
A systematic approach that follows these seven principles can help you translate patient feedback into improved service.
Fam Pract Manag. 2016;23(3):15-19
Author disclosures: no relevant financial affiliations disclosed.
Patient satisfaction scores are increasingly affecting reimbursement for medical care as value-based purchasing becomes more prevalent. Succeeding in this payment model requires physicians and their organizations to first understand how patients judge service quality and then to take a systematic approach to using patient feedback to improve service.
All customers form opinions about service quality by comparing their preservice expectations to their actual experience and assessing the result.1 If an experience meets or exceeds expectations, the customer perceives good service. If an experience falls short of expectations, creating a “customer gap,” the customer perceives poor service. Most patients lack the technical knowledge to judge the quality of their medical care, so when asked on a survey to rate “overall quality of care,” they often reflect on the service experience. With every interaction, patients form opinions about quality based on staff empathy, service attitude, and friendliness, as well as provider communication skills and practice efficiency. There is no better way to evaluate the impact of service quality on the care experience than to ask our patients.
In this article, we share Mayo Clinic Arizona's (MCA's) seven-prong model for improving service quality,2 as well as several tools we used and lessons we learned implementing the model in our family medicine practice.
The general principles and advice can be adapted to suit medical practices of any size. (See “Challenges and advantages for small practices.”)
CHALLENGES AND ADVANTAGES FOR SMALL PRACTICES
The basic tenets of this model for improving service and satisfaction apply to practices of all sizes; however, the implementation may look different for small practices. For example, most small practices do not have a staff member whose primary role and expertise is leading service improvement. Instead, they may need to tap the service passions of an existing employee, perhaps a practice manager or someone with prior customer service or teaching experience who could help improve service. This person should be somewhat analytical, have good communication skills, and be knowledgeable about how the practice operates.
Similarly, small practices are not likely to have the data measurement and analysis capabilities of a large organization, so they may need to contract with a consultant or perhaps a local university to obtain those services.
Although small practices certainly have unique challenges when it comes to improving service, it should be noted that they also have unique advantages. For example, quicker decision-making capabilities, less bureaucracy, smaller patient populations, and greater transparency may make it easier to identify, buy into, and act on improvements.
The seven principles
Our model for improving service quality incorporates seven widely accepted principles:
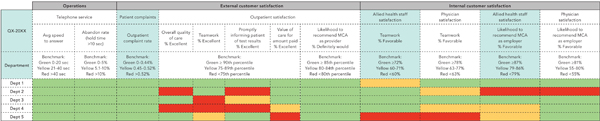
1. Use multiple data sources to drive improvement. A data-driven approach is crucial to improving service quality, so our first step was to obtain valid patient satisfaction survey data. (See “Surveys, vendors, and costs.”) The service dimensions we measured, such as “thoroughness of the medical exam,” “listening to patient concerns,” and “showing courtesy and caring,” are similar to those on the Clinician and Group Consumer Assessment of Healthcare Providers and Systems (CG-CAHPS) survey. To provide additional perspectives, we also looked at employee satisfaction data, call center metrics, and customer complaint rates – data that previously had been held closely by source report owners. We compiled the data in a single dashboard (see “Outpatient service dashboard”) so, at a glance, we could see how each department, and the organization overall, was doing.
SURVEYS, VENDORS, AND COSTS
Mayo Clinic Arizona contracts with a national patient satisfaction survey vendor that fields a 50-item telephone survey to a random sample of patients. Patients use a five-point scale (excellent, very good, good, fair, or poor) to rate our service quality related to the provider (physicians and midlevel providers), the allied health staff (nurses, technicians, and nonclinical staff), the facility, and global attributes, such as overall quality and likelihood to recommend.
The federally approved CG-CAHPS survey is rapidly becoming a part of how providers are paid. The CAHPS website provides the files needed to conduct the survey and analyze the data. CMS-approved vendors can be found online as well.
CG-CAHPS survey costs vary depending on the vendor and how the survey is administered. One report estimated the cost per completed survey to range from $7 for mail administration to $11 for telephone administration.1 Assuming 45 completed surveys per provider, the minimum requirement according to the report, the cost would be $315 to $495.
We monitor the dashboard and review it regularly with providers and allied health staff. We also have custom patient satisfaction reports automatically emailed quarterly from our survey vendor's online system to help keep relevant data in front of providers and other staff. These reports allow us to look at both individual and group performance.
OUTPATIENT SERVICE DASHBOARD
Our outpatient service dashboard compiles service-related metrics from multiple source reports. Being able to visually scan multiple metrics for each department, instead of viewing them in isolation, gives a more complete picture of service quality. The dashboard shown here displays the current quarter's data, but we also track trend data from previous quarters. Some benchmarks are based on mean performance, while others are based on industry standards or leadership targets.
2. Define clear lines of accountability for service quality. We want every employee in our organization to be engaged in service quality improvement. Therefore, every provider and staff member is held responsible for delivering excellent service. For example, the department chair has access to provider-specific data and discusses it with the provider during performance reviews. The emphasis is on personal improvement, not punishment. (See “Provider improvement summary.”) When provider data are shared at the department or organization level, they are blinded to emphasize team accountability.
Provider improvement summary
The sample report shown below summarizes baseline patient perceptions of provider-specific behaviors during the clinical encounter and improvements two years later. The data represent an individual provider, but we can also view the data for all providers combined.
| Provider-specific survey questions | Baseline % Excellent | Two years later % Excellent | Percent change | P value |
|---|---|---|---|---|
| Thoroughness of medical exam | 62 | 70 | 8 | 0.04 |
| Spending enough time with patient | 69 | 74 | 5 | NS |
| Listening to patient concerns | 67 | 75 | 8 | 0.04 |
| Using understandable words and terms | 70 | 77 | 7 | NS |
| Explaining medical condition | 65 | 73 | 8 | 0.04 |
| Involving patient in decisions about care | 65 | 72 | 7 | NS |
| Showing courtesy and caring | 74 | 80 | 6 | NS |
| Perception of overall quality of care | 69 | 79 | 10 | 0.01 |
| Patient comments obtained from the satisfaction survey | "I liked the interaction with the physician." "I liked the doctor's explanation of my problem." | "Our primary care doctor has always take the time to answer our questions and has never made us feel rushed. Thank you for the excellent care." "He seems like he has nothing else to do besides talk to me and answer questions." "The doctor is personable, caring, knowledgeable ... makes you feel like you are the only one." "I think the communication with the doctor was much improved over the typical care here." | ||
Because providers and staff are accountable, it was important to involve them in improvement activities from the beginning. After all, front line employees who serve patients every day often have the best understanding of where service breaks down and how to fix it. We encouraged staff to identify improvement opportunities and help design small changes to practice workflows. To help the team assess the impact of changes, receptionists gave short, point-of-service surveys to patients at checkout. Post-improvement data were then displayed in work areas to hold team members accountable to one another and to encourage staff ownership of their part of the patient experience.
Recognizing that providers are strong influencers of the patient experience, we gave them the satisfaction survey questions upfront so they would feel more confident in the process and know which aspects of service patients were being asked to rate. They also received their patient satisfaction survey data and comments quarterly.
3. Provide service consultation and improvement tools. Without careful analysis, patient satisfaction survey data can be misinterpreted and misused. To prevent this, the patient experience leader in our organization partnered with us to provide objective data analysis. She also provided service quality audits, education and training, improvement tools, and other consultative services. She essentially functioned as an internal consultant, aligned with but not reporting to practice leadership in order to maintain independence and objectivity.
4. Define service values and performance standards. Key leaders and staff defined the service values for our organization, which were introduced at staff meetings and displayed in work areas and break rooms. These values use the mnemonic “SERVE”:
Solutions-focused: Solve problems when and where they occur,
Empathetic: Treat everyone as you wish you or your family to be treated,
Reliable: Own the work; if you don't have the answer, find it,
Valuing others: Protect patient and employee confidentiality,
Exceed patient expectations: Contribute to an unparalleled experience.
Staff then developed their own role-specific service performance standards (e.g., “We answer telephone calls in three rings with a consistent greeting” or “We listen to patients without interrupting them”). Leveraging the staff's knowledge of their jobs in developing these standards encouraged their buy-in.
A key performance standard for providers is the number of patients assigned to them. From the providers' perspective, panel size and makeup can significantly impact service quality and patient satisfaction. One particular patient comment – “I feel that [my doctor] has too many patients, which does not give her enough time to follow-up with patients in a reasonable amount of time” – drove us to reevaluate the number of patients each provider was caring for and take a more team-based approach. The new Mayo Model of Community Care partners two physicians with four advanced midlevel providers (nurse practitioners and physician assistants), which we have found to be a more efficient use of resources. This model also enhances job satisfaction by allowing all providers to practice at the top of their licenses.
5. Provide service education and training to providers and allied health staff. Rather than providing general service education, we tried to customize it based on the family medicine practice's needs, identified through their data and service performance standards. We covered topics such as satisfaction surveying basics, handling and recovering from common service complaints, and how staff behaviors influence patients' perceptions of overall quality. All staff, including physicians and administrative leaders, participated in service education.
We offered individual education and training as well. For example, to address some interpersonal challenges identified through patient feedback, one provider requested a personal coach, who observed his interactions with patients and offered constructive feedback.
6. Continuously monitor and improve service quality. In addition to our ongoing monitoring of data, we also conduct periodic “secret assessments” of service performance. For example, a practice administrator or a nurse might call or walk through the practice experiencing things as a patient would. Interestingly, the nursing staff's assessments of their peers tended to be more critical than the practice administrator's and led nursing staff to create new service performance standards.
Monitoring our performance data pointed us to simple changes we could make. For example, repeated feedback from patients indicated that a 15-minute visit didn't give them enough time to address all of their needs. This led us to develop a simple form that asks patients to list the top three questions or issues they would like to cover during their visit and whether they have any medications that need to be refilled or any forms that need to be completed.3 (You can download a similar form from the FPM archives.) We send this form to each patient with the previsit paperwork, and the provider reviews the completed form before entering the exam room. Asking patients to identify their top three problems has helped us set more realistic patient expectations about appointment length, minimize the “customer gap,” and improve satisfaction. One provider even commented that use of the form has led to more focused office visits, getting the patient and provider on the same page regarding what is most important to the patient.
7. Recognize and reward excellent service. Our organization holds annual events to recognize departments and individuals who achieve exceptional performance. Two years after implementing this model, our family medicine practice was recognized with its first “five-star” award for exceeding the 90th percentile goal for patient perception of overall quality.
Other forms of recognition include “thank-you grams,” which staff use to express gratitude to colleagues. We display all thank-you grams on a recognition board to support the service culture and teamwork. In addition, we email positive patient comments to all staff and award movie tickets to employees specifically named by patients for providing excellent service.
Lessons learned
Our journey to improve family medicine service quality has taught us the following lessons:
Take a comprehensive approach to service improvement. Don't be tempted to implement quick fixes or flavor-of-the-month service programs. They don't stick and don't improve the patient experience or the service culture. Improving behaviors and processes that move the metrics is best achieved when you systematically apply all seven service quality principles.4
Be vigilant. Creating a culture in which all staff feel a sense of ownership of the patient experience requires the constant vigilance of the practice administrator or another practice leader. This person must help communicate performance standards, observe service performance, provide timely feedback, and mentor front-line staff. Staying vigilant is easier if you believe that what you're doing makes a difference. For example, a patient of ours commented that “The Mayo culture inherent within your staff provides for a calm and caring environment for patients like me. I'm such a sissy … It is great to have people like you to help me when I visit.” This reminded our staff of the impact of their service behaviors and to never underestimate the power of a warm smile or a gentle touch.
Get executive leadership's endorsement and visible support. Physicians and other practice leaders must demonstrate a genuine commitment to service excellence. Our chief executive officer sets the tone with visible support of service quality leadership and improvement. One important lesson we learned is that Human Resources must be involved in the process. There may be disgruntled employees who, when being held to service performance standards, are unwilling or unable to adapt and change their behaviors to provide patients with better service.
Be transparent. Share satisfaction survey questions, patient ratings, and comments with all front-line staff and providers, as they help create the patient experience.
Keep your promises. Review the messages in your marketing materials, including brochures, radio or print advertisements, your website, and your patient portal. Can your practice keep the implied and explicit promises, or are patients' expectations elevated to such a level that your practice would be challenged to meet them? It's possible that your practice's marketing messages contribute to the “customer gap” and patient dissatisfaction. For example, if your marketing materials promise state-of-the-art medical care but your office space looks run down and outdated, that could create a gap between patients' expectations and experiences.
Great expectations
As patients pay more out of their own pockets for health care, they will have higher service expectations, be less tolerant of poor service, and more quickly leave practices that don't satisfy their needs. It is not enough to simply remodel a facility; practices must actually improve service quality. Doing so requires a comprehensive approach, a systematic method for collecting and acting on patient satisfaction data, and a culture of accountability. Improving service is the right thing to do for the patient and, in a value-based payment model, may help to sustain a practice into the future.
