
When patients need to be referred for counseling, these tips can ensure success.
Fam Pract Manag. 2012;19(1):36
Dr. McBride is director of behavioral medicine at Floyd Medical Center's Family Practice Residency in Rome, Ga. He is a credentialed pastoral counselor and licensed family therapist. Author disclosure: no relevant financial affiliations disclosed.
Family medicine has always been a discipline that looks at the whole person. While physicians in some fields of medicine can maneuver around psychosocial issues or pretty much ignore them regardless of their importance to the patient's health, family physicians must consider more than just the physical complaint.
A common struggle for family physicians, however, is finding time to fully address psychosocial issues. Utilizing a counselor is one option, but some physicians hesitate to do so because of past experiences where it did not go smoothly. Here are some pointers for improving referrals to a counselor:
1. Take time to prepare the patient. In many communities, counseling continues to have a stigma. Some patients may think that counseling is only for “mental cases,” so it is vital that you use appropriate language, such as “I would like for you to see the counselor for support in dealing with the stress in your life.” You may also want to suggest, “Try it one time, and see if it works for you.” Often, once the patient meets the counselor, he or she will return. It may take several months to persuade some patients to seek counseling, but don't give up.
2. Assure the patient that you are going to continue caring for him or her. It is important to guard against showing any frustration with the patient or with his or her psychosocial problems, which would suggest that you are simply attempting to get the patient out of your hair. Instead, seek to show compassion, and express your desire for the patient to see a counselor in the context of your goal that the patient receive the best overall care.
3. Establish a relationship with a counselor in your community. It is difficult to be genuinely positive about sending someone to see a counselor if you do not have some familiarity with the counselor. Ask around to identify good counselors in your community, and invite them to your office or to lunch. Ask about their knowledge of the stressors created by chronic illnesses or other clinical issues. And, of course, look at their credentials, including state licensure and membership in national organizations such as the American Association of Marriage and Family Therapists or the National Association of Social Workers.
4. Address confidentiality issues. As a general rule, counselors obtain written releases from patients in order to talk to other counselors or professionals about a patient. You may need to let the counselor know what you would like in terms of feedback about the patient and how often you want to receive updates.
5. Recognize that physicians and counselors operate differently. For example, the language counselors use can be different from what physicians are accustomed to (“client” versus “patient”). The counseling environment tends to operate at a slower pace, with most counselors refusing to be interrupted in the middle of counseling sessions unless it is an emergency. Also, change may not happen as rapidly with psychosocial issues as with physical issues.
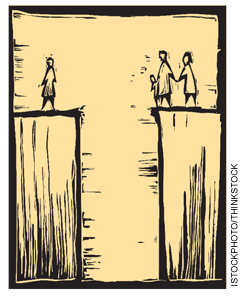
Understanding and anticipating these differences can lead to a better referral relationship and better outcomes for the patient. Just as in a relay race where the baton can be dropped and the race lost at the moment of transfer, the handoff between the physician and the counselor can determine success or failure. If done well, both you and your patients will greatly benefit.
