
You're likely already doing the work, so why not get paid for it?
Fam Pract Manag. 2016;23(3):30-35
Author disclosure: no relevant financial affiliations disclosed.
In family medicine practices today, coding drives revenue. Even for employed physicians, coding drives compensation because it is a proxy for productivity. Although many practices are wisely preparing for value-based payment, physicians still need to optimize current revenue and compensation through correct coding. After all, 95 percent of all visits are still paid using fee for service.1
Unfortunately, many groups don't bother monitoring their coding patterns or optimizing their coding. They seem to believe that variation in levels of evaluation and management (E/M) service among physicians is unavoidable and beyond their control. It is not. Using a relatively simple but vital tool – a “CPT frequency report” – practices can identify coding patterns that result in lost revenue. (See “What is a CPT frequency report?”)
Differences in specialty and scope of practice result in some appropriate variation in E/M coding patterns. However, I recently reviewed the CPT frequency report of a multisite primary care group and found variation that had resulted in significant differences in their work relative value units (RVUs) per encounter and total revenue.
This article draws on that analysis to identify four often overlooked coding and revenue opportunities.
WHAT IS A CPT FREQUENCY REPORT?
A CPT frequency report, like the sample shown here, is simply a listing of all CPT codes billed by each physician for a given period, typically a year. The report lists the code, the code description, and the number of times it was billed. Physician leaders and managers can compile the report annually from the practice's billing system and get a snapshot of the group's coding patterns, without having to review individual charts and documentation. Although there will always be variation due to differences in practice patterns and patient populations, this tool can help reveal avoidable coding variances due to overcoding, undercoding, missed charges, or compliance issues.
For example, the report shows that Physician A reports code 99213 almost three times as often as code 99214, although the benchmark ratio is 1.08:1. There are no Medicare wellness visits or transitional care management services reported. There are no smoking cessation services or certification of home health services reported either. Nebulizer treatments are reported 16 times, but the medication for the nebulizer isn't billed. Influenza vaccinations are reported but no administration. New patient visits are billed at much higher levels than benchmarks.
Physician B has a ratio of 99213s to 99214s that is in line with the benchmark. This physician reports Medicare wellness visits and transitional care management services (both levels), as well as a few smoking cessation services. There are no home health certification services reported, however.
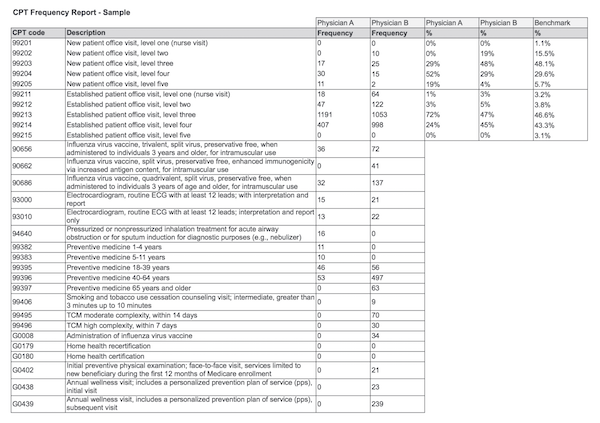
Benchmarks are derived from the Centers for Medicare & Medicaid Services, E/M Codes by Specialty. Available at: https://www.cms.gov/research-statistics-data-and-systems/statistics-trends-and-reports/medicarefeeforsvcpartsab/medicareutilizationforpartb
1. Bill for high-value services you've probably been providing for free
Three high-value services family physicians are likely providing but not always billing for are transitional care management, chronic care management, and advance care planning.
Transitional care management. This service involves seeing patients who are discharged from the hospital or another facility. It includes talking to the patient by phone, seeing the patient for an office visit after discharge, reconciling medications, reviewing the discharge summary, coordinating care, and providing patient and family support.
In the CPT frequency analysis referenced earlier, only 9 out of 26 physicians billed any transitional care management services during the year. One physician actually reported a number of discharge visits but not a single transitional care management service. Without reviewing individual records, it's impossible to know how many of the group's patients were eligible for transitional care management, but it is safe to assume that all physicians had provided the service at some point over the year. In many cases, they likely billed these services as an office visit (e.g., CPT code 99214) instead of a transitional care management service (e.g., CPT code 99495). The difference between the two codes is 0.6 work RVUs or approximately $57.32. (See “RVU and payment comparisons.”)
RVU AND PAYMENT COMPARISONS
The table below demonstrates the RVUs and payment allowances for services commonly provided by family physicians. Payment amounts shown here are not geographically adjusted.
Every CPT code is assigned relative value units (RVUs) that help determine payment and reflect the following:
The level of physician work (the physician's time, skill, training, and intensity required),
Practice expenses (rent, staffing, equipment, and supplies for either “non-facility” settings such as free-standing physician offices or “facility” settings such as inpatient settings or hospital outpatient clinics),
Professional liability (the physician's malpractice expense).
Total RVUs are then multiplied by a conversion factor set by Congress (currently $35.804) to determine the national payment rate. A geographic adjustment is applied to determine local payment rates. To look up local rates, use the Physician Fee Schedule Search.
| Code | Work RVUs | Total facility RVUs | Total non-facility RVUs | National payment amount, non-facility |
|---|---|---|---|---|
| E/M visits | ||||
| 99214, Established-patient office visit | 1.5 | 2.21 | 3.02 | $108.20 |
| 99215, Established-patient office visit | 2.11 | 3.13 | 4.7 | $168.39 |
| Transitional care management | ||||
| 99495, Moderate complexity TCM | 2.11 | 3.11 | 4.62 | $165.52 |
| 99496, High complexity TCM | 3.05 | 4.50 | 6.51 | $233.24 |
| Medicare wellness visits | ||||
| G0402, Welcome to Medicare visit (without ECG) | 2.43 | 3.58 | 4.68 | $167.67 |
| G0438, Initial annual wellness visit | 2.43 | 4.82 | 4.82 | $172.69 |
| G0439, Subsequent annual wellness visit | 1.50 | 3.27 | 3.27 | $117.16 |
One physician in the analysis managed to report transitional care management services but recorded all of them at the highest level. This is not likely accurate and could pose a compliance problem. The Centers for Medicare & Medicaid Services (CMS) has stated in the past that a more expected ratio for transitional care management services is three moderate complexity visits for every one high complexity visit.
The requirements for code 99495 are as follows:
Communication (direct contact, telephone, or electronic) with the patient or caregiver within two business days of discharge,
Medical decision making of at least moderate complexity during the service period,
A face-to-face visit within 14 days of discharge.
The requirements for code 99496 are as follows:
Communication (direct contact, telephone, or electronic) with the patient or caregiver within two business days of discharge,
Medical decision making of high complexity during the service period,
A face-to-face visit within seven days of discharge.
Much of the work of transitional care management is done by clinical staff supervised by the physician. A staff member calls the patient within two business days of discharge, opens the template on the day of the face-to-face visit, and provides coordination or educational services as directed by the physician. By capturing these codes, the physician is awarded additional work RVUs for the direction and oversight, and the practice is paid for work it previously did for free or for a lesser rate. Note that CMS now allows the physician to bill the transitional care management code on the day of the face-to-face visit, rather than waiting until 30 days after the discharge. This change should make billing for this service even easier.
Chronic care management. At the time of the group's CPT frequency analysis, chronic care management codes (and advance care planning codes) had not yet been released, so they did not factor into the analysis. Nevertheless, they represent clear coding and payment opportunities for family physicians.
Chronic care management applies to patients who have multiple (two or more) chronic conditions expected to last at least 12 months, or until the patient's death, that place the patient at significant risk of death, acute exacerbation/decompensation, or functional decline. There is a single code – 99490. The three key requirements for billing chronic care management are 1) having a scanned, signed patient agreement, 2) having a patient-centered care plan, and 3) having a monthly log showing at least 20 minutes of staff contact time. Staff are key to managing these tasks. (For downloadable tools to help you meet these requirements, see “Chronic Care Management and Other New CPT Codes,” FPM, January/February 2015.)
Advance care planning. This service is now reportable with two new codes:
99497, “Advance care planning including the explanation and discussion of advance directives such as standard forms (with completion of such forms, when performed), by the physician or other qualified health professional; first 30 minutes, face-to-face with the patient, family member(s), and/or surrogate,”
+99498, “each additional 30 minutes (list separately in addition to code for primary procedure).”
Providers can use these codes to report the face-to-face service even if the visit does not involve completing the relevant legal forms. The service can occur as a stand-alone visit or as part of an E/M visit. In the latter case, time spent on E/M services would not count toward time used for advance care planning. (For more on the advance care planning codes, see “Coding and Billing Rules in 2016: Out With the Old, In With the New,” FPM, January/February 2016.)
2. Perform wellness visits and, when appropriate, perform them with a problem-oriented visit on the same day
Many physicians I work with objected to the “Welcome to Medicare” visit (G0402-G0405) and annual wellness visits (G0438-G0439) when they were introduced many years ago, noting that these visits didn't require a physical exam. Physicians weren't prohibited from doing an exam, of course; the real issue was that they didn't see the value in the screening and health-risk-assessment tools required for the visit. Instead of incorporating the visits, many physicians continued to schedule only problem-oriented visits for Medicare patients and, at the end of one of those visits, would provide – free of charge – referrals for screenings and advice about immunizations. This resulted in lost revenue.
Practices that have successfully integrated wellness visits into their physicians' days rely on ancillary staff to collect the data needed for these visits. The patient can often fill out the required screening tool, or a staff member can collect the data. The family physician can then provide the personalized advice.
In the CPT frequency analysis referenced in this article, 10 of the 26 clinicians didn't report any wellness visits. Of the clinicians who did report wellness visits, the volume varied from 62 visits to 452 visits in a year. In place of wellness visits, they coded established patient visits, usually a 99214. The difference in work RVUs between a level-four established patient visit (99214) and an initial annual wellness visit (G0438) is 0.93; the revenue difference, based on national amounts, is $64.49.
Most Medicare patients have chronic problems to discuss at their wellness visits. CMS allows physicians to report both the problem-oriented visit and the wellness visit on the same day, and the revenue implications of reporting both services are significant. (See “The bottom line of billing a problem-oriented and wellness visit.”) Of course, the problem-oriented visit must be medically necessary, and both the wellness visit and the problem-oriented visit must be documented.
THE BOTTOM LINE OF BILLING A PROBLEM-ORIENTED AND WELLNESS VISIT
The following tables show the revenue potential of reporting a problem-oriented visit (such as a 99213 or 99214) along with a wellness visit (such as an initial or subsequent annual wellness visit) when both services are provided on the same day.
| Reporting both a 99213 and an initial annual wellness visit | ||
|---|---|---|
| Work RVUs | Non-facility payment | |
| 99213 | 0.97 | $73.45 |
| G0438 | 2.43 | $172.69 |
| Total | 3.4 | $246.14 |
| Reporting both a 99214 and an initial annual wellness visit | ||
|---|---|---|
| Work RVUs | Non-facility payment | |
| 99214 | 1.5 | $108.2 |
| G0438 | 2.43 | $172.69 |
| Total | 3.93 | $280.89 |
| Reporting both a 99213 and a subsequent annual wellness visit | ||
|---|---|---|
| Work RVUs | Non-facility payment | |
| 99213 | 0.97 | $73.45 |
| G0439 | 1.5 | $117.16 |
| Total | 2.47 | $190.61 |
| Reporting both a 99214 and a subsequent annual wellness visit | ||
|---|---|---|
| Work RVUs | Non-facility payment | |
| 99214 | 1.5 | $108.2 |
| G0439 | 1.5 | $117.16 |
| Total | 3 | $225.36 |
One of the billing requirements is that none of the documentation for the wellness visit can be used to select the level of service for the problem-oriented visit. To separate the documentation, physicians can either create two separate notes, which requires more work, or create one note for both services but clearly delineate the problem-oriented history, exam, and decision making from those of the preventive service. Because a wellness visit does not include the HPI, ROS, exam, or assessment/plan related to acute or chronic conditions, when those components are documented, it is a good indication that you should bill for both a problem-oriented visit and a wellness visit.
One group I know of has taken the opposite approach. It adds wellness visits to scheduled office visits. The coding and revenue are the same as adding a problem-oriented visit to a scheduled wellness visit, but the framework changes. The nurse and physician look at the day's schedule and identify Medicare patients scheduled for office visits for whom a wellness visit could be added. Of course, additional time may be needed for the risk assessment and counseling, but nurse practitioners or other staff can help with the wellness portion of the visit. The staff document the additional screenings related to the wellness visit, and the physician or other provider documents the problem-oriented visit and the personalized advice given based on the screening information documented by the staff. Since the wellness visit is covered entirely by Medicare, without a copay or deductible, the practice has had very few patient complaints with this method.
The work of the wellness visit is two-fold: 1) screening for depression, ability to perform activities of daily living, health risk assessment, and safety at home and 2) giving personalized advice based on the responses. All of the screening and data collection is staff work. Giving personalized advice is physician work, and most physicians are already doing this. Embracing and reporting these services supports physicians in achieving RVU and revenue goals without adding additional patient visits.
3. Identify missed ancillary charges and have a system for capturing them
By simply reviewing the CPT frequency report, even without looking at a single chart, the group was able to identify lost ancillary charges.
One of the more concerning issues was that only two of the 26 physicians in the group reported home health certifications (G0180) and recertifications (G0179) even though the process is simple. Keeping track of certifications and recertifications is another staff job. The physician develops the plan, answers the phone calls, writes the orders, and signs the certification. Staff can implement a billing process without additional burden to the physician. One key is for staff to copy the necessary forms for the biller, since they typically arrive by fax and are sent back that way. Implementing a system for this allows the physician to be paid for work already being done. A single home health certification is worth about $54.
Additionally, only four clinicians in the group billed for smoking cessation (G0436-G0437 or 99406-99407). Although the work RVUs and payment are small (about $14 for 3 minutes to 10 minutes of counseling), this represents work being given away for free. Any time spent on smoking cessation counseling should be documented and billed. If this service is billed with an E/M service on the same day, simply attaching modifier 25 to the E/M code will communicate that it is significant and separately identifiable from the tobacco cessation counseling.
The following discoveries also raised questions about missed charges or incorrectly posted charges:
Vaccines and medications were given without an administration code, which is always a billable service,
Nebulizer treatments were given, but medications weren't charged,
Finger-stick services were billed (although this is a bundled charge), but no lab test was reported,
Only half of the clinicians reported a single electrocardiogram in a year,
Amounts billed for CLIA-waived tests varied widely, from $221 to $5,341 per physician.
4. Pay attention to your 99213s and 99214s
Many physicians are tired of discussing the difference between a 99213 and a 99214. They have received conflicting messages from one coder to another, from electronic health record vendors, and from managers. But the frequency report for the primary care group showed that the variation between the 26 physicians, advanced practice nurses, and physician assistants was too large to ignore. For example, two physicians reported all new patient visits as level-four services, while other physicians rarely used the code.
Practices should review two key metrics. The first metric is the percentage of 99214 visits as a percentage of all established patient visits (99211-99215). The CMS benchmark is 43.3 percent for physicians.2 The other metric to track is the ratio between 99213 and 99214 visits. The CMS norm is 1.08.2 In other words, you should expect the ratio of 99213 visits to 99214 visits to be almost equal. If a physician is billing three, four, or five times as many 99213s as 99214s, or vice versa, do a chart review to determine whether the coding is accurate (not likely) or the physician needs some coding education.
For a quick refresher, according to Medicare's Documentation Guidelines for E/M Services, a 99213 code requires two out of three of the following:
Expanded problem-focused history (chief complaint, 1 to 3 elements of the HPI, and pertinent ROS),
Expanded problem-focused exam (6 to 11 elements),
Low-complexity medical decision making.
A 99214 code requires two out of three of the following:
Detailed history (chief complaint, 4 or more elements of the HPI or status of 3 or more chronic diseases, 2 to 9 elements of the ROS, and 1 element of the PFSH),
Detailed exam (12 or more elements),
Moderate-complexity medical decision making.
(For more on this topic, see “Coding ‘Routine’ Office Visits: 99213 or 99214?” FPM, September 2005.)
“No dollar left behind”
The medical director of an accountable care organization uses this phrase to remind family physicians that coding matters, even as the system is driving toward value-based payment. Physicians are naturally more interested in patient care and outcomes than CPT codes, but coding currently drives the lion's share of revenue in most family medicine practices. Coding produces revenue for the practice and, for employed physicians, determines RVU-based compensation. Until practices are paid solely for value and outcomes, coding will continue to matter greatly.
