
Three principles helped this small primary care practice conquer the dreaded inbox and its mountain of messages.
Fam Pract Manag. 2012;19(5):25-29
Paula Eaton is practice administrator at Martin's Point Health Care-Bangor in Bangor, Maine. Author disclosure: no relevant financial affiliations disclosed.
Physicians face a barrage of messages every day – phone messages from patients, emails from consultants, faxes from pharmacies, reports from laboratories, sticky notes from support staff, and on and on. All of this information coming into the practice needs to be processed, routed, and acted upon promptly and efficiently. Failure to do so can result in patient dissatisfaction, delays, rework, and errors.
This article describes how our four-provider practice, Martin's Point Health Care-Bangor, decreased the hassle of managing messages and created a more efficient practice overall.
Guiding principles
Before I describe our processes for managing messages, I should offer some background, beginning with three key principles that underlie our work. First, every member of the practice needs to operate at the highest level of responsibility that their experience, ability, and licensure allows. Second, employees need to be given effective tools and training to help them succeed. And third, processes need to be standardized across the practice to ensure reliability and facilitate cross coverage.
These principles are lived out in our practice in a number of ways, most notably in our use of “patient service representatives” (PSRs). These individuals typically serve as the first point of contact patients have with our practice, but they are not your traditional medical secretaries. They are trained to be masters of phone and inbox management. Many of them come from medical backgrounds, but we've also trained individuals with backgrounds in banking, marine biology, and running a small business. Potential employees undergo a thorough interview process, which includes a full team interview, and job shadowing. Once hired, they take part in a proficiency based training process that includes six to eight weeks of one-on-one training and daily feedback. This helps them incorporate improvements and reach a high level of proficiency before they're finally allowed to manage the phones on their own. Their training focuses on three primary functions: the check-in/greeter function (verifying insurance, collecting copays, etc.), the scheduler function (scheduling diagnostic tests, referrals for consults, etc.), and the phone/triage function. This latter piece is the most challenging because our PSRs must learn to follow protocols that help them analyze patient symptoms for triage purposes and manage prescription refills. We access these protocols through a web-based clinical decision support tool called the Problem Knowledge Coupler. (See "An invaluable tool.") We make significant investments in training and equipping our PSRs, and the result is that we have highly competent, enthusiastic people on the front lines. This allows our providers (three physicians and one nurse practitioner), our nurses, and our other clinical support staff to operate at high levels as well. (See “An empowered support staff.”)
AN EMPOWERED SUPPORT STAFF
Our practice has eight highly trained and empowered patient service representatives that shoulder much of the messaging process, as the article describes. Our practice also uses other staff members to their maximum abilities.
We have two RNs who practice “collaborative care nursing.” Under this model, patients who are stable but are having difficulty managing their chronic conditions – for example, they can't get their A1C under control or they need more education or support – are scheduled with a nurse. The nurse provides education, does the intake, reviews medications, etc., and then the provider joins the visit and receives a report from the nurse. The provider performs the physical examination, talks to the patient about the assessment, creates a care plan, provides orders, prescribes medications, etc., while the nurse serves as a scribe. When the provider finishes, the nurse wraps up the visit.
Three MAs and an RN function as clinical support staff. They room patients, collect vital signs, review medications, check allergies, prep the chart, and even collect information regarding the patient problem. (To read about a practice that takes a similar approach, see “A New Approach to Making Your Doctor-Nurse Team More Productive,” FPM, July/August 2008.) Our EHR contains protocols for preventive care and certain diseases and provides a list of services due (e.g., a tetanus shot or a screening mammogram), so the clinical support staff can go ahead and create the order. The provider will later review and sign off on the order.
Our physicians and nurse practitioner are comfortable with this style of practice because they have confidence in our training and protocols. Having highly trained and empowered staff members allows them to stay focused on the problem, assessment, and plan, and it makes them highly productive.
The messaging process
With PSRs at the center of our messaging process, here's how the process works for common message types:
Phone messages. These are the most common and most straightforward messages we receive. When a patient or other caller contacts our office by phone, the PSR first attempts to take care of the matter directly, often with the assistance of protocols as described earlier. If the matter requires the expertise of another member of the practice team, the PSR brings up the electronic health record (EHR; we use Centricity), selects the “phone note” function, captures the key information (caller name, number, reason calling, etc.), and forwards the message to the correct person, typically the provider. When the provider opens the EHR, which occurs multiple times throughout the day, he or she is alerted that a message is waiting, including whether the message is urgent. If a provider is absent, whether planned or unplanned, another provider will cover that person's inbox for the day.
Emails from patients. We use secure messaging provided through Kryptiq, which we can access through our EHR, to exchange messages with patients. We can send the message from within the EHR because the patient's email address has been captured as part of our intake process. Surprisingly, even though our practice has an older population, 50 percent of our panel have provided email addresses and most seem willing to try new technologies. We can attach test results or other documents to the message as needed, and the email is saved into the record automatically. We educate our patients that the following types of communication are appropriate for secured messaging: prescription refill requests, appointment requests, nonurgent medical advice, nonurgent medical follow up (including certain test results), and nonurgent medical correspondence. Email is never appropriate for urgent or emergency medical problems, mental health issues, drug or alcohol problems, HIV/AIDS related issues and diseases, or work-related injuries and disability. Our providers report receiving only about five to eight emails a week, so they are not inundated as some might expect. Offering patients the option of using the secure messaging system frees the provider from time-consuming telephone follow up. We aim for a 24-hour turnaround for email replies and have found it to be doable.
We also have a general email box for the practice, which we access via Microsoft Outlook. Our PSRs monitor this account. Occasionally, patients use this general email address to contact us about clinical matters, but we educate them, to protect their privacy, that they need to use the secure messaging portal instead.
Refill requests. Refill requests come into our practice in several ways. A pharmacy might call, fax the request to our general email box, or send it electronically so that it appears in the provider's EHR inbox. The PSRs handle much of this work with the assistance of the refill protocols mentioned earlier. The requests then go to the provider for final signature.
Refill requests coming directly from patients are also handled by the PSR using protocols, with some exceptions. For example, if a patient calls to request a refill on a narcotic medication, which the PSR is not allowed to handle, the request is routed electronically to the provider as a phone message.
Test results. When test results come into the practice, often by fax or email, a PSR creates a message in the EHR including the reason for the test, who ordered it, pending appointments, and action needed, and routes it to the ordering provider to review. This puts the report in context, giving the provider all the information needed to assess the test results. For tests conducted at facilities that have an interface with our EHR, results arrive directly in the provider's inbox; however, each provider is assigned a PSR who monitors the inbox for such messages. Messages marked with a red exclamation mark by the testing facility are urgent; those with a yellow exclamation mark are important. If a result is critical, the testing facility will call, and the PSR will immediately locate the physician.
After the provider reviews the results, he or she can email the patient directly from the EHR indicating that everything is normal, call the patient if the results are abnormal, or message the PSR with follow-up instructions, such as sending the patient a letter or contacting the patient to schedule a follow-up visit.
Internal messages. Within the EHR, there is a feature called the flag. It is an internal communication tool that we use instead of physical sticky notes to communicate that a patient is upset about something, needs a form filled out, or has a special need. We can send a flag to one person or to multiple people, and when the recipient views any part of the EHR, the system will indicate that a flag or other message is waiting. Although it is attached to the chart, it will only become a permanent part of the record if we convert it to a note, which is rarely necessary. If a provider uses a flag to ask a clinical support staff member or PSR to order a test, for example, that would be converted into a note.
Face to face. Despite our electronic messaging tools, we sometimes need face-to-face conversations or even traditional sticky notes. Electronic systems do not obviate these modes of communication. If a matter is critical or we know that a provider isn't likely to be looking at his or her computer screen for a while, we do not hesitate to speak directly with one another. Likewise, we try to be mindful of our patients' needs and recognize when phone or face-to-face conversations with them may be more comforting or appropriate, even if they are not the most efficient option.
We also use team huddles to share information before beginning each day. These are brief face-to-face meetings involving all members of the office staff. Team members communicate issues that might arise during the workday, review staffing issues such as who is out sick or who has to leave early, and review each patient on the day's schedule.
AN INVALUABLE TOOL
The use of protocols and other decision support tools can enable practices to delegate symptom analysis, medication refills, standard treatments, and follow-up scheduling to nonmedical staff, depending on state laws regarding licensure. Our practice uses the Problem Knowledge Coupler for these functions. Below is the first screen the patient service representative (PSR) typically sees when a patient contacts our office.
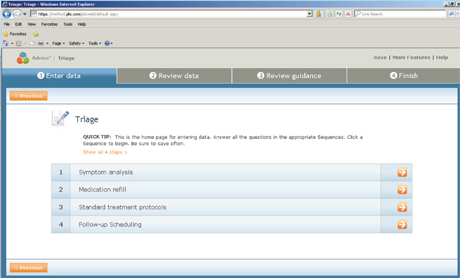
The next three screens show what the PSR sees if a patient contacts our office with a complaint of cough. The patient's symptoms guide the PSR to the appropriate action – in this case, scheduling the patient for a same-day, 15-minute appointment and checking with the provider about ordering a chest X-ray before the visit.
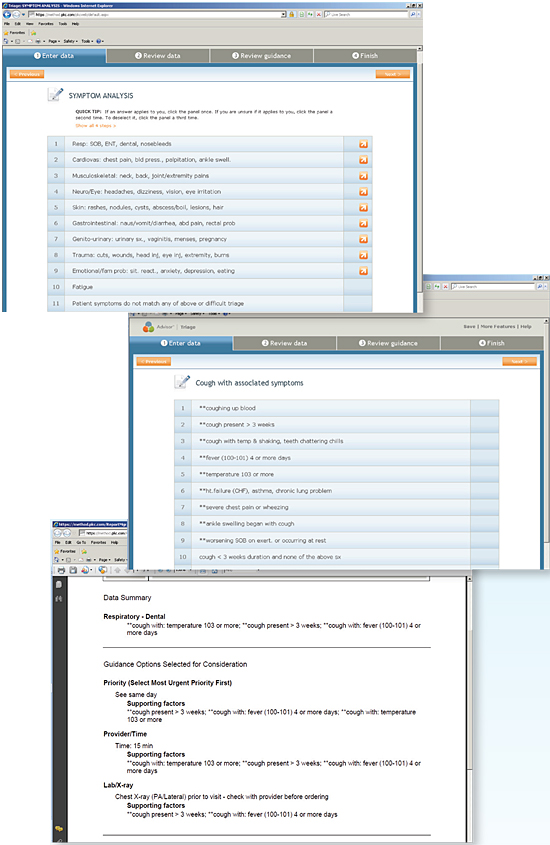
The purpose of these triage protocols is to enable nonmedical staff to effectively and safely assess patient complaints to determine the following:
Which patients need to be seen.
Where they should be seen (ED vs. office).
What level provider is appropriate.
How much time should be allowed for evaluation and whether testing should be obtained before the appointment.
This should not be perceived as a process to limit demand or limit access to the practice. If the patient does not need to be seen, detailed instructions are provided for home care and when to call again if there is no progress. In general, all patients with symptoms that are new and unexplained, severe, progressing rapidly, or persistent should be seen.
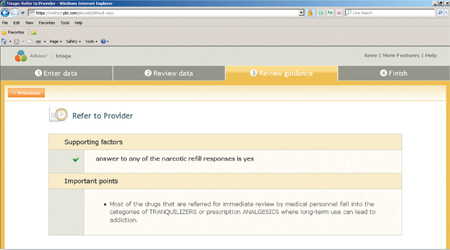
The final screen below shows an example of the medication refill screen the PSR sees if a patient contacts our office to request a narcotic drug. The recommended action in this case is “refer to provider.”
No turning back
With our use of technology, effective delegation, and extensive protocols, we have brought order to our messaging process. Our patients and visitors consistently remark that our practice runs smoothly and has a sense of calmness, and our providers and staff report high degrees of satisfaction. (Our practice's score on the Great Place to Work assessment was 100 percent last year.) Of course, getting to this point wasn't easy. Change is difficult, even if you've been at it for a while, but there is great satisfaction in improving the major areas of your practice – those systems that directly affect patients. Would we ever go back to the old way of managing messages? Not a chance.
