have been advised to purchase an electronic health record (EHR) system. Unfortunately, EHRs can cost tens of thousands of dollars per doctor, which many practices simply cannot afford. However, there are ways to improve your clinical practice without purchasing an EHR. Since most practices, even small ones, already have computers that staff members use for word processing, billing and common office applications, it makes economic sense to use these tools for more than just business operations and mailings. Using readily available computer tools, you can improve your care.
Population health and disease management
One of the great improvements in practice that an EHR enables is the ability to manage chronic illness in a proactive, organized fashion. Many physicians without EHRs take a passive approach: They wait for patients who are chronically ill to show up at their practice with an acute problem, and then they address any chronic disease issues at that time or reschedule the patient for another visit dedicated to the chronic illness. This approach has several disadvantages when you think of your patient population as a whole. It neglects patients who rarely visit the practice and delays chronic disease management until the patient arrives at your doorstep.
But what if you could keep track of all your patients with diabetes, including their required labs and preventive services, and use that information to manage your patient population proactively? Most commercial EHRs can do this, but it can also be done by using a commercially available spreadsheet program, such as Microsoft Excel, or a database program, such as Microsoft Access. For example, using a spreadsheet program, you can easily create a list (or registry) of your practice’s patients with a given chronic disease and then use that list to track key measures and remind you and your staff automatically when patients need certain labs and preventive services. Such lists can be accessed and managed by anyone on your staff (including nurses, medical assistants and administrative staff) with minimal training.
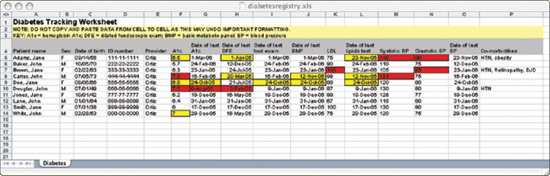
For a readymade diabetes registry, you can download the Excel file in this article. This registry, a version of the one we use in my practice, tracks a number of interventions and clinical parameters important in diabetes management and alerts you if there are problems. For instance, if the date of a patient’s last A1C was more than 90 days ago, that date cell turns yellow as a warning; if more than 180 days ago, it turns red. Additionally, if a patient’s A1C is outside of the normal range, the corresponding data cell will also change colors. These visual cues allow staff members to scan the worksheet and quickly identify which patients are due for which service. To begin using the registry, just delete the sample patient data shown and start collecting the equivalent information on your patients with diabetes.
If you want to create your own registry from scratch, you need only a basic familiarity with Excel. Create a new file and start entering the names of patients who have the chronic illness you’re focusing on. You can identify this population by screening patients as they arrive for visits, by reviewing billing records and by doing chart audits, and you can add names as you go along. Next, decide what interventions you want to track. Then create columns for the interventions and enter the dates when the patients last received each service.
You can design the spreadsheet to alert you (by changing the color of a cell in the worksheet) when the service is overdue or when a given marker is above a certain threshold (e.g., A1C above 7.0). This feature is called “conditional formatting” in Excel and is fairly easy to set up, with some practice. To see how it works, click on any of the colored cells in the downloaded sample spreadsheet. Click the Format menu and then select Conditional formatting. You will then be able to view the formulas in the cell you have selected. Using the formulas from the sample worksheet or variations on them, you should be able to apply conditional formatting to selected cells in your new file.
Once you’ve created the worksheet, save it somewhere on a computer or on the practice network where any staff member who needs to can access it. This will make it easy for staff members to review the information – weekly or monthly, depending on your practice’s volume of patients with a given chronic illness – and then notify patients when a given service is due. The worksheet can be updated periodically as laboratory results or consultant reports come in, as new patients with the given diagnosis join the practice or as practice standards change.
This tool can also be used for preventive services (e.g., Pap smears, mammograms or colon cancer screenings) for the general patient population. As patients join your practice, staff members can enter their demographic information into similar worksheets that will highlight when a preventive service is due.
The most difficult part of creating these worksheets is the initial data entry. This can be done over several months by assigning the job to a specific staff member or by hiring a part-time data-entry clerk to perform the job. Once you have created the initial worksheet, you can assign the maintenance aspects to any staff member, who will need to be trained only on how to update the worksheet and how to contact patients when services are due.
A SAMPLE DIABETES TRACKING WORKSHEET
The diabetes tracking worksheet used by the author’s practice is shown here. Click below to download the worksheet.
Putting it into practice
Four years ago, our clinic’s parent health care organization dictated that all of its satellite clinics would be required to implement clinical practice guidelines for chronic diseases and show measurable improvements in patient care. After convening a few brainstorming sessions in which all members of our clinic (physicians, nurses, medical assistants and administrative personnel) participated, we elected to implement a chronic disease tracking system like the one mentioned above. We already had a computer server that all members of the clinic could access, so a computerized tracking system made sense for our practice. We used Microsoft Excel and created a list of our practice’s patients with type-2 diabetes mellitus, since we had a large number of patients with diabetes in our practice. We chose to monitor six diabetes target values: blood pressure, lipids, foot exam, eye exam, immunizations and A1C.
The hardest part of the process was identifying all patients in our practice who had type-2 diabetes. All members of the clinic staff helped identify those patients using billing records, chart audits and daily patient screening. By spreading out the work among nurses, administrative staff, physicians and medical assistants, we created a team effort and a sense of ownership over the process. We also spread out the work over several weeks, with each staff member auditing 10 to 15 charts per day to look for patients who have diabetes, so as to not overwhelm the staff and to continue daily operations. As we identified patients with diabetes, we would enter them into our database and record the last charted measurements of each of the target values we wanted to improve (last eye exam, last A1C, etc.). As we identified these values, the staff would contact patients who were overdue for any exams or services to get those accomplished. We programmed our worksheet to change the color of cells to indicate values or services that need to be addressed for each patient.
After a few months, we had our first tracking worksheet completed. We then assigned the monitoring of the system to a team member who would be responsible for checking the worksheet monthly and contacting patients to remind them of any needed services. As we received laboratory results or consult reports, staff members would make the appropriate entry into the worksheet. By using this system, we were able to increase our compliance with recommended services. Our patients also appreciated the reminders and the attention from our staff, which increased our patient satisfaction numbers as well.
Over the course of a year, we chose several other chronic diseases (hypertension, hyperlipidemia and asthma) and created similar tracking systems for each of them as well. After getting our chronic disease tracking systems going, we created worksheets for all of the patients enrolled in our practice, not only those with chronic diseases. We chose several preventive services (mammograms and Pap smears to start) and began using the same tracking techniques to improve our compliance with those services as well. While we had several problems that were outside our control (e.g., mammography services are not readily available in our practice setting, so it was difficult to order mammograms and get timely results), our overall preventive service compliance rate increased over time. Working with this system eventually helped our practice achieve the highest preventive services compliance rates of all outpatient clinics in our organization as measured by our parent health care organization.
Bottom line
Clearly, an EHR can provide the same advantages and more with less effort than the approach described above. However, physicians in small practices may not be able to afford EHRs. As physicians face increasing demands to improve care and document their performance as part of pay-for-performance initiatives, even those who can’t afford to buy an EHR will need to find ways to improve the quality of care they provide. This article demonstrates how family physicians can do just that, using some common computer tools without making a huge investment in an EHR.
As with all changes, it’s best to start small and pick one area or disease that you want to improve. Involve your whole staff and come up with a plan that everyone agrees to, then implement the changes and make modifications as you go along. You’ll find that the effort will pay off in the end with healthier patients and happier staff.