As virtual visits become more popular, physicians should consider their value and what it would take to provide them.
Fam Pract Manag. 2015;22(4):16-20
Author disclosure: Dr. Kaibara holds a less than 1-percent share in MeMD.

Not long ago, virtual visits were considered the stuff of science fiction. Today, if you type the search term “online doctor” into your Internet browser, you will get more than 700,000 results. Patients can use a computer to purchase a prescription drug, have a skin lesion diagnosed, or get a second opinion on an MRI – services that once required a visit to the doctor's office. This virtual marketplace is expected to grow exponentially and serve more than 7 million patients in the United States by 2018.1
Much of the virtual care provided today is through private companies, which could eventually erode the services traditionally furnished face-to-face in primary care. But if primary care offices offered virtual visits, they could take part in this business while protecting continuity of care, quality, and patient satisfaction. As such, primary care physicians may want to consider offering virtual visits. (See “Checklist for getting started with virtual visits.”)
In addition, physicians are likely to be solicited about buying a virtual visit system or working for a virtual visit company and should be aware of the technological, financial, and medicolegal considerations. This article provides a lay of the land to help physicians understand this evolving industry.
CHECKLIST FOR GETTING STARTED WITH VIRTUAL VISITS
Investigate any restrictions on virtual visits by your state medical board.
Investigate malpractice coverage for virtual care.
Identify what services you will offer virtually.
Investigate virtual visit technology/vendors.
Understand private payer and Medicare reimbursement.
Set prices for cash-paying patients. Survey patients to identify an effective price point, if needed.
Ensure HIPAA compliance. See the U.S. Department of Health & Human Services guidance.
Draft policies for virtual prescribing, appropriate visit categories, informed consent, etc.
Market the service to patients, making it clear that virtual visits are not for urgent matters.
What are virtual visits?
Many people confuse virtual visits with telemedicine and portal visits, but there are some key differences:
Telemedicine involves telecommunication between two medical facilities. The patient and a facilitator are in one facility (the “originating site”), and the treating provider or provider team is in the other facility (the “distant site”). In the originating site, most medical devices – from stethoscopes to advanced intensive care monitoring equipment – are connected directly to a computer in the distant site, which can be expensive.
Portal visits are similar to virtual visits but not as interactive because they do not take place in real time. Instead, the patient submits his or her information via a secure electronic portal, and a physician reviews it and replies electronically within a set timeframe, usually 24 or 48 hours. Many electronic health record (EHR) systems offer a basic patient portal but do not offer real-time communication, although they will likely evolve to include this in the future.
Virtual visits allow the patient to access care via a web-cam without using a facilitator or going to a facility. Generally, a patient goes to the provider's website, requests a visit via an online scheduling system, and then pays a set price online to see the doctor. Most sites require the patient to enter a short medical history and allow attachments (medical records, a blood pressure log, an image of a suspicious mole, etc.). The patient is then connected to a physician who reviews the information and communicates with the patient in real time via webcam. Diagnostic tools are generally limited to those the patient owns, such as a home thermometer or blood pressure cuff. At the conclusion of the visit, the patient receives a secure link to an electronic record of diagnosis, treatment, any e-prescriptions, and discharge instructions.
In most cases, physicians provide virtual visits by signing up with a service – either a virtual visit service offered by one of their insurance companies or a private virtual visit company. Some of these companies may offer their platforms to private offices at fixed or per-patient rates. Additionally, HIPAA-compliant products are available with a large range of costs, from a webcam that can be used while documenting in an existing EHR system to all-in-one technologies that provide a webcam as well as documentation technology and support. However, these systems require assembly. This can be difficult for many physicians, akin to trying to assemble an EHR.
The value of virtual visits
Research has shown that patients like the convenience of receiving care virtually.2 Additionally, many patients believe that the potential value of using technology to improve their health care is greater than the potential risk to privacy.3 Initial data indicates that virtual visits improve access to care, in part by lowering the cost of care.4 Virtual visit fees are usually less than $100, although many are less than $50. Initial evidence also suggests that home-based telehealth positively affects clinical outcomes.5,6
Although virtual visits are most often used by young, healthy, tech-savvy, and well-off patients, data shows that elderly, chronically ill, and underserved populations are likely to adopt the technology as it becomes more user friendly and reliable.7
For physicians and medical staff, virtual visits expand the opportunity to connect with patients. In particular, virtual visits could be a helpful way to manage the expanding responsibilities placed on primary care, such as engaging patients in shared decision making, managing patients with chronic conditions, and keeping patients out of the hospital. These tasks can be difficult to execute solely through episodic office visits during office hours.
Key considerations
Because virtual medicine is an evolving area, physicians looking to add it to their practices should not presume anything. For example, the practice of virtual medicine is not yet a standard inclusion in all medical malpractice policies; supplemental coverage or riders are often required. Also, even though virtual care is borderless, most states currently require physician licensure to treat patients residing in the state, with exceptions generally made only for teleradiology. However, there is potential for this barrier to disappear in the near future. Five states have adopted a national medical licensure compact agreement for all physicians, and it is pending in many others.8
Medical board laws and policy are another gray area. Most regulations were written to address the in-person practice of medicine – language that is difficult to extrapolate to virtual care. To encourage a uniform and safe adoption of virtual care, the Federation of State Medical Boards recently published a model telemedicine policy that is relevant to virtual visits as well.9 State medical boards are free to adopt the model policy or amend it as necessary. A key point of the policy is that virtual medicine should be held to the same standard of care as ambulatory medicine. Both should include formation of a doctor-patient relationship, proper evaluation and treatment, responsible prescribing practices, protection of the patient, and safeguarding patient privacy. Each of these widely accepted elements of care has implications for virtual visits:
Formation of a doctor-patient relationship. The safest practice would be to provide virtual visits only to established patients. Knowing their background can make it easier to treat patients virtually or to redirect them to a face-to-face office visit if needed. In fact, some states may require physicians to form a relationship with the patient through a physical examination before a virtual visit is allowed.
Proper evaluation and treatment. To properly evaluate and treat patients, physicians will have to consider what conditions are and are not amenable to virtual treatment. This must then be communicated with patients in advance so that the patient will seek an appropriate treatment venue and not delay care. In deciding what problems to treat virtually, physicians must consider what exam elements can be performed virtually, such as the patient taking his or her own temperature.
Below are some common uses for virtual visits:
To refill medications for patients with stable chronic conditions (such as diabetes, renal failure, congestive heart failure, or chronic obstructive pulmonary disease), assess medication compliance, or address other routine issues that do not require a face-to-face physical examination. Office visits could then be used to address preventive care and interventions that alter disease progression.
To provide brief intensive counseling or self-management support for patients with conditions such as obesity or smoking. Brief counseling is the perfect use of virtual care because it is primarily a verbal rather than physical interaction, and the webcam allows for connection through eye contact and facial expressions. In addition, virtual communication can help reduce logistical barriers to communicating regularly in person.
To treat conditions where an office visit is not imperative and empiric therapy is reasonable, such as the treatment of urinary tract infection in symptomatic but otherwise healthy premenopausal, nonpregnant women.10 In a recent comparison of 8,000 virtual visit and in-person doctors' visits for urinary tract and sinus infections, less than 7 percent of patients in either group returned for a consultation within three weeks, and the virtual platform did not have higher rates of misdiagnosis or treatment failure than traditional visits.11
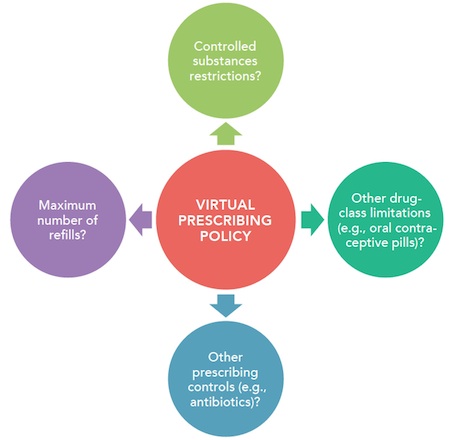
Responsible prescribing. Virtual prescribing should include limitations and be governed by a prescribing policy. Many private telehealth companies have policies against prescribing drugs that have abuse potential or important side effects to follow over time, such as controlled substances, weight-loss medications, erectile dysfunction drugs, and antidepressants. Virtual prescription policies may differ for primary care offices because patients are known to the physician and can be followed. (See “Prescribing policy considerations.”)
PRESCRIBING POLICY CONSIDERATIONS
Primary care offices should consider creating a more restrictive prescribing policy for virtual visits. Four key questions to consider are illustrated below:
Protection of the patient. This begins with having adequate malpractice insurance that covers virtual visits, as discussed earlier. In addition, virtual visits should include informed consent, specifically a discussion of the usual risks, benefits, and alternatives of treatment as well as the unique limitations of virtual care. For example, a physician instructing a patient virtually to use supportive care for a probable viral upper respiratory tract infection should make the patient aware that an in-person evaluation might include rapid streptococcal testing or a chest X-ray.
Safeguarding patient privacy. HIPAA physical standards require that patient care be conducted in a private area. This is simple to achieve in an examination room. The virtual visit must be afforded the same amount of privacy so that it is not possible for another party to view the screen or overhear a patient encounter. Further, HIPAA technical rules determine minimum security software requirements in health care. Many popular consumer products such as Skype and Face-time are appealing because patients are familiar with them and no additional software is required. However, at this time, while many of these commercial products encrypt or otherwise secure their services, they do not explicitly state that they are HIPAA compliant. Further, HIPAA requires physicians to enter into a business associate agreement with covered service entities to appropriately safeguard protected health information. Physicians partnering with a virtual visit company or purchasing commercial telemedicine software products would, of course, need to ensure that all products they use are HIPAA compliant.
Reimbursement
Most virtual visit services currently require cash payment directly from the patient at the time of the service. As noted earlier, the price is often about $50 per visit. If a physician provided just one virtual visit per day at this rate, the resulting gross revenue would be about $12,000 per year, with very little time invested and almost no visit costs outside of the physician and the technology itself.
As evidence grows to support the cost-effectiveness of virtual visits, third-party reimbursement is expanding. The 2015 Medicare Physician Fee Schedule expanded the services that can be furnished to patients as part of the Medicare telehealth benefit to include prolonged evaluation and management services in the outpatient setting, the annual wellness visit, psychotherapy, and psychoanalysis. Medicaid generally will pay for virtual visits as well.
Most major insurers are at least piloting virtual visits in select markets. Some insurers are offering them more broadly, such as United Healthcare, which recently launched a national ad campaign highlighting its virtual visit benefit. Reimbursement is variable, however, and will need to be confirmed with local payers. Several private insurers have partnered directly with virtual visit companies as an adjunct service, similar to 24-hour nurse telephone hotlines. Further, some employers have elected to offer virtual visit services separate from the employer-sponsored health plan to reduce overall health care costs.
Other fee options to consider are offering virtual visits via a cash-pay service for uninsured patients or as part of a concierge practice.
A disruptive innovation
Although it is difficult to envision the future of medicine, it is clear that virtual care will challenge how primary care is traditionally delivered. In 1897, when the first case of croup diagnosed via telephone was published, many physicians did not accept the practice as medically sound.12 Now, doctors field an average of more than 100 calls per week, many of which address clinical problems or involve prescriptions. Virtual medicine could be the modern-day telephone call and, as such, is worthy of early consideration by primary care physicians.
RELATED RESOURCES
This nonprofit organization provides resources for the latest legislative action in telemedicine, offers information on malpractice insurance and model standards, and offers an accreditation program for online patient consultations.
The center offers resources on state licensure and reimbursement law organized by state as well as resources outlining Medicare and Medicaid reimbursement for telehealth.
RELATED ARTICLES FROM FAMILY PRACTICE MANAGEMENT
Making a case for online physician-patient communication. Adler KG. Fam Pract Manag. 2008;15(5):A3–A6. .
Removing six key barriers to online portal use. Twiddy D. Fam Pract Manag. 2015;22(1):26–31. .
Secure messaging: myths, facts, and pitfalls. Franklin R. Fam Pract Manag. 2013;20(1):21–24. .
Virtual office visits: a reachable and reimbursable innovation. Eads M. Fam Pract Manag. 2007;14(9):20–22. .