
More and more health plans are grading physicians on their performance. Now, it’s time for physicians to grade their health plans.
Fam Pract Manag. 2006;13(9):55-59

Physicians, sharpen your red pencils.
As health plans increasingly attempt to grade you on your quality of care, your prescribing patterns and your coding levels, it seems fair to finally turn the tables. The AAFP and Family Practice Management are launching a nationwide online survey that enables family physicians to grade individual health plans on their payment rates, claims processing, formularies and other factors. The responses will generate a massive payer report card, which will be published in the April 2007 issue of FPM. Based on physicians’ experiential data, the report card will help demonstrate which health plans are doing well and which need to improve their performance.
How it works
To participate in the payer survey, log on to https://www.aafp.org/fpm/payersurvey. The survey is currently open to AAFP members only; it requires input of a valid AAFP member ID number and password.
The AAFP/FPM Survey of Physicians’ Experiences With Third-Party Payers has four easy-to-complete sections:
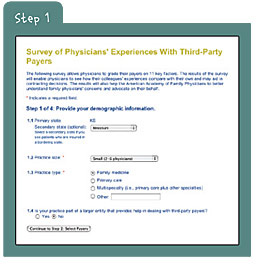
Step 1. Enter your demographic information (4 questions). Once you log in, your primary state will be prefilled, based on information pulled from your AAFP membership record. If the primary state isn’t correct, or if you provide care for patients insured in a bordering state, select a secondary state from the drop-down menu in question 1.1.
The three additional questions in this section address practice size, type and ownership.
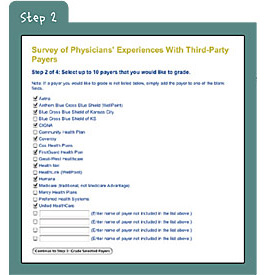
Step 2. Select your payers (1 question). You will be presented with a list of third-party payers that do business in the state or states you identified in step 1. From that list, select up to 10 payers that you would like to grade. Choose the payers you deal with most often and want to provide feedback on, both good and bad. Medicare (traditional, not Medicare Advantage plans) is included in the list as well.
If one of your payers is not included but you would like to grade its performance, simply add that payer to one of the blank fields and check the corresponding box.
Step 3. Grade your payers (11 questions). On a scale of A (excellent) to F (failing), grade each payer in your list, taking into account all products offered by that payer (HMO, PPO, etc.). You’ll need to assign grades in 11 categories:
Payment rates (whether they are adequate or too heavily discounted);
Adherence to Current Procedural Terminology (CPT) in claims processing (whether the payer recognizes modifiers, inappropriately bundles or downcodes services, etc.);
Timeliness of payments (whether clean claims are paid within an appropriate amount of time);
Accessibility, knowledge and responsiveness to your practice’s concerns (whether payer representatives are easy to reach, helpful, etc.);
Member eligibility and benefits information (whether it is accurate and easy to access);
The payer’s Web site (whether it provides accurate information and smooth transactions);
Formularies (whether the information is easy to access, how often it changes, etc.);
Prior authorization (how often it is required, how reasonable the decisions are, etc.);
The appeals process (whether decisions are timely, reasonable, etc.);
Physician performance data (whether data is accurate, valid and used fairly);
The contracting process (whether the payer is willing to negotiate, disclose its fee schedule, etc.).

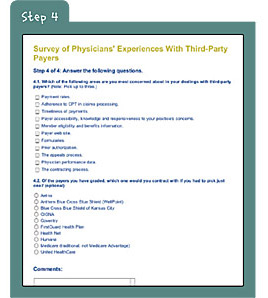
Step 4. Provide final responses (2 questions). In the final section of survey, you’ll be asked to select your top concerns related to payers and identify which payer you would contract with if you had to pick just one. You’ll also be able to submit general comments related to the survey. If you want to register a specific complaint about a specific payer, use the AAFP Health Plan Complaint Form at https://www.aafp.org/online/en/home/practicemgt/specialtopics/managedcare.html.
Using the report card
The payer report card we will develop from the survey results and publish in the spring will be useful on several levels. It will highlight both high-performing and low-performing payers and will help bolster the AAFP’s advocacy efforts on behalf of family physicians. It will also provide you with a tool to use in contracting decisions – as well as the satisfaction of turning the tables on your payers.
The point of the survey isn’t to condemn health plans but to provide honest input and comparisons that will aid physicians and spark positive changes in the physician-payer relationship. So log on to https://www.aafp.org/fpm/payersurvey, and spread the word to your colleagues. This is your chance to be heard and to wield the power of the red pencil.