
Changing your EHR could lead to greater practice satisfaction – or not. The results of this survey may surprise you.
Fam Pract Manag. 2015;22(1):13-18
Author disclosures: no relevant financial affiliations disclosed.
Over the last several years, electronic health record (EHR) systems have become pervasive. Numerous surveys, including our prior surveys,1 have shown that overall physician satisfaction with EHRs is relatively low. Increasingly, physicians are changing EHRs or at least wondering if there are better EHRs out there. We embarked on this latest survey to answer three questions:
What key factors are driving practices to change EHRs?
What main challenges are they encountering along the way?
Does changing EHRs lead to improved EHR performance and user satisfaction?
In other words, we were interested in discovering why practices are changing EHRs and how they are finding the experience. We hope that the answers to these questions can better inform us all as we continue to struggle with the current technology.
Note that this latest survey is a departure from past FPM surveys, which provided user ratings of specific EHR systems across several dimensions of EHR performance and user satisfaction.1
Who responded?
As with our prior surveys of EHR user satisfaction, we published the current survey in Family Practice Management and invited family physicians who had recently switched systems to respond.2 Over the data-collection period (mid-July through September 2014), 438 physicians started the survey, but we had to eliminate 133 responses for failing to complete key questions or failing to meet at least one criterion of participation. We were looking for respondents from practices that had changed EHR systems in recent years (2010 or later). We had to exclude 13 responses from physicians who had changed from paper records to an EHR, nine from physicians who had changed EHRs simply by changing practices, and 111 from physicians who didn't name an identifiable EHR.
Of the remaining 305 respondents, 50 percent worked in practices owned by a hospital, health system, or university; 41 percent worked in physician-owned practices; 4 percent worked in federally qualified health centers; and the rest worked in a variety of other settings. While 24 percent worked in practices with at least 100 physicians, 21 percent were in solo practice. Respondents divided almost equally between practices of up to nine physicians and practices of 10 or more physicians.
As with any non-randomized survey, our results should be interpreted with caution. We do not know how representative our 305 usable responses are of the universe of family physicians who have changed EHRs since Jan. 1, 2010.
Changing from what to what?
The 305 respondents in the analysis group named a total of 41 EHR systems as their current systems and a total of 73 EHR systems as their previous systems – the difference in numbers presumably an indication of market consolidation. In fact, 25 EHR systems accounted for 82 percent of the “previous system” responses, while only 11 EHR systems accounted for the same percentage of “current system” responses. (See “The most commonly reported EHR systems.”) Given all the systems mentioned, it's not surprising that the respondents detailed a total of 198 different “from-to” pairs, and even the most common switch (from Centricity EMR to EpicCare Ambulatory) was mentioned by only 17 respondents.
THE MOST COMMONLY REPORTED EHR SYSTEMS
Of the 305 respondents in the analysis group, 251 (82 percent) previously used at least one of the 25 systems in the left column. Similarly, 251 respondents (not necessarily the same 251) now use one of the 11 systems in the right column. The shorter list and generally larger user numbers in the right column suggest considerable consolidation of the EHR market.
| Previous systems (most common EHRs switched from) | Current systems (most common EHRs switched to) |
|---|---|
| Centricity EMR (N = 30) | EpicCare Ambulatory (N = 74) |
| eClinicalWorks (N = 27) | eClinicalWorks (N = 34) |
| Allscripts Professional EHR (N = 22) | Praxis (N = 30) |
| NextGen Ambulatory EHR (N = 22) | Allscripts Professional EHR (N = 18) |
| Practice Partner (N = 18) | NextGen Ambulatory EHR (N = 18) |
| Misys EMR (N = 14) | athenaClinicals (N = 17) |
| Allscripts Enterprise (N = 13) | Cerner Millennium PowerChart/PowerWorks (N = 15) |
| athenaClinicals (N = 11) | Allscripts TouchWorks EHR (Allscripts Enterprise) (N = 13) |
| EpicCare Ambulatory (N = 11) | Practice Fusion (N = 12) |
| SOAPware (N = 10) | Amazing Charts (N = 11) |
| Proprietary systems (N = 8) | e-MDs (N = 9) |
| e-MDs (N = 8) | |
| Cerner Millennium PowerChart/PowerWorks (N = 7) | |
| Practice Fusion (N = 7) | |
| Allscripts MyWay (N = 6) | |
| Amazing Charts (N = 6) | |
| ChartConnect (N = 6) | |
| Horizon Ambulatory Care (N = 5) | |
| McKesson Practice Complete (N = 4) | |
| Praxis (N = 4) | |
| Centricity Practice Solution (N = 3) | |
| MPM (LSS/Meditech) (N = 3) | |
| AHLTA (N = 2) | |
| Amicore PenChart (N = 2) | |
| CGM Clinical (N = 2) |
While our sample is too small to suggest winners and losers in the EHR marketplace, we do see some suggestive numbers. EpicCare Ambulatory and Praxis had the most net gains in customers among our respondents, with net increases of 63 users and 26 users respectively. Centricity EMR, Misys EMR, and Practice Partner had the greatest net losses, with drops of 27, 14, and 12 users respectively. Some losses may be due to EHR mergers or acquisitions.
Why did they change?
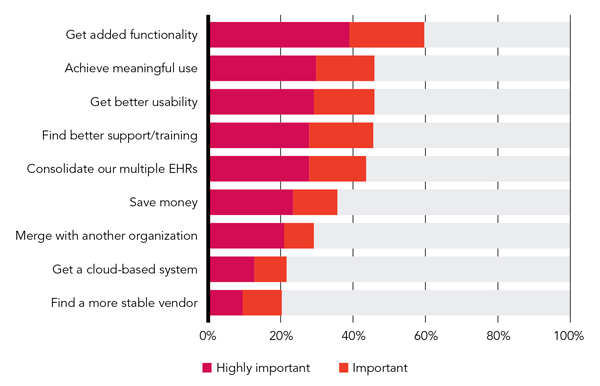
We asked respondents to rate the importance of eight factors in their practices' decisions to change EHR systems. The most common reason for changing EHRs was to add needed functionality. This was the only reason deemed important or highly important by more than 50 percent of respondents. The inability to achieve the Centers for Medicare & Medicaid Services' meaningful use requirements, poor usability, poor vendor support and training, and the desire to get everyone in a health system on the same EHR were the next most common reasons for making the change. (See “Reasons for the switch.”) A number of respondents added comments indicating that the change was not something they had requested but rather was forced on them, sometimes more than once, by their practice administration:
“Administration of the big system mandated we change from NextGen to Allscripts, and in two months we will be moving to Athena, mandated by … the giant mothership we are owned by now,”
“We were forced to [change EHRs] as part of the larger organization. Decision to switch was made at executive level,”
“[It was a] business decision by hospital owner attracted to the product's billing and financial reporting, not driven by clinical users' interests.”
REASONS FOR THE SWITCH
How hard was the change?
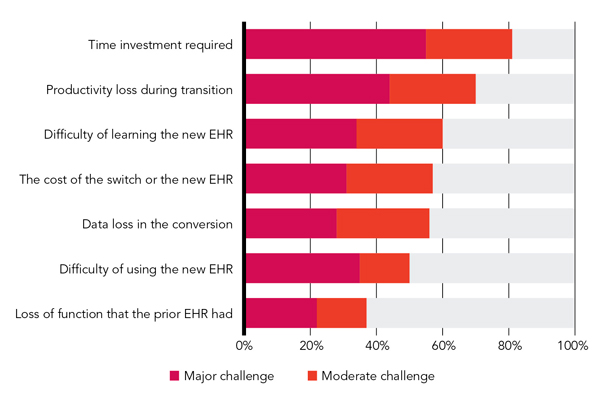
As you might expect, respondents found the process of changing EHR systems to be less than easy. Asked to rate a variety of potential challenges, 81 percent of respondents called the time investment required a moderate or major challenge. Similarly, and unsurprisingly, 70 percent rated productivity loss during the transition a moderate or major challenge. Other challenge ratings are depicted in “Challenges encountered in the process.” While data loss in the conversion was only the fifth most significant challenge according to the ratings, it was still considered a moderate or major challenge by 56 percent of respondents, and it was mentioned by more respondents than any other challenge in separate verbatim comments such as these:
“Data migration is an absolute joke. Old data doesn't import well into the new EMR.”
“Basically [we] lost the last two years' records except each hand-entered item.”
“We now have two sets of data. Old data would not transfer over, so it has to be reentered by the physician at time of visit.”
One respondent went so far as to advise, “Don't even bother with data migration. Just save an archived, read-only version of your old EMR. Migration is almost always a disaster.”
CHALLENGES ENCOUNTERED IN THE PROCESS
Was the change worthwhile?
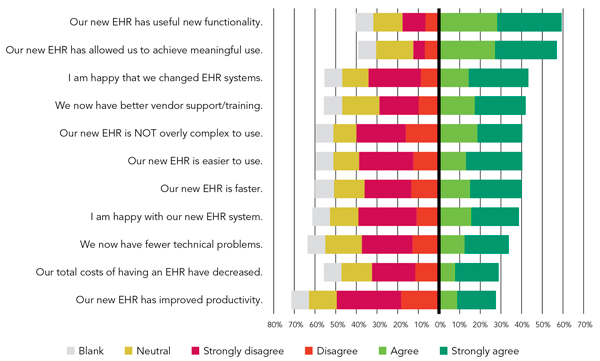
Given the difficulty and expense of changing EHR systems, one would hope that it makes life better. And indeed, 59 percent of respondents agreed or strongly agreed that their new EHRs have useful new functionality and 57 percent agreed or strongly agreed that their new systems allow them to achieve meaningful use – the two highest rated reasons for switching, as we saw above. But the rest of the picture is not exactly rosy. (See “Respondents' opinions about having changed EHR systems.”) Only 43 percent agreed or strongly agreed that they are happy they changed EHR systems, 42 percent say they have better support and training, 41 percent consider their new EHR “NOT overly complex to use,” and only 39 percent are happy with their new EHR. On this last point, it seems worthwhile to note that two systems, Praxis and Amazing Charts, had zero negative responses to the statement, “I am happy with our new EHR system.” (See “Agreement with the statement ‘I am happy with our new EHR system.’”)
RESPONDENTS' OPINIONS ABOUT HAVING CHANGED EHR SYSTEMS
AGREEMENT WITH THE STATEMENT “I AM HAPPY WITH OUR NEW EHR SYSTEM”
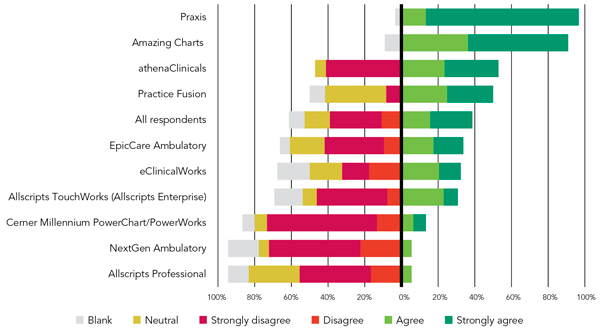
As we have seen in an analysis of our previous survey data,3 those who were personally involved in making the switch tend to look more favorably on their new system. Of the 140 respondents who said they were involved in the decision to change systems, 61 percent are happy with their new EHR; of those not involved in the decision, only 19 percent are happy with their new EHR. Given that, it's not surprising that 71 percent of solo physicians and 51 percent of respondents from two- and three-physician practices are happy with their new EHRs, as compared with no more than 32 percent of physicians in larger practices.
What can we conclude?
First, our data suggest that the EHR market is consolidating, that a number of practices are gravitating toward Epic (mostly large, hospital-owned practices, according to our full data), and that EHR changes haven't been particularly satisfying for physicians. Those who don't participate in the change decision and process tend to be less satisfied with the results.
Although the most common reason to change EHRs is to add needed functionality that was missing, many other factors are at play. Meaningful use and the perceived inadequacies of vendors and their software usability clearly play significant roles. In addition, many physicians are changing EHR systems not of their own volition but because their employers or new ownership have mandated the change, usually to provide system-wide integration.
Changing EHR systems is a major endeavor that typically requires large time investments from both users and management and occasions lost productivity, the challenge of learning a new EHR, and significant costs. It can also mean a step backwards, at least temporarily, if significant amounts of data cannot be converted electronically. As one respondent noted, “Plan for a slow down and major shake up for the first three to four months. Prepare yourself as if you are implementing an EHR for the first time. It is just as disruptive.”
Does making a switch improve things? It does appear to help add useful functionality and to help users achieve meaningful use. It doesn't, however, appear to make them happier or to lead consistently to better overall EHR performance. Users were about equally split on whether they had better usability and speed, lower costs, and fewer technical glitches with their new EHR than with their old one. They were also equally split on whether they were happy with the new EHR. Disturbingly, more users disagreed that their new EHR improved productivity than agreed (49 percent vs. 28 percent). One could attribute this to the learning curve of a new EHR, but something else may be going on, because 62 percent of respondents had made their switch more than a year earlier.
So if your current EHR just cannot incorporate functionality you need or get you to meaningful use, it may be time to switch to a new EHR. On the other hand, if you just want to change because you don't like using your current EHR or consider it a drag on your productivity, the grass may not be greener on the other side. Proceed carefully. The issue may be universal to EHRs, or it may be related to how you are using the EHR rather than the software itself. Be sure to do careful analyses of your current problematic workflows (i.e., who does what and when). Changing those workflows, rather than the software, may lead to a satisfactory (and easier) solution in many cases.
We'll give the last word to one survey respondent who advised those thinking about switching EHRs to approach the endeavor with realistic expectations: “Expect getting a new EHR to be like getting intensive chemotherapy for a minimally responsive malignancy: A few are better off, but the process is very traumatizing.”
